Kosin Med J.
2019 Jun;34(1):1-14. 10.7180/kmj.2019.34.1.1.
Association between Ischemic Electrocardiographic Changes during Acetylcholine Provocation Test and Long-Term Clinical Outcomes in Patients with Vasospastic Angina
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Kosin University Gospel Hospital, Busan, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Cardiovascular Center, Korea University Guro Hospital, Seoul, Korea. swrha617@yahoo.co.kr
- KMID: 2451770
- DOI: http://doi.org/10.7180/kmj.2019.34.1.1
Abstract
OBJECTIVES
Intracoronary injection of acetylcholine (Ach) has been shown to induce significant coronary artery spasm (CAS) in patients with vasospastic angina. Clinical significance and angiographic characteristics of patients with ischemic electrocardiogram (ECG) changes during the Ach provocation test are not clarified yet.
METHODS
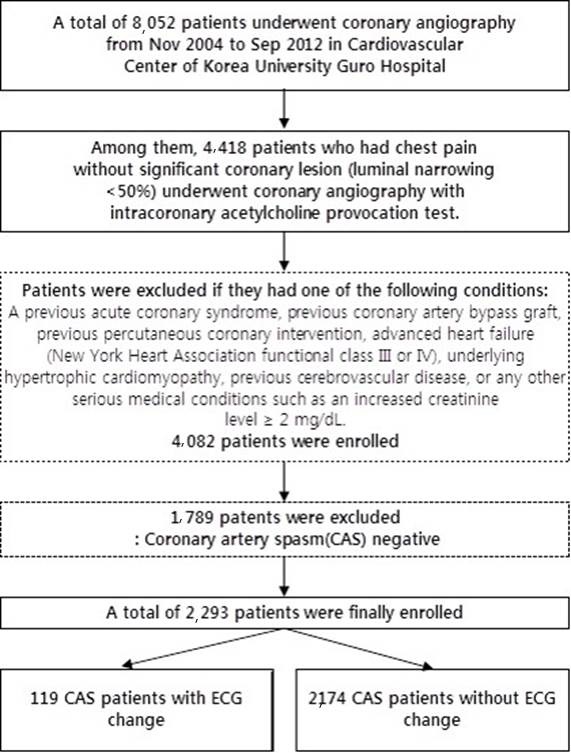
A total 4,418 consecutive patients underwent coronary angiography with Ach provocation tests from 2004 to 2012 were enrolled. Ischemic ECG changes were defined as transient ST-segment depression or elevation ( > 1 mm) and T inversion with/without chest pain. Finally, a total 2,293 patients (28.5% of total subjects) proven CAS were enrolled for this study.
RESULTS
A total 119 patients (5.2%) showed ECG changes during Ach provocation tests. The baseline clinical and procedural characteristics are well balanced between the two groups. Ischemic ECG change group showed more frequent chest pain, higher incidence of baseline spasm, severe vasospasm, multi-vessel involvement, and more diffuse spasm ( > 30 mm) than those without ischemic ECG changes. At 5 years, the incidences of death, major adverse cardiac events (MACE) and major adverse cardiac and cerebral events (MACCE) were higher in the ischemic ECG change group despite of optimal medical therapy.
CONCLUSIONS
The patients with ischemic ECG changes during Ach provocation tests were associated with more frequent chest pain, baseline spasm, diffuse, severe and multi-vessel spasm than patients without ischemic ECG changes. At 5-years, the incidences of death, MACE and MACCE were higher in the ischemic ECG change group, suggesting more intensive medical therapy with close clinical follow up will be required.
Keyword
MeSH Terms
Figure
Reference
-
1. Ong P, Athanasiadis A, Borgulya G, Mahrholdt H, Kaski JC, Sechtem U. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries. The ACOVA Study (Abnormal COronary VAsomotion in patients with stable angina and unobstructed coronary arteries). J Am Coll Cardiol. 2012; 59:655–662.
Article2. Douglas PS, Patel MR, Bailey SR, Dai D, Kaltenbach L, Brindis RG, et al. Hospital variability in the rate of finding obstructive coronary artery disease at elective, diagnostic coronary angiography. J Am Coll Cardiol. 2011; 58:801–809.
Article3. Johnston N, Schenck-Gustafsson K, Lagerqvist B. Are we using cardiovascular medications and coronary angiography appropriately in men and women with chest pain? Eur Heart J. 2011; 32:1331–1336.
