J Neurocrit Care.
2019 Jun;12(1):9-19. 10.18700/jnc.190086.
Assessment and management of coagulopathy in neurocritical care
- Affiliations
-
- 1Department of Neurosurgery, McGovern Medical School at UTHealth, Houston, TX, USA. Tiffany.R.Chang@uth.tmc.edu
- 2Department of Neurology, Columbia University, Vagelos College of Physicians and Surgeons, New York, NY, USA.
- KMID: 2452822
- DOI: http://doi.org/10.18700/jnc.190086
Abstract
- Coagulopathy may be defined as the loss of balance between hemostatic and fibrinolytic processes resulting in excessive bleeding, intravascular thrombosis or abnormalities in coagulation testing. It is frequently encountered across a wide range of conditions seen in the neurocritical care unit and can contribute to poor outcomes. Early recognition and appropriate management are key, with traumatic brain injury, acute ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage presenting unique challenges to the neurointensivist. We will discuss techniques to assess coagulopathies as well as treatment strategies for the brain injured patient.
Keyword
MeSH Terms
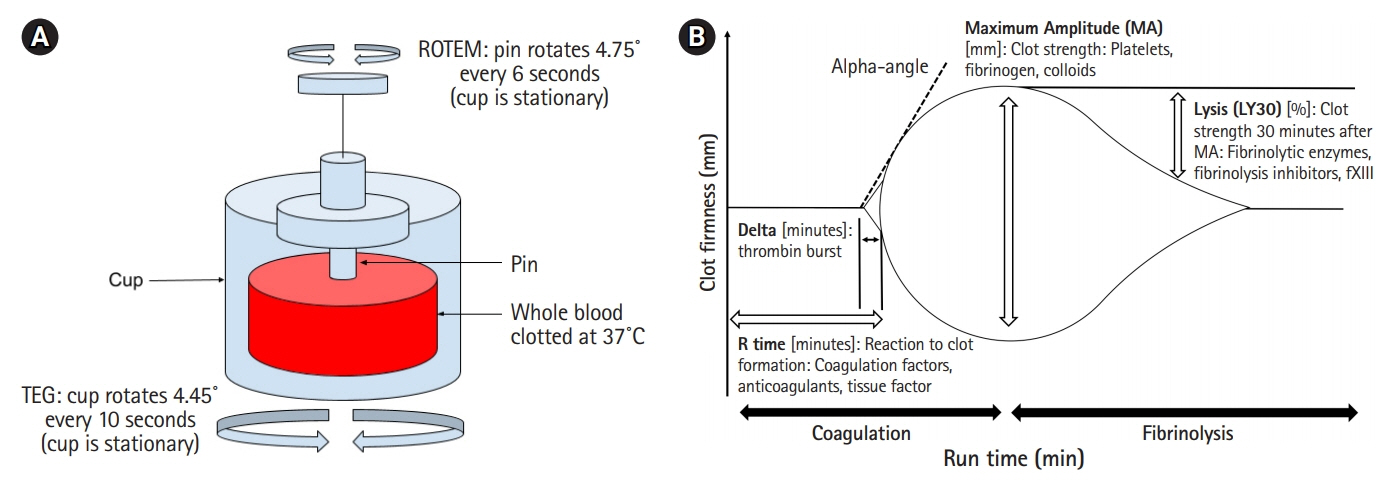
Figure
Reference
-
1. Levi M, Opal SM. Coagulation abnormalities in critically ill patients. Crit Care. 2006; 10:222.
Article2. Strauss R, Wehler M, Kreutzer D, Mehler K, Mueller A, Koebnick C, et al. Incidence and implications of coagulopathy in medical intensive care patients. Crit Care. 2001; 5(Suppl 1):P105.
Article3. Frontera JA, Lewin JJ 3rd, Rabinstein AA, Aisiku IP, Alexandrov AW, Cook AM, et al. Guideline for reversal of antithrombotics in intracranial hemorrhage: a statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care. 2016; 24:6–46.4. Abdelmalik PA, Boorman DW, Tracy J, Jallo J, Rincon F. Acute traumatic coagulopathy accompanying isolated traumatic brain injury is associated with worse long-term functional and cognitive outcomes. Neurocrit Care. 2016; 24:361–70.
