Ann Rehabil Med.
2019 Jun;43(3):289-296. 10.5535/arm.2019.43.3.289.
The Role of Regular Physical Therapy on Spasticity in Children With Cerebral Palsy
- Affiliations
-
- 1Department of Rehabilitation Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea. byhong@catholic.ac.kr
- 2Department of Statistics, Sungkyunkwan University, Seoul, Korea.
- KMID: 2453918
- DOI: http://doi.org/10.5535/arm.2019.43.3.289
Abstract
OBJECTIVE
To investigate the effect of physical therapy (PT) intervention on spasticity in patients with cerebral palsy (CP), and to assess the degree of deterioration of spasticity when regular PT is interrupted in those patients.
METHODS
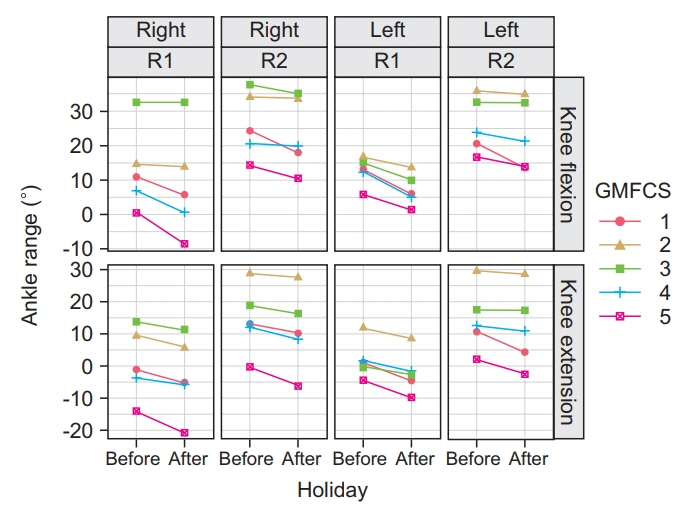
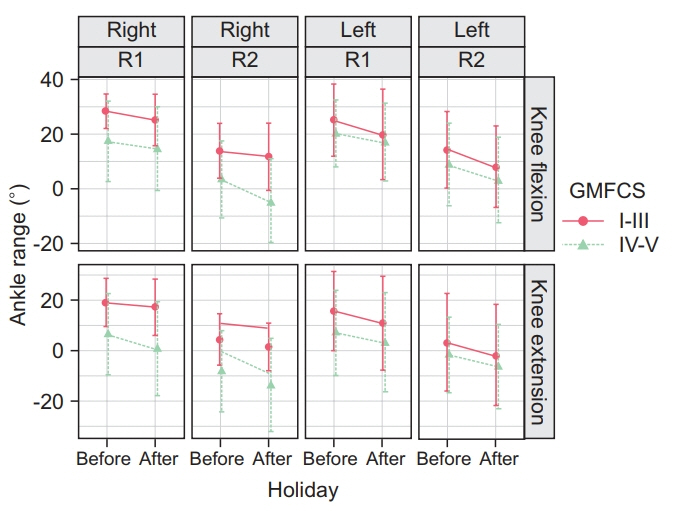
We recruited 35 children with spastic CP who visited our hospital for PT, and whose Modified Tardieu Scale (MTS) scores were serially recorded including before and after a 10-day public holiday time frame period. The outcome measures were the angle of range of motion (ROM) of dorsiflexion of the ankle joint (R1 and R2) in the knee flexion and extension positions as assessed using the MTS.
RESULTS
The range of dorsiflexion of the ankle joint (R1 and R2) after the holiday period was significantly decreased as compared with that measured ROM noted before the holiday period, regardless of the knee position, age, or gross motor function. The dynamic component of the MTS (R2-R1) showed a slight decrease in the knee flexion position.
CONCLUSION
Interruption of regular PT aggravated spasticity and decreased ankle joint ROM in children with spastic CP. Our findings suggest that regular PT in the care continuum for children with CP is crucial for the maintenance of ROM in the spastic ankle joints.
MeSH Terms
Figure
Reference
-
1. Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, et al. Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol. 2005; 47:571–6.
Article2. Surveillance of Cerebral Palsy in Europe. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol. 2000; 42:816–24.3. Westbom L, Rimstedt A, Nordmark E. Assessments of pain in children and adolescents with cerebral palsy: a retrospective population-based registry study. Dev Med Child Neurol. 2017; 59:858–63.
Article4. Yim SY, Yang CY, Park JH, Kim MY, Shin YB, Kang EY, et al. Korean Database of Cerebral Palsy: a report on characteristics of cerebral palsy in South Korea. Ann Rehabil Med. 2017; 41:638–49.
Article5. Scholtes VA, Becher JG, Beelen A, Lankhorst GJ. Clinical assessment of spasticity in children with cerebral palsy: a critical review of available instruments. Dev Med Child Neurol. 2006; 48:64–73.
Article6. Sees JP, Miller F. Overview of foot deformity management in children with cerebral palsy. J Child Orthop. 2013; 7:373–7.
Article7. Hagglund G, Lauge-Pedersen H, Wagner P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet Disord. 2007; 8:101.
