Yonsei Med J.
2015 May;56(3):832-837. 10.3349/ymj.2015.56.3.832.
Sparing Effects of Sufentanil on Epidural Ropivacaine in Elderly Patients Undergoing Transurethral Resection of Prostate Surgery
- Affiliations
-
- 1Department of Anesthesiology, the First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou, Zhejiang, P.R. China. yuh_li@qq.com
- 2Department of Anesthesiology, Shaoxing People's Hospital, Shaoxing, Zhejiang, P.R. China.
- 3Medical Research Center, Shaoxing People's Hospital, Shaoxing, Zhejiang, P.R. China.
- KMID: 2450361
- DOI: http://doi.org/10.3349/ymj.2015.56.3.832
Abstract
- PURPOSE
This study examined the sparing effect of sufentanil on the median effective concentration (EC50) of epidural ropivacaine in elderly patients undergoing elective transurethral resection of prostate (TURP).
MATERIALS AND METHODS
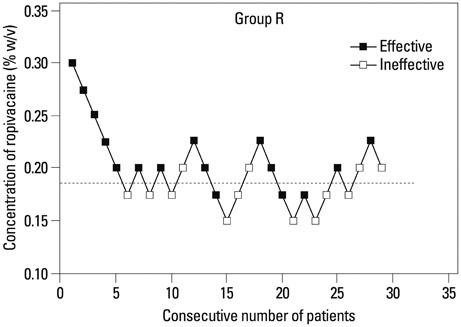
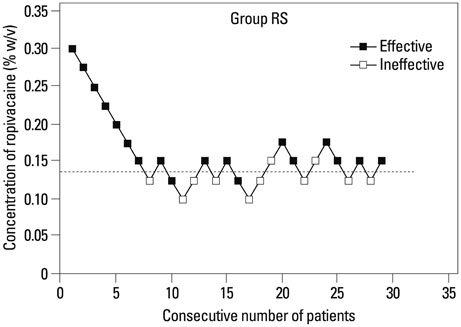
This was a prospective randomized double-blind dose-response study. Fifty eight elderly patients with American Society of Anesthesiologists physical status I-II who were scheduled for TURP surgery under epidural anesthesia were randomly allocated to a group receiving 15 mL of ropivacaine (group R) or a group receiving ropivacaine plus 5 microg of sufentanil (group RS). The concentration of ropivacaine was determined by a Dixon's up-and-down sequential allocation. The first participant received 0.3% of ropivacaine in both groups and subsequent concentrations were determined by the response of the previous patient in the same group. The EC50 of epidural ropivacaine was analyzed using the Dixon and Massey method.
RESULTS
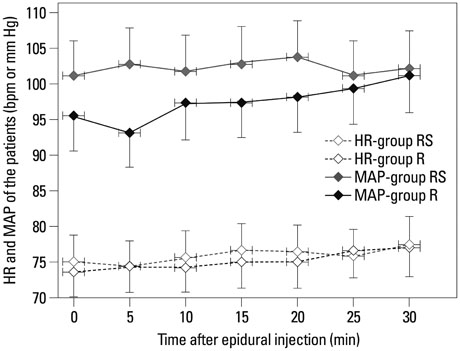
The EC50 of ropivacaine during TURP surgery was 0.186% (95% confidence interval, 0.173-0.200%) in group R, and 0.136% (95% confidence interval, 0.127-0.144%) in group RS (p<0.01). No differences in Bromage scale of motor block examination and the onset time of sensory block were observed.
CONCLUSION
Administration of 5 microg of epidural sufentanil caused a 37% reduction in the EC50 of epidural ropivacaine in elderly patients who underwent TURP surgery. Thus, sufentanil addition during surgery of TURP can decrease the dose of ropivacaine anesthesia required.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Amides/*administration & dosage
Anesthesia, Epidural/*methods
Anesthetics, Local/*administration & dosage
Dose-Response Relationship, Drug
Double-Blind Method
Humans
Male
Middle Aged
Pain Measurement
Prospective Studies
Sufentanil/*administration & dosage
*Transurethral Resection of Prostate
Treatment Outcome
Amides
Anesthetics, Local
Sufentanil
Figure
Reference
-
1. Nydahl PA, Philipson L, Axelsson K, Johansson JE. Epidural anesthesia with 0.5% bupivacaine: influence of age on sensory and motor blockade. Anesth Analg. 1991; 73:780–786.2. Simon MJ, Veering BT, Stienstra R, van Kleef JW, Burm AG. The effects of age on neural blockade and hemodynamic changes after epidural anesthesia with ropivacaine. Anesth Analg. 2002; 94:1325–1330.