Article5. Franke CL, de Jonge J, van Swieten JC, Op de Coul AA, van Gijn J. Intracerebral hematomas during anticoagulant treatment. Stroke. 1990; 21:726–30.
Article6. Flibotte JJ, Hagan N, O'Donnell J, Greenberg SM, Rosand J. Warfarin, hematoma expansion, and outcome of intracerebral hemorrhage. Neurology. 2004; 63:1059–64.
Article7. Flaherty ML, Kissela B, Woo D, Kleindorfer D, Alwell K, Sekar P, et al. The increasing incidence of anticoagulant-associated intracerebral hemorrhage. Neurology. 2007; 68:116–21.
Article8. Veltkamp R, Rizos T, Horstmann S. Intracerebral bleeding in patients on antithrombotic agents. Semin Thromb Hemost. 2013; 39:963–71.
Article9. Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:2032–60.
Article10. Hirsh J, Poller L. The international normalized ratio. A guide to understanding and correcting its problems. Arch Intern Med. 1994; 154:282–8.
Article11. Kitchens CS. To bleed or not to bleed? Is that the question for the PTT? J Thromb Haemost. 2005; 3:2607–11.
Article12. Vanderwerf JD, Kumar MA. Management of neurologic complications of coagulopathies. Handb Clin Neurol. 2017; 141:743–64.
Article13. Walsh M, Fritz S, Hake D, Son M, Greve S, Jbara M, et al. Targeted thromboelastographic (TEG) blood component and pharmacologic hemostatic therapy in traumatic and acquired coagulopathy. Curr Drug Targets. 2016; 17:954–70.
Article14. Sankarankutty A, Nascimento B, Teodoro da Luz L, Rizoli S. TEG® and ROTEM® in trauma: similar test but different results? World J Emerg Surg. 2012; 7 Suppl 1:S3.
Article15. Holcomb JB, Minei KM, Scerbo ML, Radwan ZA, Wade CE, Kozar RA, et al. Admission rapid thrombelastography can replace conventional coagulation tests in the emergency department: experience with 1974 consecutive trauma patients. Ann Surg. 2012; 256:476–86.16. Gonzalez E, Moore EE, Moore HB, Chapman MP, Chin TL, Ghasabyan A, et al. Goal-directed hemostatic resuscitation of trauma-induced coagulopathy: a pragmatic randomized clinical trial comparing a viscoelastic assay to conventional coagulation assays. Ann Surg. 2016; 263:1051–9.17. Tapia NM, Chang A, Norman M, Welsh F, Scott B, Wall MJ Jr, et al. TEG-guided resuscitation is superior to standardized MTP resuscitation in massively transfused penetrating trauma patients. J Trauma Acute Care Surg. 2013; 74:378–85.
Article18. Johansson PI, Stensballe J. Effect of haemostatic control resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang. 2009; 96:111–8.
Article19. Collyer TC, Gray DJ, Sandhu R, Berridge J, Lyons G. Assessment of platelet inhibition secondary to clopidogrel and aspirin therapy in preoperative acute surgical patients measured by Thrombelastography Platelet Mapping. Br J Anaesth. 2009; 102:492–8.
Article20. Sibbing D, Braun S, Jawansky S, Vogt W, Mehilli J, Schömig A, et al. Assessment of ADP-induced platelet aggregation with light transmission aggregometry and multiple electrode platelet aggregometry before and after clopidogrel treatment. Thromb Haemost. 2008; 99:121–6.
Article21. McDonald MM, Almaghrabi TS, Saenz DM, Cai C, Rahbar MH, Choi HA, et al. Dual antiplatelet therapy is associated with coagulopathy detectable by thrombelastography in acute stroke. J Intensive Care Med. 2017; Jan. 1. [Epub]. https://doi.org/10.1177/0885066617729644.
Article22. Frontera JA, Provencio JJ, Sehba FA, McIntyre TM, Nowacki AS, Gordon E, et al. The role of platelet activation and inflammation in early brain injury following subarachnoid hemorrhage. Neurocrit Care. 2017; 26:48–57.
Article23. Naidech AM, Jovanovic B, Liebling S, Garg RK, Bassin SL, Bendok BR, et al. Reduced platelet activity is associated with early clot growth and worse 3-month outcome after intracerebral hemorrhage. Stroke. 2009; 40:2398–401.