Article8. Hagglund G, Wagner P. Development of spasticity with age in a total population of children with cerebral palsy. BMC Musculoskelet Disord. 2008; 9:150.
Article9. Chan G, Miller F. Assessment and treatment of children with cerebral palsy. Orthop Clin North Am. 2014; 45:313–25.
Article10. Gormley ME Jr. Treatment of neuromuscular and musculoskeletal problems in cerebral palsy. Pediatr Rehabil. 2001; 4:5–16.11. Nahm NJ, Graham HK, Gormley ME Jr, Georgiadis AG. Management of hypertonia in cerebral palsy. Curr Opin Pediatr. 2018; 30:57–64.
Article12. Colver A, Fairhurst C, Pharoah PO. Cerebral palsy. Lancet. 2014; 383:1240–9.
Article13. Wiart L, Darrah J, Kembhavi G. Stretching with children with cerebral palsy: what do we know and where are we going? Pediatr Phys Ther. 2008; 20:173–8.
Article14. Wood E, Rosenbaum P. The gross motor function classification system for cerebral palsy: a study of reliability and stability over time. Dev Med Child Neurol. 2000; 42:292–6.
Article15. Katusic A, Alimovic S. The relationship between spasticity and gross motor capability in nonambulatory children with spastic cerebral palsy. Int J Rehabil Res. 2013; 36:205–10.
Article16. Gracies JM, Burke K, Clegg NJ, Browne R, Rushing C, Fehlings D, et al. Reliability of the Tardieu scale for assessing spasticity in children with cerebral palsy. Arch Phys Med Rehabil. 2010; 91:421–8.
Article17. Pin T, Dyke P, Chan M. The effectiveness of passive stretching in children with cerebral palsy. Dev Med Child Neurol. 2006; 48:855–62.
Article18. Park EY, Kim WH. Effect of neurodevelopmental treatment-based physical therapy on the change of muscle strength, spasticity, and gross motor function in children with spastic cerebral palsy. J Phys Ther Sci. 2017; 29:966–9.
Article19. Tilton AH. Therapeutic interventions for tone abnormalities in cerebral palsy. NeuroRx. 2006; 3:217–24.
Article20. Damiano DL. Rehabilitative therapies in cerebral palsy: the good, the not as good, and the possible. J Child Neurol. 2009; 24:1200–4.
Article21. Wu YN, Hwang M, Ren Y, Gaebler-Spira D, Zhang LQ. Combined passive stretching and active movement rehabilitation of lower-limb impairments in children with cerebral palsy using a portable robot. Neurorehabil Neural Repair. 2011; 25:378–85.
Article22. Arpino C, Vescio MF, De Luca A, Curatolo P. Efficacy of intensive versus nonintensive physiotherapy in children with cerebral palsy: a meta-analysis. Int J Rehabil Res. 2010; 33:165–71.
Article23. Hong BY, Jo L, Kim JS, Lim SH, Bae JM. Factors influencing the gross motor outcome of intensive therapy in children with cerebral palsy and developmental delay. J Korean Med Sci. 2017; 32:873–9.
Article24. Verschuren O, Peterson MD, Balemans AC, Hurvitz EA. Exercise and physical activity recommendations for people with cerebral palsy. Dev Med Child Neurol. 2016; 58:798–808.
Article25. O’Dwyer N, Neilson P, Nash J. Reduction of spasticity in cerebral palsy using feedback of the tonic stretch reflex: a controlled study. Dev Med Child Neurol. 1994; 36:770–86.26. Aisen ML, Kerkovich D, Mast J, Mulroy S, Wren TA, Kay RM, et al. Cerebral palsy: clinical care and neurological rehabilitation. Lancet Neurol. 2011; 10:844–52.
Article27. McNee AE, Gough M, Morrissey MC, Shortland AP. Increases in muscle volume after plantarflexor strength training in children with spastic cerebral palsy. Dev Med Child Neurol. 2009; 51:429–35.
Article28. Hagglund G, Wagner P. Spasticity of the gastrosoleus muscle is related to the development of reduced passive dorsiflexion of the ankle in children with cerebral palsy: a registry analysis of 2,796 examinations in 355 children. Acta Orthop. 2011; 82:744–8.29. Bell KJ, Ounpuu S, DeLuca PA, Romness MJ. Natural progression of gait in children with cerebral palsy. J Pediatr Orthop. 2002; 22:677–82.
Article30. Numanoglu A, Gunel MK. Intraobserver reliability of modified Ashworth scale and modified Tardieu scale in the assessment of spasticity in children with cerebral palsy. Acta Orthop Traumatol Turc. 2012; 46:196–200.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contributing Factors Analysis for the Changes of the Gross Motor Function in Children With Spastic Cerebral Palsy After Physical Therapy
- Percutaneous Selective Radiofrequency Thermocoagulation in the Treatment of Spastic Cerebral Palsy: A case report
- Immediate Effect of a Single Session of Whole Body Vibration on Spasticity in Children With Cerebral Palsy
- Effects of Botulinum Toxin A Treatment in Cerebral Palsy
- The Effects of Dilution Volume of Botulinum Toxin A on the Spasticity of Children with Cerebral Palsy