Article3. Kuthiala G, Chaudhary G. Ropivacaine: a review of its pharmacology and clinical use. Indian J Anaesth. 2011; 55:104–110.
Article4. Chaudhary A, Bogra J, Singh PK, Saxena S, Chandra G, Verma R. Efficacy of spinal ropivacaine versus ropivacaine with fentanyl in transurethral resection operations. Saudi J Anaesth. 2014; 8:88–91.
Article5. Li Y, Zhu S, Bao F, Xu J, Yan X, Jin X. The effects of age on the median effective concentration of ropivacaine for motor blockade after epidural anesthesia with ropivacaine. Anesth Analg. 2006; 102:1847–1850.
Article6. Lyons G, Columb M, Hawthorne L, Dresner M. Extradural pain relief in labour: bupivacaine sparing by extradural fentanyl is dose dependent. Br J Anaesth. 1997; 78:493–497.
Article7. Polley LS, Columb MO, Wagner DS, Naughton NN. Dose-dependent reduction of the minimum local analgesic concentration of bupivacaine by sufentanil for epidural analgesia in labor. Anesthesiology. 1998; 89:626–632.
Article8. Robinson AP, Lyons GR, Wilson RC, Gorton HJ, Columb MO. Levobupivacaine for epidural analgesia in labor: the sparing effect of epidural fentanyl. Anesth Analg. 2001; 92:410–414.
Article9. Lee YY, Ngan Kee WD, Muchhal K, Chan CK. Randomized double-blind comparison of ropivacaine-fentanyl and bupivacaine-fentanyl for spinal anaesthesia for urological surgery. Acta Anaesthesiol Scand. 2005; 49:1477–1482.
Article10. Unlugenc H, Ozalevli M, Gunduz M, Gunasti S, Urunsak IF, Guler T, et al. Comparison of intrathecal magnesium, fentanyl, or placebo combined with bupivacaine 0.5% for parturients undergoing elective cesarean delivery. Acta Anaesthesiol Scand. 2009; 53:346–353.
Article11. Braga Ade F, Braga FS, Potério GM, Pereira RI, Reis E, Cremonesi E. Sufentanil added to hyperbaric bupivacaine for subarachnoid block in Caesarean section. Eur J Anaesthesiol. 2003; 20:631–635.
Article12. Oğün CO, Kirgiz EN, Duman A, Okesli S, Akyürek C. Comparison of intrathecal isobaric bupivacaine-morphine and ropivacaine-morphine for Caesarean delivery. Br J Anaesth. 2003; 90:659–664.13. Wang LZ, Zhang YF, Tang BL, Yao KZ. Effects of intrathecal and i.v. small-dose sufentanil on the median effective dose of intrathecal bupivacaine for Caesarean section. Br J Anaesth. 2007; 98:792–796.
Article14. Leysen JE, Gommeren W, Niemegeers CJ. [3H]Sufentanil, a superior ligand for mu-opiate receptors: binding properties and regional distribution in rat brain and spinal cord. Eur J Pharmacol. 1983; 87:209–225.
Article15. Grass JA, Sakima NT, Schmidt R, Michitsch R, Zuckerman RL, Harris AP. A randomized, double-blind, dose-response comparison of epidural fentanyl versus sufentanil analgesia after cesarean section. Anesth Analg. 1997; 85:365–371.
Article16. Olofsson C, Nygårds EB, Bjersten AB, Hessling A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004; 48:1240–1244.
Article17. Meininger D, Byhahn C, Kessler P, Nordmeyer J, Alparslan Y, Hall BA, et al. Intrathecal fentanyl, sufentanil, or placebo combined with hyperbaric mepivacaine 2% for parturients undergoing elective cesarean delivery. Anesth Analg. 2003; 96:852–858.18. Dahlgren G, Hultstrand C, Jakobsson J, Norman M, Eriksson EW, Martin H. Intrathecal sufentanil, fentanyl, or placebo added to bupivacaine for cesarean section. Anesth Analg. 1997; 85:1288–1293.