Article24. Lindblad C, Thelin EP, Nekludov M, Frostell A, Nelson DW, Svensson M, et al. Assessment of platelet function in traumatic brain injury: a retrospective observational study in the neuro-critical care setting. Front Neurol. 2018; 9:15.
Article25. Ettinger MG. Coagulation abnormalities in subarachnoid hemorrhage. Stroke. 1970; 1:139–42.
Article26. Ettinger MG. Thromboelastographic studies in cerebral infarction. Stroke. 1974; 5:350–4.
Article27. Elliott A, Wetzel J, Roper T, Pivalizza E, McCarthy J, Wallace C, et al. Thromboelastography in patients with acute ischemic stroke. Int J Stroke. 2015; 10:194–201.
Article28. McDonald MM, Wetzel J, Fraser S, Elliott A, Bowry R, Kawano-Castillo JF, et al. Thrombelastography does not predict clinical response to rtPA for acute ischemic stroke. J Thromb Thrombolysis. 2016; 41:505–10.
Article29. Yao X, Dong Q, Song Y, Wang Y, Deng Y, Li Y. Thrombelastography maximal clot strength could predict one-year functional outcome in patients with ischemic stroke. Cerebrovasc Dis. 2014; 38:182–90.
Article30. Kawano-Castillo J, Ward E, Elliott A, Wetzel J, Hassler A, McDonald M, et al. Thrombelastography detects possible coagulation disturbance in patients with intracerebral hemorrhage with hematoma enlargement. Stroke. 2014; 45:683–8.
Article31. Lauridsen SV, Hvas AM, Sandgaard E, Gyldenholm T, Rahbek C, Hjort N, et al. Coagulation profile after spontaneous intracerebral hemorrhage: a cohort study. J Stroke Cerebrovasc Dis. 2018; 27:2951–61.
Article32. Kang DW, Han MK, Kim HJ, Yun SC, Jeon SB, Bae HJ, et al. New ischemic lesions coexisting with acute intracerebral hemorrhage. Neurology. 2012; 79:848–55.
Article33. Windeløv NA, Welling KL, Ostrowski SR, Johansson PI. The prognostic value of thrombelastography in identifying neurosurgical patients with worse prognosis. Blood Coagul Fibrinolysis. 2011; 22:416–9.34. Larsen CC, Hansen-Schwartz J, Nielsen JD, Astrup J. Blood coagulation and fibrinolysis after experimental subarachnoid hemorrhage. Acta Neurochir (Wien). 2010; 152:1577–81.
Article35. Ramchand P, Nyirjesy S, Frangos S, Doerfler S, Nawalinski K, Quattrone F, et al. Thromboelastography parameter predicts outcome after subarachnoid hemorrhage: an exploratory analysis. World Neurosurg. 2016; 96:215–21.
Article36. Schreiber MA, Differding J, Thorborg P, Mayberry JC, Mullins RJ. Hypercoagulability is most prevalent early after injury and in female patients. J Trauma. 2005; 58:475–80.
Article37. Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008; 65:748–54.
Article38. Johansson PI, Stissing T, Bochsen L, Ostrowski SR. Thrombelastography and tromboelastometry in assessing coagulopathy in trauma. Scand J Trauma Resusc Emerg Med. 2009; 17:45.
Article39. Harhangi BS, Kompanje EJ, Leebeek FW, Maas AI. Coagulation disorders after traumatic brain injury. Acta Neurochir (Wien). 2008; 150:165–75.
Article40. de Oliveira Manoel AL, Neto AC, Veigas PV, Rizoli S. Traumatic brain injury associated coagulopathy. Neurocrit Care. 2015; 22:34–44.
Article41. Nakae R, Takayama Y, Kuwamoto K, Naoe Y, Sato H, Yokota H. Time course of coagulation and fibrinolytic parameters in patients with traumatic brain injury. J Neurotrauma. 2016; 33:688–95.
Article42. Stravitz RT, Lisman T, Luketic VA, Sterling RK, Puri P, Fuchs M, et al. Minimal effects of acute liver injury/acute liver failure on hemostasis as assessed by thromboelastography. J Hepatol. 2012; 56:129–36.
Article43. Greinacher A, Selleng K. Thrombocytopenia in the intensive care unit patient. Hematology Am Soc Hematol Educ Program. 2010; 2010:135–43.
