J Clin Neurol.
2019 Jan;15(1):54-61. 10.3988/jcn.2019.15.1.54.
Impact of Functional Status on Noncardioembolic Ischemic Stroke Recurrence Within 1 Year: The Korean Stroke Cohort for Functioning and Rehabilitation Study
- Affiliations
-
- 1Department of Rehabilitation Medicine, Wonkwang University School of Medicine and Institute of Wonkwang Medical Science, Iksan, Korea. mcjoo68@wku.ac.kr
- 2Department of Rehabilitation Medicine, School of Medicine, Chungnam National University, Daejeon, Korea.
- 3Department of Rehabilitation Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 4Department and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 5Department of Physical and Rehabilitation Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 6Department of Rehabilitation Medicine, Pusan National University School of Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea.
- 7Department of Preventive Medicine, Wonkwang University School of Medicine, Iksan, Korea.
- 8Department of Rehabilitation Medicine, Kyungpook National University School of Medicine, Kyungpook National University Hospital, Daegu, Korea.
- 9Department of Rehabilitation Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea.
- 10Department of Statistics, Hallym University, Chuncheon, Korea.
- 11Department of Health Convergence, Ewha Womans University, Seoul, Korea.
- 12Department of Physical and Rehabilitation Medicine, Sungkyunkwan University School of Medicine, Seoul, Korea. yunkim@skku.edu
- KMID: 2451145
- DOI: http://doi.org/10.3988/jcn.2019.15.1.54
Abstract
- BACKGROUND AND PURPOSE
Few studies have investigated the relationship between the specific functional factors potentially associated with functional level and stroke recurrence. We conducted a study of patients with noncardioembolic ischemic stroke (NCIS) to determine the functional factors affecting recurrence within the first year.
METHODS
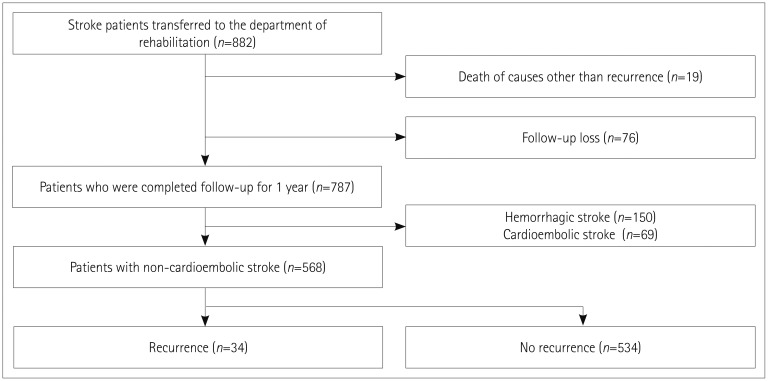
In total, 568 first-ever NCIS patients (age=65.1±17.4 years, mean±SD) were analyzed in a multicenter, prospective cohort study registered from August 2012. Demographic characteristics, past medical history, comorbidities, laboratory data, stroke features in neuroimaging, acute treatments, and medications at discharge were assessed. Functional factors reflecting gross functional impairment, ambulatory function, motor function, activities of daily living, cognition, language ability, swallowing function, mood, and quality of life were comprehensively evaluated in face-to-face assessments using standardized tools at the time of discharge.