Article19. Polley LS, Columb MO, Lyons G, Nair SA. The effect of epidural fentanyl on the minimum local analgesic concentration of epidural chloroprocaine in labor. Anesth Analg. 1996; 83:987–990.
Article20. Palm S, Gertzen W, Ledowski T, Gleim M, Wulf H. Minimum local analgesic dose of plain ropivacaine vs. ropivacaine combined with sufentanil during epidural analgesia for labour. Anaesthesia. 2001; 56:526–529.
Article21. Buyse I, Stockman W, Columb M, Vandermeersch E, Van de Velde M. Effect of sufentanil on minimum local analgesic concentrations of epidural bupivacaine, ropivacaine and levobupivacaine in nullipara in early labour. Int J Obstet Anesth. 2007; 16:22–28.
Article22. Chen X, Qian X, Fu F, Lu H, Bein B. Intrathecal sufentanil decreases the median effective dose (ED50) of intrathecal hyperbaric ropivacaine for caesarean delivery. Acta Anaesthesiol Scand. 2010; 54:284–290.
Article23. Parpaglioni R, Baldassini B, Barbati G, Celleno D. Adding sufentanil to levobupivacaine or ropivacaine intrathecal anaesthesia affects the minimum local anaesthetic dose required. Acta Anaesthesiol Scand. 2009; 53:1214–1220.
Article24. Boulier V, Gomis P, Lautner C, Visseaux H, Palot M, Malinovsky JM. Minimum local analgesic concentrations of ropivacaine and levobupivacaine with sufentanil for epidural analgesia in labour. Int J Obstet Anesth. 2009; 18:226–230.
Article25. Wulf HF. Up-down sequential allocation technique to investigate the influence of opioids on the efficacy of epidural local anesthetics in labor pain. Anesthesiology. 1999; 90:1788–1789.
Article26. Capogna G, Celleno D, Laudano D, Giunta F. Alkalinization of local anesthetics. Which block, which local anesthetic? Reg Anesth. 1995; 20:369–377.27. Bromage PR. A comparison of the hydrochloride and carbon dioxide salts of lidocaine and prilocaine in epidural analgesia. Acta Anaesthesiol Scand Suppl. 1965; 16:55–69.
Article28. Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Writing Committee, the American Urological Association. Transurethral prostatectomy: immediate and postoperative complications. Cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol, 141: 243-247, 1989. J Urol. 2002; 167:5–9.
Article29. Ozmen S, Koşar A, Soyupek S, Armağan A, Hoşcan MB, Aydin C. The selection of the regional anaesthesia in the transurethral resection of the prostate (TURP) operation. Int Urol Nephrol. 2003; 35:507–512.
Article30. Dobson PM, Caldicott LD, Gerrish SP, Cole JR, Channer KS. Changes in haemodynamic variables during transurethral resection of the prostate: comparison of general and spinal anaesthesia. Br J Anaesth. 1994; 72:267–271.
Article31. Meyer RA, Macarthur AJ, Downey K. Study of equivalence: spinal bupivacaine 15 mg versus bupivacaine 12 mg with fentanyl 15 µg for cesarean delivery. Int J Obstet Anesth. 2012; 21:17–23.
Article32. Erturk E, Bostan H, Eroglu A. Epidural analgesia and vaginal delivery in a patient with aortic stenosis and insufficiency. Med Princ Pract. 2011; 20:574–576.
Article33. Congedo E, Sgreccia M, De Cosmo G. New drugs for epidural analgesia. Curr Drug Targets. 2009; 10:696–706.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Epidural Analgesia using 0.1% Levobupivacaine or 0.1% Ropivacaine Combined with Sufentanil in Gynecologic Surgery
- Selective Spinal Anesthesia Using 1 mg of Bupivacaine with Opioid in Elderly Patients for Transurethral Resection of Prostate
- Comparison of Sufentanil and Fentanyl Added to Ropivacaine for Patient-Controlled Thoracic Epidural Analgesia
- The Efficacy of Epidural Ketamine on Shivering during Transurethral Resection of the Prostate under Epidural Anesthesia
- Comparison of Sufentanil and Morphine with Ropivacaine for Patient-controlled Epidural Analgesia after Gastrectomy