J Korean Ophthalmol Soc.
2014 May;55(5):679-685. 10.3341/jkos.2014.55.5.679.
Clinical Features of Posterior Capsule Rupture during Phacoemulsification Performed by Novice Ophthalmologists
- Affiliations
-
- 1Department of Ophthalmology, Keimyung University School of Medicine, Daegu, Korea. changsd@dsmc.or.kr
- KMID: 2218088
- DOI: http://doi.org/10.3341/jkos.2014.55.5.679
Abstract
- PURPOSE
To report the related factors of posterior capsule rupture and the difference of postoperative visual prognosis after phacoemulsification by analyzing clinical features of the surgery performed by ten novice ophthalmologists.
METHODS
We retrospectively evaluated electronic medical records of 326 patients (412 phacoemulsification cases) who underwent surgery by novice ophthalmologists certified by the Board of Ophthalmology after a resident training program.
RESULTS
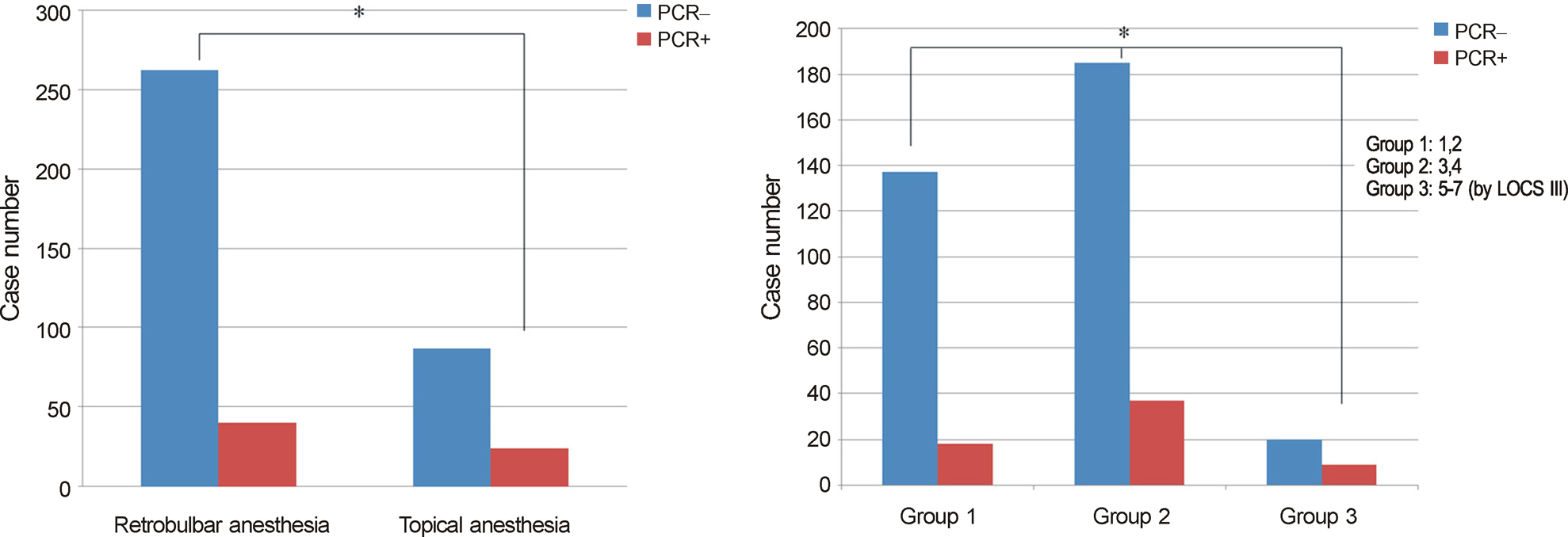
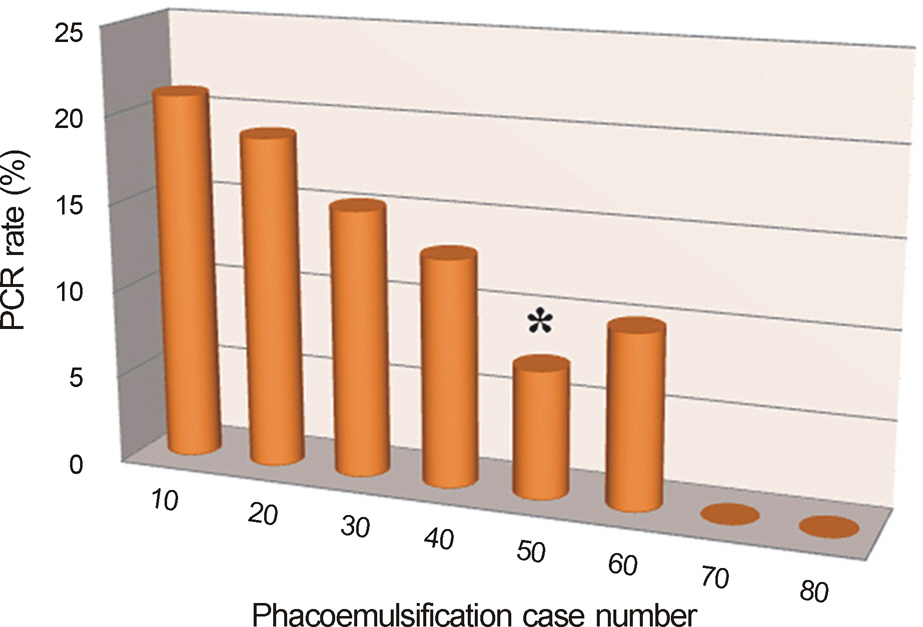
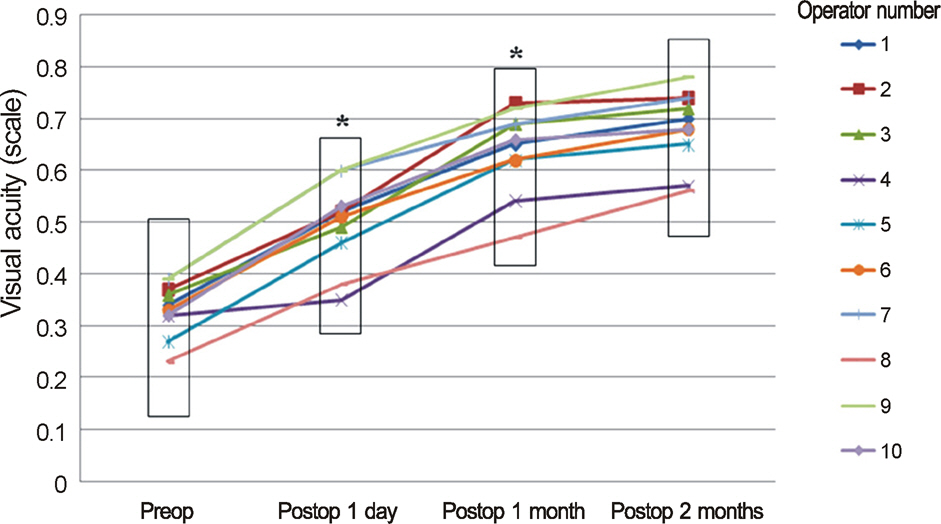
The number of cataract surgeries performed by each surgeon within the ophthalmology fellowship period (6 months - 2 years) ranged from 16 to 75 eyes, and perioperative posterior capsule ruptures occurred in 64 of 412 eyes (15.5%). Factors such as age, sex, laterality, axial length and clinical courses were not related to the rate of posterior capsule rupture. Nucleosclerosis was significantly related to the posterior capsule rupture rate and was especially higher in the group with a grade higher than five compared to that in the groups with a grade less than 5 based on the Lens Opacities Classification System III (p = 0.033). Factors of surgeon's subspecialty, nucleofractis method, and period between residency and the fellowship were not related to the posterior capsule rupture rate, except when considering anesthetic methods. The posterior capsule rupture rate was less frequent in the retrobulbar surgery group than the topical surgery group (p = 0.046). Postoperative visual outcomes were significantly different at postoperative day one and one month (p = 0.023, 0.022, respectively) but not at postoperative two months (p = 0.059).
CONCLUSIONS
Phacoemulsifications performed by novice ophthalmologists showed a statistically significant difference in posterior capsule rupture rate between nucleosclerosis and anesthesia groups. Postoperative visual outcome differed at postoperative day one and one month but not after two months postoperatively.