RESULTS
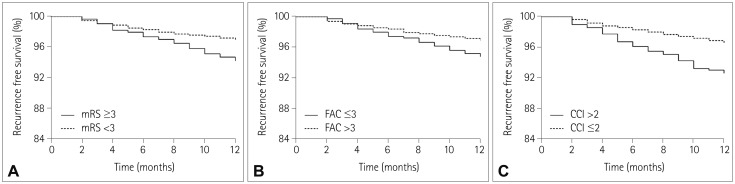
The cumulative incidence of stroke recurrence in NCIS was 6.0% (n=34) at 1 year. The period from admission to discharge was 34.4±7.0 days. The independent predictors of stroke recurrence within 1 year in multivariate Cox proportional-hazards regression analyses were 1) age [per-year hazard ratio (HR)=1.04, 95% confidence interval (CI)=0.97-1.06, p=0.048], 2) Charlson Comorbidity Index higher than 2 (HR=1.72, 95% CI=1.26-2.22, p=0.016), 3) modified Rankin Scale score of 3 or more at discharge (HR=1.56, 95% CI=1.22-1.94, p=0.032), and 4) Functional Ambulation Category of 3 or less at discharge (HR=2.56, 95% CI=1.84-3.31, p=0.008).
CONCLUSIONS
In addition to patient age, moderate-to-severe functional impairment requiring the help of others (especially for ambulation) at the time of discharge and the severity of comorbidity were independent predictors of stroke recurrence within 1 year of the first NCIS.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Stroke Rehabilitation Fact Sheet in Korea
Se Hee Jung
Ann Rehabil Med. 2022;46(1):1-8. doi: 10.5535/arm.22001.
Reference
-
1. Elkind MS. Outcomes after stroke: risk of recurrent ischemic stroke and other events. Am J Med. 2009; 122(4 Suppl 2):S7–S13. PMID: 19332241.
Article2. Kuwashiro T, Sugimori H, Ago T, Kamouchi M, Kitazono T. FSR Investigators. Risk factors predisposing to stroke recurrence within one year of non-cardioembolic stroke onset: the Fukuoka Stroke Registry. Cerebrovasc Dis. 2012; 33:141–149. PMID: 22179660.
Article3. Hillen T, Coshall C, Tilling K, Rudd AG, McGovern R, Wolfe CD. South London Stroke Register. Cause of stroke recurrence is multifactorial: patterns, risk factors, and outcomes of stroke recurrence in the south London stroke register. Stroke. 2003; 34:1457–1463. PMID: 12750544.4. Callaly E, Ni Chroinin D, Hannon N, Marnane M, Akijian L, Sheehan O, et al. Rates, predictors, and outcomes of early and late recurrence after stroke: the North Dublin Population Stroke Study. Stroke. 2016; 47:244–246. PMID: 26585395.5. Andersen SD, Gorst-Rasmussen A, Lip GY, Bach FW, Larsen TB. Recurrent stroke: the value of the CHA2DS2VASc score and the essen stroke risk score in a nationwide stroke cohort. Stroke. 2015; 46:2491–2497. PMID: 26304862.6. Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:227–276. PMID: 20966421.
Article7. Kono Y, Yamada S, Kamisaka K, Araki A, Fujioka Y, Yasui K, et al. Recurrence risk after noncardioembolic mild ischemic stroke in a Japanese population. Cerebrovasc Dis. 2011; 31:365–372. PMID: 21252505.
Article8. Elkind MS, Luna JM, McClure LA, Zhang Y, Coffey CS, Roldan A, et al. C-reactive protein as a prognostic marker after lacunar stroke: levels of inflammatory markers in the treatment of stroke study. Stroke. 2014; 45:707–716. PMID: 24523037.9. Kim GM, Park KY, Avery R, Helenius J, Rost N, Rosand J, et al. Extensive leukoaraiosis is associated with high early risk of recurrence after ischemic stroke. Stroke. 2014; 45:479–485. PMID: 24370756.
Article10. Cheng YY, Shu JH, Hsu HC, Liang Y, Chang ST, Kao CL, et al. The impact of rehabilitation frequencies in the first year after stroke on the risk of recurrent stroke and mortality. J Stroke Cerebrovasc Dis. 2017; 26:2755–2762. PMID: 28760410.
Article11. Park JH, Ovbiagele B. Relationship of functional disability after a recent stroke with recurrent stroke risk. Eur J Neurol. 2016; 23:361–367. PMID: 26493027.
