J Neurocrit Care.
2019 Jun;12(1):46-50. 10.18700/jnc.190077.
Recurrent aseptic meningitis as an initial clinical presentation of primary Sjögren's syndrome
- Affiliations
-
- 1Department of Neurology, Yeungnam University College of Medicine, Daegu, Republic of Korea. sejinmayo@ynu.ac.kr
- KMID: 2452826
- DOI: http://doi.org/10.18700/jnc.190077
Abstract
- BACKGROUND
The neurological manifestations of Sjögren's syndrome (SjS) are nonspecific and may precede the onset of sicca symptoms. Hence, the diagnosis of SjS is often delayed. Recurrent aseptic meningitis is an uncommon neurological manifestation of primary SjS; only few cases have been reported in the medical literature.
CASE REPORT
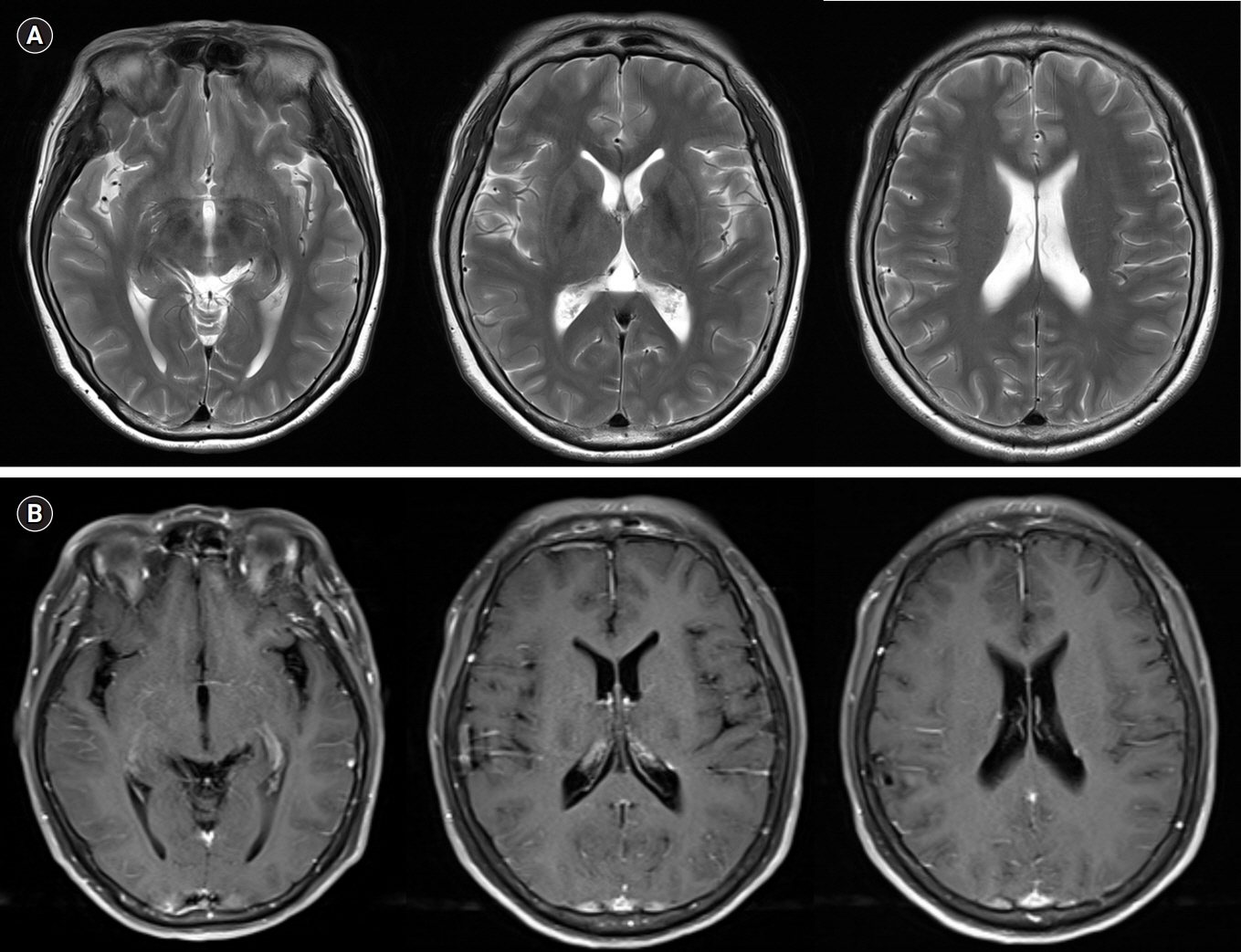
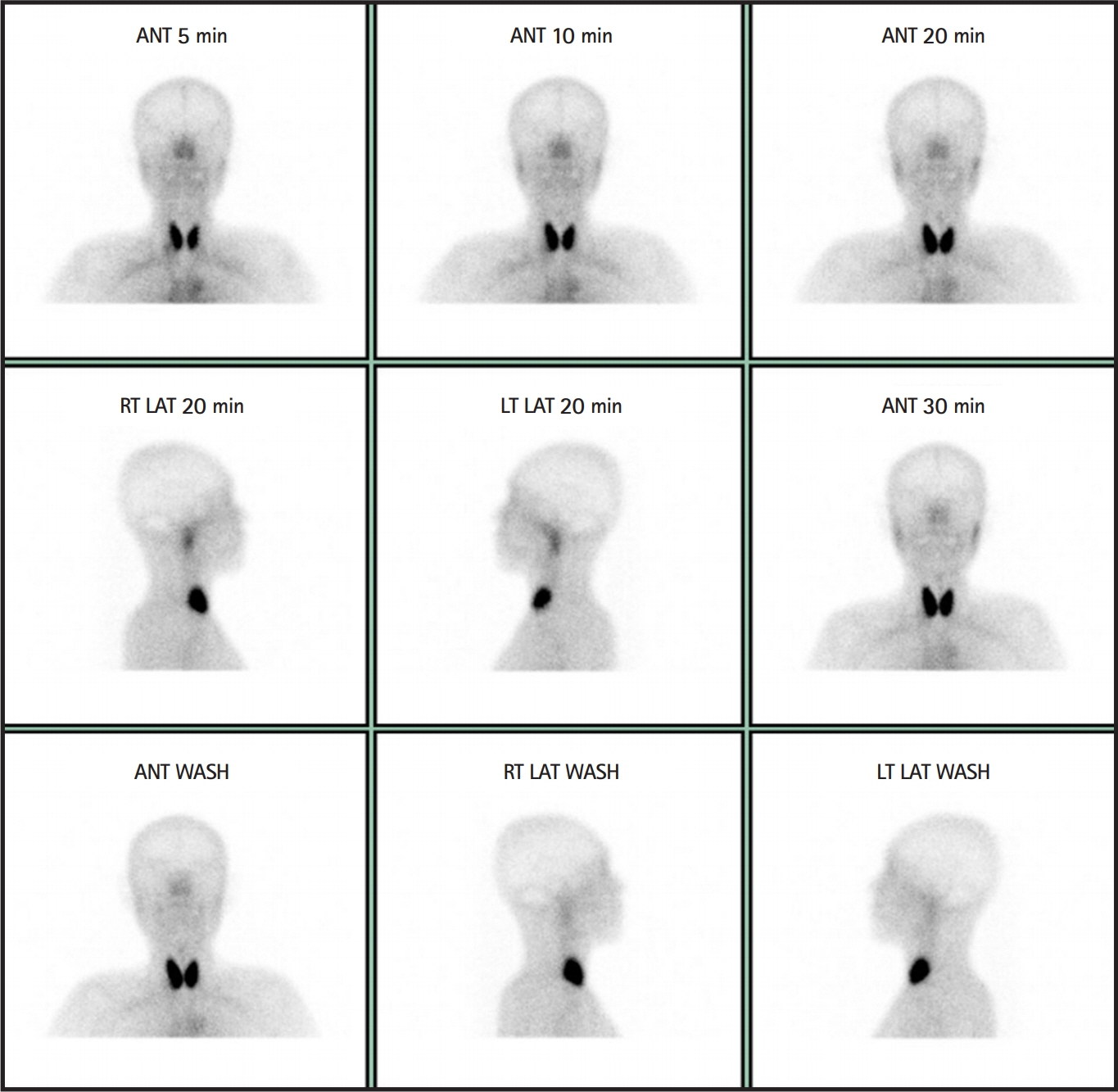
A 54-year-old woman was admitted for recurrent aseptic meningitis. The patient had a history of two episodes of aseptic meningitis, which had occurred 12 and 7 years before this presentation. The patient had overt sicca symptoms for 5 years. SjS was diagnosed based on the results of serum autoantibody tests, Schirmer's test, and salivary scintigraphy. We concluded that recurrent aseptic meningitis occurred as an initial presentation of primary SjS.