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Posterior Capsule Rupture Rate during Phacoemulsification by Novice Ophthalmologists: Microscope vs. Intracameral Illumination
Yu Jeong Kim, Hyejin Seo, Jong Hwan Lee, Seong-Woo Kim, Tae-Young Chung, Sung Jin Lee, Kyu Hyung Park, Dong Heun Nam
J Korean Ophthalmol Soc. 2019;60(7):654-660. doi: 10.3341/jkos.2019.60.7.654.
Reference
-
References
1. Eom Y, Kang SY, Kim HM, Song JS. A survey report on cataract surgical experiences during ophthalmology residency in korea. J Korean Ophthalmol Soc. 2011; 52:429–33.
Article2. Park UC, Kwon JW, Han YK. Clinical results of posterior capsule ruptures in the first 1000 phacoemulsification cases. J Korean Ophthalmol Soc. 2005; 46:1270–5.3. Park JW, Kim MS. Analysis of cause and outcome of posterior capsular rupture during phacoemulsification in cataract surgery. J Korean Ophthalmol Soc. 2003; 44:1311–6.4. Tabandeh H, Smeets B, Teimory M, Seward H. Learning phacoemulsification: the surgeon-in-training. Eye (Lond). 1994; 8:475–7.
Article5. Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmol. 2009; 116:431–6.
Article6. Woodfield AS, Gower EW, Cassard SD, Ramanthan S. Intraoperative phacoemulsification complication rates of second- and third-year ophthalmology residents a 5-year comparison. Ophthalmology. 2011; 118:954–8.7. Blomquist PH, Morales ME, Tong L, Ahn C. Risk factors for vitreous complications in resident-performed phacoemulsification surgery. J Cataract Refract Surg. 2012; 38:208–14.
Article8. Briszi A, Prahs P, Hillenkamp J, et al. Complication rate and risk factors for intraoperative complications in resident-performed pha-coemulsification surgery. Graefes Arch Clin Exp Ophthalmol. 2012; 250:1315–20.
Article9. Kelman CD. Symposium: Phacoemulsification. Summary of personal experience. Trans Am Acad Ophthalmol Otolaryngol. 1974; 78:OP35–8.10. Pedersen OO. Phacoemulsification and intraocular lens implantation in patients with cataract. Experiences of a beginning phacoemulsification surgeon. Acta Ophthalmol (Copenh). 1990; 68:59–64.11. Cruz OA, Wallace GW, Gay CA, et al. Visual results and complications of phacoemulsification with intraocular lens implantation performed by ophthalmology residents. Ophthalmol. 1992; 99:448–52.
Article12. Bae GJ, Kim KB, Joo CK. Clinical results of posterior capsular rupture during cataract operation. J Korean Ophthalmol Soc. 1993; 34:993–8.13. Kim KB, Jeun EJ, Kim JC. Clinical results of the eyes with posterior capsule rupture during cataract operation. J Korean Ophthalmol Soc. 1998; 39:2647–52.14. Muhtaseb M, Kalhoro A, Ionides A. A system for preoperative stratification of cataract patients according to risk of intraoperative complications: a prospective analysis of 1441 cases. Br J Ophthalmol. 2004; 88:1242–6.
Article15. Gupta A, Singh J, Dhillon B. Cataract classification system for risk stratification in surgery. J Cataract Refract Surg. 2011; 37:1363–4.
Article16. Abbasoglu OE, Hosal B, Tekeli O, Gursel E. Risk factors for vitreous loss in cataract surgery. Eur J Ophthalmol. 2000; 10:227–32.17. Park GS, Shyn KH. Risk factors for posterior capsular rupture in cataract surgery. J Korean Ophthalmol Soc. 2002; 43:1418–22.18. Ünal M, Yucel I, Sarici A, et al. Phacoemulsification with topical anesthesia: Resident experience. J Cataract Refract Surg. 2006; 32:1361–5.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Posterior Capsule Rupture Rate during Phacoemulsification by Novice Ophthalmologists: Microscope vs. Intracameral Illumination
- A Case of Isolated Posterior Capsule Rupture Caused by Blunt Ocular Trauma
- Analysis of Cause and Outcome of Posterior Capsular Rupture during Phacoemulsification in Cataract Surgery
- Clinical Results of Phacoemulsification with Scleral Pocket Incision in Diabetic Patients
- Clinical Results of Posterior Capsule Ruptures in the First 1000 Phacoemulsification Cases