Article12. Leidy NK. Functional status and the forward progress of merry-go-rounds: toward a coherent analytical framework. Nurs Res. 1994; 43:196–202. PMID: 8047422.13. Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995; 273:59–65. PMID: 7996652.
Article14. Ustün B, Kennedy C. What is “functional impairment?” Disentangling disability from clinical significance. World Psychiatry. 2009; 8:82–85. PMID: 19516924.15. Saunders DH, Greig CA, Mead GE. Physical activity and exercise after stroke: review of multiple meaningful benefits. Stroke. 2014; 45:3742–3747. PMID: 25370588.16. Chang WH, Sohn MK, Lee J, Kim DY, Lee SG, Shin YI, et al. Korean stroke cohort for functioning and rehabilitation (KOSCO): study rationale and protocol of a multi-centre prospective cohort study. BMC Neurol. 2015; 15:42. PMID: 25886039.
Article17. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993; 24:35–41. PMID: 7678184.
Article18. Schmidt M, Jacobsen JB, Johnsen SP, Bøtker HE, Sørensen HT. Eighteen-year trends in stroke mortality and the prognostic influence of comorbidity. Neurology. 2014; 82:340–350. PMID: 24363134.
Article19. Chang WH, Sohn MK, Lee J, Kim DY, Lee SG, Shin YI, et al. Predictors of functional level and quality of life at 6 months after a first-ever stroke: the KOSCO study. J Neurol. 2016; 263:1166–1177. PMID: 27113602.20. Fried L, Bernardini J, Piraino B. Charlson comorbidity index as a predictor of outcomes in incident peritoneal dialysis patients. Am J Kidney Dis. 2001; 37:337–342. PMID: 11157375.
Article21. Ovbiagele B, Lyden PD, Saver JL. VISTA Collaborators. Disability status at 1 month is a reliable proxy for final ischemic stroke outcome. Neurology. 2010; 75:688–692. PMID: 20733143.
Article22. Mehrholz J, Wagner K, Rutte K, Meissner D, Pohl M. Predictive validity and responsiveness of the functional ambulation category in hemiparetic patients after stroke. Arch Phys Med Rehabil. 2007; 88:1314–1319. PMID: 17908575.
Article23. Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB. Similar motor recovery of upper and lower extremities after stroke. Stroke. 1994; 25:1181–1188. PMID: 8202977.
Article24. Ancheta J, Husband M, Law D, Reding M. Initial functional independence measure score and interval post stroke help assess outcome, length of hospitalization, and quality of care. Neurorehabil Neural Repair. 2000; 14:127–134. PMID: 15470823.
Article25. Mungas D. In-office mental status testing: a practical guide. Geriatrics. 1991; 46:54–58. 636626. Enderby P, Crow E. Frenchay aphasia screening test: validity and comparability. Disabil Rehabil. 1996; 18:238–240. PMID: 8743301.
Article27. Kim J, Oh BM, Lee GJ, Lee SA, Chun SW, Han TR. Clinical factors associated with severity of post-stroke dysphagia. Brain Neurorehabil. 2011; 4:116–120.
Article28. Roger PR, Johnson-Greene D. Comparison of assessment measures for post-stroke depression. Clin Neuropsychol. 2009; 23:780–793. PMID: 19288333.
Article29. Golicki D, Niewada M, Buczek J, Karlińska A, Kobayashi A, Janssen MF, et al. Validity of EQ-5D-5L in stroke. Qual Life Res. 2015; 24:845–850. PMID: 25347978.
Article30. Toni D, Di Angelantonio E, Di Mascio MT, Vinisko R, Bath PM. PRoFESS Study Group. Types of stroke recurrence in patients with ischemic stroke: a substudy from the PRoFESS trial. Int J Stroke. 2014; 9:873–878. PMID: 24148608.