Article44. Chan KH, Mann KS, Chan TK. The significance of thrombocytopenia in the development of postoperative intracranial hematoma. J Neurosurg. 1989; 71:38–41.
Article45. Hunt BJ. Bleeding and coagulopathies in critical care. Surv Anesthesiol. 2014; 58:274–5.
Article46. Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009; 145:24–33.47. Roderick P, Davies R, Jones C, Feest T, Smith S, Farrington K. Simulation model of renal replacement therapy: predicting future demand in England. Nephrol Dial Transplant. 2004; 19:692–701.
Article48. Pavord S, Myers B. Bleeding and thrombotic complications of kidney disease. Blood Rev. 2011; 25:271–8.
Article49. Mannucci PM, Vicente V, Vianello L, Cattaneo M, Alberca I, Coccato MP, et al. Controlled trial of desmopressin in liver cirrhosis and other conditions associated with a prolonged bleeding time. Blood. 1986; 67:1148–53.
Article50. Kim JH, Baek CH, Min JY, Kim JS, Kim SB, Kim H. Desmopressin improves platelet function in uremic patients taking antiplatelet agents who require emergent invasive procedures. Ann Hematol. 2015; 94:1457–61.
Article51. Zeigler ZR, Megaludis A, Fraley DS. Desmopressin (d-DAVP) effects on platelet rheology and von Willebrand factor activities in uremia. Am J Hematol. 1992; 39:90–5.
Article52. Gordz S, Mrowietz C, Pindur G, Park JW, Jung F. Effect of desmopressin (DDAVP) on platelet membrane glycoprotein expression in patients with von Willebrand's disease. Clin Hemorheol Microcirc. 2005; 32:83–7.53. Kapapa T, Röhrer S, Struve S, Petscher M, König R, Wirtz CR, et al. Desmopressin acetate in intracranial haemorrhage. Neurol Res Int. 2014; 2014:298767.
Article54. Van Herzeele C, De Bruyne P, Evans J, Eggert P, Lottmann H, Norgaard JP, et al. Safety profile of desmopressin tablet for enuresis in a prospective study. Adv Ther. 2014; 31:1306–16.
Article55. He J, Whelton PK, Vu B, Klag MJ. Aspirin and risk of hemorrhagic stroke: a meta-analysis of randomized controlled trials. JAMA. 1998; 280:1930–5.56. Creager MA. Results of the CAPRIE trial: efficacy and safety of clopidogrel. Clopidogrel versus aspirin in patients at risk of ischaemic events. Vasc Med. 1998; 3:257–60.57. Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007; 357:2001–15.
Article58. Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009; 361:1045–57.
Article59. ACTIVE Writing Group of the ACTIVE Investigators, Connolly S, Pogue J, Hart R, Pfeffer M, Hohnloser S, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet. 2006; 367:1903–12.60. Khan NI, Siddiqui FM, Goldstein JN, Cox M, Xian Y, Matsouaka RA, et al. Association between previous use of antiplatelet therapy and intracerebral hemorrhage outcomes. Stroke. 2017; 48:1810–7.
Article61. Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016; 387:2605–13.
Article62. Choi PA, Parry PV, Bauer JS, Zusman BE, Panczykowski DM, Puccio AM, et al. Use of aspirin and P2Y12 response assays in detecting reversal of platelet inhibition with platelet transfusion in patients with traumatic brain injury on antiplatelet therapy. Neurosurgery. 2017; 80:98–104.
Article63. Naidech AM, Liebling SM, Rosenberg NF, Lindholm PF, Bernstein RA, Batjer HH, et al. Early platelet transfusion improves platelet activity and may improve outcomes after intracerebral hemorrhage. Neurocrit Care. 2012; 16:82–7.
Article64. Furay E, Daley M, Teixeira PG, Coopwood TB, Aydelotte JD, Malesa N, et al. Goal-directed platelet transfusions correct platelet dysfunction and may improve survival in patients with severe traumatic brain injury. J Trauma Acute Care Surg. 2018; 85:881–7.
Article65. Tcheng JE. Clinical challenges of platelet glycoprotein IIb/IIIa receptor inhibitor therapy: bleeding, reversal, thrombocytopenia, and retreatment. Am Heart J. 2000; 139(2 Pt 2):S38–45.