CONCLUSION
This case suggest that SjS should be included in the differential diagnosis of recurrent aseptic meningitis.
MeSH Terms
Figure
Reference
-
1. Delalande S, de Seze J, Fauchais AL, Hachulla E, Stojkovic T, Ferriby D, et al. Neurologic manifestations in primary Sjögren syndrome: a study of 82 patients. Medicine (Baltimore). 2004; 83:280–91.2. Tobón GJ, Pers JO, Devauchelle-Pensec V, Youinou P. Neurological disorders in primary Sjögren's syndrome. Autoimmune Dis. 2012; 2012:645967.
Article3. Rossi R, Valeria Saddi M. Subacute aseptic meningitis as neurological manifestation of primary Sjögren's syndrome. Clin Neurol Neurosurg. 2006; 108:688–91.
Article4. Alexander EL, Alexander GE. Aseptic meningoencephalitis in primary Sjögren's syndrome. Neurology. 1983; 33:593–8.5. Ishida K, Uchihara T, Mizusawa H. Recurrent aseptic meningitis: a new CSF complication of Sjögren's syndrome. J Neurol. 2007; 254:806–7.6. Shiboski CH, Shiboski SC, Seror R, Criswell LA, Labetoulle M, Lietman TM, et al. 2016 American College of Rheumatology/European League Against Rheumatism classification criteria for primary Sjögren's syndrome: a consensus and data-driven methodology involving three international patient cohorts. Ann Rheum Dis. 2017; 76:9–16.7. Rosenberg J, Galen BT. Recurrent meningitis. Curr Pain Headache Rep. 2017; 21:33.
Article8. Mori K, Iijima M, Koike H, Hattori N, Tanaka F, Watanabe H, et al. The wide spectrum of clinical manifestations in Sjögren's syndrome-associated neuropathy. Brain. 2005; 128(Pt 11):2518–34.
Article9. Gono T, Kawaguchi Y, Katsumata Y, Takagi K, Tochimoto A, Baba S, et al. Clinical manifestations of neurological involvement in primary Sjögren's syndrome. Clin Rheumatol. 2011; 30:485–90.
Article10. Fragkioudaki S, Mavragani CP, Moutsopoulos HM. Predicting the risk for lymphoma development in Sjögren syndrome: an easy tool for clinical use. Medicine (Baltimore). 2016; 95:e3766.11. Saraux A, Pers JO, Devauchelle-Pensec V. Treatment of primary Sjögren syndrome. Nat Rev Rheumatol. 2016; 12:456–71.
Article12. de Seze J, Delalande S, Fauchais AL, Hachulla E, Stojkovic T, Ferriby D, et al. Myelopathies secondary to Sjögren's syndrome: treatment with monthly intravenous cyclophosphamide associated with corticosteroids. J Rheumatol. 2006; 33:709–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Treatment with Steroid and Hydrochloroquine of Thrombocytopenia in Primary Sjögren's Syndrome
- Longitudinal Changes of the European League Against Rheumatism Sjögren's Syndrome Patient Reported Index in Korean Patients with Primary Sjögren's Syndrome
- A Case of Sjögren-Larsson Syndrome
- A Case Report of Benign Recurrent Aseptic Meningitis Mollaret`s Meningitis
- Acute Urinary Retention due to Aseptic Meningitis: Meningitis-Retention Syndrome