Article31. Omori T, Kawagoe M, Moriyama M, Yasuda T, Ito Y, Hyakuta T, et al. Multifactorial analysis of factors affecting recurrence of stroke in Japan. Asia Pac J Public Health. 2015; 27:NP333–NP340. PMID: 22500031.
Article32. Zhang C, Zhao X, Wang C, Liu L, Ding Y, Akbary F, et al. Prediction factors of recurrent ischemic events in one year after minor stroke. PLoS One. 2015; 10:e0120105. PMID: 25774939.
Article33. Magalhães R, Abreu P, Correia M, Whiteley W, Silva MC, Sandercock P. Functional status three months after the first ischemic stroke is associated with long-term outcome: data from a community-based cohort. Cerebrovasc Dis. 2014; 38:46–54. PMID: 25226861.
Article34. de Haan R, Limburg M, Bossuyt P, van der Meulen J, Aaronson N. The clinical meaning of Rankin ‘handicap’ grades after stroke. Stroke. 1995; 26:2027–2030. PMID: 7482643.
Article35. Kono Y, Kawajiri H, Kamisaka K, Kamiya K, Akao K, Asai C, et al. Predictive impact of daily physical activity on new vascular events in patients with mild ischemic stroke. Int J Stroke. 2015; 10:219–223. PMID: 25381835.
Article36. Ovbiagele B, Saver JL, Fredieu A, Suzuki S, Selco S, Rajajee V, et al. In-hospital initiation of secondary stroke prevention therapies yields high rates of adherence at follow-up. Stroke. 2004; 35:2879–2883. PMID: 15514170.
Article37. Kono Y, Yamada S, Yamaguchi J, Hagiwara Y, Iritani N, Ishida S, et al. Secondary prevention of new vascular events with lifestyle intervention in patients with noncardioembolic mild ischemic stroke: a single-center randomized controlled trial. Cerebrovasc Dis. 2013; 36:88–97. PMID: 24029303.
Article38. Ivey FM, Womack CJ, Kulaputana O, Dobrovolny CL, Wiley LA, Macko RF. A single bout of walking exercise enhances endogenous fibrinolysis in stroke patients. Med Sci Sports Exerc. 2003; 35:193–198. PMID: 12569203.
Article39. Tang J, Wan JY, Bailey JE. Performance of comorbidity measures to predict stroke and death in a community-dwelling, hypertensive Medicaid population. Stroke. 2008; 39:1938–1944. PMID: 18436883.
Article40. Tessier A, Finch L, Daskalopoulou SS, Mayo NE. Validation of the Charlson comorbidity index for predicting functional outcome of stroke. Arch Phys Med Rehabil. 2008; 89:1276–1283. PMID: 18586129.
Article41. Yeh HJ, Huang N, Chou YJ, Cheng SP, Lee WK, Lai CC, et al. Older age, low socioeconomic status, and multiple comorbidities lower the probability of receiving inpatient rehabilitation half a year after stroke. Arch Phys Med Rehabil. 2017; 98:707–715. PMID: 27633939.
Article42. Kyu HH, Bachman VF, Alexander LT, Mumford JE, Afshin A, Estep K, et al. Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013. BMJ. 2016; 354:i3857. PMID: 27510511.
Article43. Howard VJ, McDonnell MN. Physical activity in primary stroke prevention: just do it. Stroke. 2015; 46:1735–1739. PMID: 25882053.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in Epidemiological Trends and Rehabilitation Usage in Neurological Diseases in Korea: Stroke
- Erratum to: Impact of Functional Status on Noncardioembolic Ischemic Stroke Recurrence Within 1 Year: The Korean Stroke Cohort for Functioning and Rehabilitation Study
- Stroke Rehabilitation Fact Sheet in Korea
- The Impact of Cortical Cerebral Microinfarcts on Functional Outcomes in Patients With Ischemic Stroke
- Dual Antiplatelet Therapy after Noncardioembolic Ischemic Stroke or Transient Ischemic Attack: Pros and Cons