Article66. Calmer S, Ferkau A, Larmann J, Johanning K, Czaja E, Hagl C, et al. Desmopressin (DDAVP) improves recruitment of activated platelets to collagen but simultaneously increases platelet endothelial interactions in vitro. Platelets. 2014; 25:8–15.67. Mannucci PM, Remuzzi G, Pusineri F, Lombardi R, Valsecchi C, Mecca G, et al. Deamino-8-D-arginine vasopressin shortens the bleeding time in uremia. N Engl J Med. 1983; 308:8–12.
Article68. Reiter RA, Mayr F, Blazicek H, Galehr E, Jilma-Stohlawetz P, Domanovits H, et al. Desmopressin antagonizes the in vitro platelet dysfunction induced by GPIIb/IIIa inhibitors and aspirin. Blood. 2003; 102:4594–9.
Article69. Wademan BH, Galvin SD. Desmopressin for reducing postoperative blood loss and transfusion requirements following cardiac surgery in adults. Interact Cardiovasc Thorac Surg. 2014; 18:360–70.
Article70. Jin L, Ji HW. Effect of desmopressin on platelet aggregation and blood loss in patients undergoing valvular heart surgery. Chin Med J (Engl). 2015; 128:644–7.
Article71. Naidech AM, Maas MB, Levasseur-Franklin KE, Liotta EM, Guth JC, Berman M, et al. Desmopressin improves platelet activity in acute intracerebral hemorrhage. Stroke. 2014; 45:2451–3.
Article72. Masotti L, Di Napoli M, Godoy DA, Rafanelli D, Liumbruno G, Koumpouros N, et al. The practical management of intracerebral hemorrhage associated with oral anticoagulant therapy. Int J Stroke. 2011; 6:228–40.
Article73. Pabinger I, Brenner B, Kalina U, Knaub S, Nagy A, Ostermann H, et al. Prothrombin complex concentrate (Beriplex P/N) for emergency anticoagulation reversal: a prospective multinational clinical trial. J Thromb Haemost. 2008; 6:622–31.74. Steiner T, Poli S, Griebe M, Hüsing J, Hajda J, Freiberger A, et al. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Lancet Neurol. 2016; 15:566–73.
Article75. Dias JD, Norem K, Doorneweerd DD, Thurer RL, Popovsky MA, Omert LA. Use of thromboelastography (TEG) for detection of new oral anticoagulants. Arch Pathol Lab Med. 2015; 139:665–73.
Article76. Marlu R, Hodaj E, Paris A, Albaladejo P, Cracowski JL, Pernod G. Effect of non-specific reversal agents on anticoagulant activity of dabigatran and rivaroxaban: a randomised crossover ex vivo study in healthy volunteers. Thromb Haemost. 2012; 108:217–24.77. Connolly SJ, Crowther M, Eikelboom JW, Gibson CM, Curnutte JT, Lawrence JH, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019; 380:1326–35.
Article78. Pollack CV Jr, Reilly PA, Weitz JI. Dabigatran reversal with idarucizumab. N Engl J Med. 2017; 377:1691–2.
Article79. Sarode R, Milling TJ Jr, Refaai MA, Mangione A, Schneider A, Durn BL, et al. Efficacy and safety of a 4-factor prothrombin complex concentrate in patients on vitamin K antagonists presenting with major bleeding: a randomized, plasma-controlled, phase IIIb study. Circulation. 2013; 128:1234–43.80. Goldstein JN, Refaai MA, Milling TJ Jr, Lewis B, Goldberg-Alberts R, Hug BA, et al. Four-factor prothrombin complex concentrate versus plasma for rapid vitamin K antagonist reversal in patients needing urgent surgical or invasive interventions: a phase 3b, open-label, non-inferiority, randomised trial. Lancet. 2015; 385:2077–87.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hiccups in neurocritical care
- Neurotrauma Code: Proposal for the Implementation of Strategies in Areas of Difficult Care for a Time-dependent Condition.
- Cooperative Sedation in Moderate Traumatic Brain Injury: A Tool for Neurocritical Care Management
- Basic considerations on magnesium in the management of neurocritical patients
- Impact of Neurointensivist Co-Management in a Semiclosed Neurocritical-Care Unit