J Korean Ophthalmol Soc.
2019 Jul;60(7):654-660. 10.3341/jkos.2019.60.7.654.
Comparison of Posterior Capsule Rupture Rate during Phacoemulsification by Novice Ophthalmologists: Microscope vs. Intracameral Illumination
- Affiliations
-
- 1Department of Ophthalmology, Gachon University Gil Hospital, Incheon, Korea. eyedawns@gilhospital.com
- 2DMC Good Eye Clinic, Seoul, Korea.
- 3Department of Ophthalmology, Korea University Guro Hospital, Seoul, Korea.
- 4Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 5Department of Ophthalmology, Soonchunhyang University Seoul Hospital, Seoul, Korea.
- 6Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2453016
- DOI: http://doi.org/10.3341/jkos.2019.60.7.654
Abstract
- PURPOSE
We compared the posterior capsule rupture (PCR) rate between microscope versus intracameral illumination in phacoemulsification surgery performed by novice ophthalmologists.
METHODS
We conducted a retrospective chart review of 300 eyes of 211 patients who underwent phacoemulsification by novice ophthalmologists from March 2012 to October 2017. Novice ophthalmologists (n = 6) were divided into those using microscope illumination (n = 4) and intracameral illumination users (n = 2). The first 50 cataract surgery cases of each novice ophthalmologist were reviewed. The results using a phacoemulsification machine and microscopy were the same. The intraoperative complications and learning curve in each case were evaluated.
RESULTS
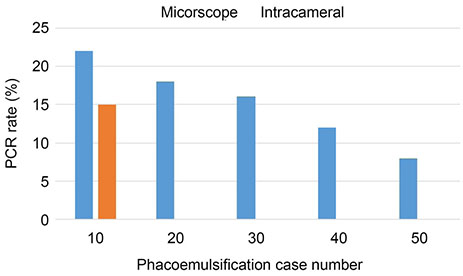
Phacoemulsifications performed by novice ophthalmologists showed a statistically significant difference in PCR rate between the microscope illumination (19.0%, 38/200) and intracameral illumination (4.0%, 4/100) groups (p = 0.001). The incidence of PCR was reduced to 22%, 18%, 16%, 12%, and 8% per 10 cases in the microscope group, while it was 15% in the first 10 cases and 0% in 50 cases thereafter in the intracameral illumination group.
CONCLUSIONS
Novice surgeons had a lower PCR rate during cataract surgery using intracameral illumination than using microscope illumination. Both groups showed a tendency for the PCR to decrease with increasing surgical cases, but the intracameral illumination group showed a shorter learning curve.
Keyword
MeSH Terms
Figure
Reference
-
1. Low SA, Braga-Mele R, Yan DB, El-Defrawy S. Intraoperative complication rates in cataract surgery performed by ophthalmology resident trainees compared to staff surgeons in a Canadian academic center. J Cataract Refract Surg. 2018; 44:1344–1349.
Article2. Bhagat N, Nissirios N, Potdevin L, et al. Complications in resident-performed phacoemulsification cataract surgery at new jersey medical school. Br J Ophthalmol. 2007; 91:1315–1317.
Article3. Le K, Bursztyn L, Rootman D, Harissi-Dagher M. National survey of Canadian ophthalmology residency education. Can J Ophthalmol. 2016; 51:219–225.
Article4. Eom Y, Kang SY, Kim HM, Song JS. A survey report on cataract surgical experiences during ophthalmology residency in Korea. J Korean Ophthalmol Soc. 2011; 52:429–433.
Article5. Randleman JB, Wolfe JD, Woodward M, et al. The resident surgeon phacoemulsification learning curve. Arch ophthalmol. 2007; 125:1215–1219.
Article6. Park UC, Kwon JW, Han YK. Clinical results of posterior capsule ruptures in the first 1,000 phacoemulsification cases. J Korean Ophthalmol Soc. 2005; 46:1270–1275.7. Jun JH, Chang SD. Clinical features of posterior capsule rupture during phacoemulsification performed by novice ophthalmologists. J Korean Ophthalmol Soc. 2014; 55:679–685.
Article8. Pingree MF, Crandall AS, Olson RJ. Cataract surgery complications in 1 year at an academic institution. J Cataract Refract Surg. 1999; 25:705–708.
Article9. Seo H, Nam DH, Lee JY, et al. Macular photostress and visual experience between microscope and intracameral illumination during cataract surgery. J Cataract Refract Surg. 2018; 44:190–197.
Article10. Wi J, Seo H, Lee JY, Nam DH. Phacoemulsification using a chisel-shaped illuminator: enhanced depth trench, one-shot crack, and phaco cut. Eur J Ophthalmol. 2016; 26:279–280.
Article11. Moon H, Lee JH, Lee JY, et al. Intracameral dynamic spotlight-assisted cataract surgery in eyes with corneal opacity, small pupil or advanced cataract. Acta Ophthalmol. 2015; 93:388–390.
Article12. Jung Y, Kim IN, Yoon J, et al. Intracameral illuminator-assisted advanced cataract surgery combined with 23-gauge vitrectomy in eyes with poor red reflex. J Cataract Refract Surg. 2013; 39:845–850.
Article13. Lee JY, Yoon J, Kim IN, et al. Intracameral illuminator-guided advanced lens capsule polishing during cataract surgery in eyes with diabetic retinopathy. Retina. 2012; 32:1420–1423.
Article14. Park YM, Park JY, Lee JS, et al. Comparative analysis of brilliant blue G and an intracameral illuminator in assisting visualization of the anterior capsule in eyes with vitreous hemorrhage. J Cataract Refract Surg. 2016; 42:1015–1021.
Article15. Yepez JB, Murati FA, García F, et al. Phacoemulsification outcomes with different illumination techniques. Eur J Ophthalmol. 2017; 27:797–800.
Article16. Rogers GM, Oetting TA, Lee AG, et al. Impact of a structured surgical curriculum on ophthalmic resident cataract surgery complication rates. J Cataract Refract Surg. 2009; 35:1956–1960.
Article17. Allinson RW, Metrikin DC, Fante RG. Incidence of vitreous loss among third-year residents performing phacoemulsification. Ophthalmology. 1992; 99:726–730.
Article18. Ezra DG, Aggarwal R, Michaelides M, et al. Skills acquisition and assessment after a microsurgical skills course for ophthalmology residents. Ophthalmology. 2009; 116:257–262.
Article19. Young BK, Greenberg PB. Is virtual reality training for resident cataract surgeons cost effective? Graefes Arch Clin Exp Ophthalmol. 2013; 251:2295–2296.
Article20. Ramani S, Pradeep TG, Sundaresh DD. Effect of wetlaboratory training on resident performed manual smallincision cataract surgery. Indian J Ophthalmol. 2018; 66:793–797.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Features of Posterior Capsule Rupture during Phacoemulsification Performed by Novice Ophthalmologists
- A Case of Isolated Posterior Capsule Rupture Caused by Blunt Ocular Trauma
- Analysis of Cause and Outcome of Posterior Capsular Rupture during Phacoemulsification in Cataract Surgery
- Cost-Effectiveness Analysis of Cataract Surgery for the Beginners Using Intraocular Illumination
- Effect of Intracameral Triamcinolone to Control Inflammation in Rabbit Eyes