Article4. Takagi Y, Yasuda S, Takahashi J, Tsunoda R, Ogata Y, Seki A, et al. Clinical implications of provocation tests for coronary artery spasm: safety, arrhythmic complications, and prognostic impact: multicentre registry study of the Japanese Coronary Spasm Association. Eur Heart J. 2013; 34:258–267.
Article5. el-Tamimi H, Davies GJ, Crea F, Maseri A. Response of human coronary arteries to acetylcholine after injury by coronary angioplasty. J Am Coll Cardiol. 1993; 21:1152–1157.
Article6. Im SI, Rha SW, Choi BG, Choi SY, Kim SW, Na JO, et al. Angiographic and clinical characteristics according to intracoronary acetylcholine dose in patients with myocardial bridge. Cardiology. 2013; 125:250–257.
Article7. Im SI, Choi WG, Rha SW, Choi BG, Choi SY, Kim SW, et al. Significant response to lower acetylcholine dose is associated with worse clinical and angiographic characteristics in patients with vasospastic angina. Korean Circ J. 2013; 43:468–473.
Article8. Summers MR, Lerman A, Lennon RJ, Rihal CS, Prasad A. Myocardial ischaemia in patients with coronary endothelial dysfunction: insights from body surface ECG mapping and implications for invasive evaluation of chronic chest pain. Eur Heart J. 2011; 32:2758–2765.
Article9. Obata JE, Kitta Y, Takano H, Kodama Y, Nakamura T, Mende A, et al. Sirolimus-eluting stent implantation aggravates endothelial vasomotor dysfunction in the infarct-related coronary artery in patients with acute myocardial infarction. J Am Coll Cardiol. 2007; 50:1305–1309.
Article10. Wakabayashi K, Suzuki H, Honda Y, Wakatsuki D, Kawachi K, Ota K, et al. Provoked coronary spasm predicts adverse outcome in patients with acute myocardial infarction: a novel predictor of prognosis after acute myocardial infarction. J Am Coll Cardiol. 2008; 52:518–522.
Article11. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17.
Article12. Onaka H, Hirota Y, Shimada S, Kita Y, Sakai Y, Kawakami Y, et al. Clinical observation of spontaneous anginal attacks and multivessel spasm in variant angina pectoris with normal coronary arteries: evaluation by 24-hour 12-lead electrocardiography with computer analysis. J Am Coll Cardiol. 1996; 27:38–44.
Article13. Ohba K, Sugiyama S, Sumida H, Nozaki T, Matsubara J, Matsuzawa Y, et al. Microvascular coronary artery spasm presents distinctive clinical features with endothelial dysfunction as nonobstructive coronary artery disease. J Am Heart Assoc. 2012; 1:e002485.
Article14. Newman CM, Maseri A, Hackett DR, el-Tamimi HM, Davies GJ. Response of angiographically normal and atherosclerotic left anterior descending coronary arteries to acetylcholine. Am J Cardiol. 1990; 66:1070–1076.
Article15. Ludmer PL, Selwyn AP, Shook TL, Wayne RR, Mudge GH, Alexander RW, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986; 315:1046–1051.
Article16. Lee SJ, Park SJ, Park SW, Kim JJ, Song JK, Hong MK, et al. Increased basal tone and hyperresponsiveness to acetylcholine and ergonovine in spasm-related coronary arteries in patients with variant angina. Int J Cardiol. 1996; 55:117–126.
Article17. Kaski JC, Maseri A, Vejar M, Crea F, Hackett D. Spontaneous coronary artery spasm in variant angina is caused by a local hyperreactivity to a generalized constrictor stimulus. J Am Coll Cardiol. 1989; 14:1456–1463.
Article18. Kuga T, Egashira K, Inou T, Takeshita A. Correlation of basal coronary artery tone with constrictive response to ergonovine in patients with variant angina. J Am Coll Cardiol. 1993; 22:144–150.
Article19. Yasue H, Omote S, Takizawa A, Nagao M, Miwa K, Tanaka S. Circadian variation of exercise capacity in patients with Prinzmetal's variant angina: role of exercise-induced coronary arterial spasm. Circulation. 1979; 59:938–948.
Article20. Okumura K, Yasue H, Matsuyama K, Goto K, Miyagi H, Ogawa H. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol. 1988; 12:883–888.
Article21. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Cir J. 2010; 74:1745–1762.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Vasomotor Tone In Vasospastic Angina
- Follow-up Provocation Test in Patients with Coronary Artery Spasm
- Long-term Circadian Patterns of Angina Attacks and Non-pharmacological Provocation Tests Responses in Patients with Vasospastic Angina
- Diagnostic Significance of ECG Ergonovine Provocation Test in Patients with Vasospastic Angina
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality