Yonsei Med J.
2015 May;56(3):737-743. 10.3349/ymj.2015.56.3.737.
Retrospective Assessment of the Validity of Robotic Surgery in Comparison to Open Surgery for Pediatric Choledochal Cyst
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Anesthesia and Pain Research Institute, Yonsei University College of Medicine, Seoul, Korea. sjbai1@yuhs.ac
- 2Department of Pediatric Surgery, Severance Children's Hospital, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. sjhan@yuhs.ac
- 3Biostatistics Collaboration Unit, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2450348
- DOI: http://doi.org/10.3349/ymj.2015.56.3.737
Abstract
- PURPOSE
We evaluated the validity of robotic surgery (RS) for pediatric choledochal cyst (CC) in comparison to open surgery (OS).
MATERIALS AND METHODS
From January 2009 to April 2013, clinical data from 79 consecutive pediatric patients with CC, who underwent RS (n=36) or OS (n=43) performed by a single pediatric surgeon, were analyzed retrospectively.
RESULTS
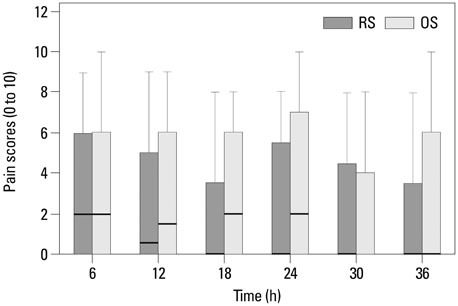
In the RS group, the age of the patients was significantly older, compared to the OS group. Operation and anesthesia times were significantly longer in the RS group than the OS group. Fluid input rates to maintain the same urine output were significantly smaller in the RS group than the OS group. The American Society of Anesthesiologists (ASA) physical status, length of postoperative hospital stay, and the incidence of surgical complications did not differ significantly between the two groups.
CONCLUSION
Although early complications could not be avoided during the development of robotic surgical techniques, RS for pediatric CC showed results comparable to those for OS. We believe that RS may be a valid and alternative surgery for pediatric CC. After further development of robotic surgical systems and advancement of surgical techniques therewith, future prospective studies may reveal more positive results.
Keyword
MeSH Terms
-
Age Distribution
Aged, 80 and over
Child
Child, Preschool
Choledochal Cyst/*surgery
Female
Humans
Incidence
Infant
Length of Stay/statistics & numerical data
Male
Minimally Invasive Surgical Procedures/*methods
Postoperative Complications/epidemiology
Postoperative Period
Prospective Studies
Reproducibility of Results
Retrospective Studies
*Robotics
Treatment Outcome
Figure
Cited by 1 articles
-
Comparison of long-term biliary complications between open and laparoscopic choledochal cyst excision in children
Changhoon Lee, Jeik Byun, Dayoung Ko, Hee-Beom Yang, Joong Kee Youn, Hyun-Young Kim
Ann Surg Treat Res. 2021;100(3):186-192. doi: 10.4174/astr.2021.100.3.186.
Reference
-
1. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359.
Article2. de Vries JS, de Vries S, Aronson DC, Bosman DK, Rauws EA, Bosma A, et al. Choledochal cysts: age of presentation, symptoms, and late complications related to Todani's classification. J Pediatr Surg. 2002; 37:1568–1573.
Article3. Bhavsar MS, Vora HB, Giriyappa VH. Choledochal cysts: a review of literature. Saudi J Gastroenterol. 2012; 18:230–236.4. Dawrant MJ, Najmaldin AS, Alizai NK. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children less than 10 kg. J Pediatr Surg. 2010; 45:2364–2368.
Article5. Akaraviputh T, Trakarnsanga A, Suksamanapun N. Robot-assisted complete excision of choledochal cyst type I, hepaticojejunostomy and extracorporeal Roux-en-y anastomosis: a case report and review literature. World J Surg Oncol. 2010; 8:87.
Article6. Chang EY, Hong YJ, Chang HK, Oh JT, Han SJ. Lessons and tips from the experience of pediatric robotic choledochal cyst resection. J Laparoendosc Adv Surg Tech A. 2012; 22:609–614.
Article7. Dangle PP, Kearns J, Anderson B, Gundeti MS. Outcomes of infants undergoing robot-assisted laparoscopic pyeloplasty compared to open repair. J Urol. 2013; 190:2221–2226.
Article8. Bao PQ, Mazirka PO, Watkins KT. Retrospective comparison of robot-assisted minimally invasive versus open pancreaticoduodenectomy for periampullary neoplasms. J Gastrointest Surg. 2014; 18:682–689.
Article9. Diao M, Li L, Cheng W. To drain or not to drain in Roux-en-Y hepatojejunostomy for children with choledochal cysts in the laparoscopic era: a prospective randomized study. J Pediatr Surg. 2012; 47:1485–1489.
Article10. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358.11. Alqahtani A, Albassam A, Zamakhshary M, Shoukri M, Altokhais T, Aljazairi A, et al. Robot-assisted pediatric surgery: how far can we go? World J Surg. 2010; 34:975–978.
Article12. Meehan JJ, Elliott S, Sandler A. The robotic approach to complex hepatobiliary anomalies in children: preliminary report. J Pediatr Surg. 2007; 42:2110–2114.
Article13. Alizai NK, Dawrant MJ, Najmaldin AS. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr Surg Int. 2014; 30:291–294.
Article14. van Haasteren G, Levine S, Hayes W. Pediatric robotic surgery: early assessment. Pediatrics. 2009; 124:1642–1649.
Article15. Meehan JJ, Sandler A. Pediatric robotic surgery: a single-institutional review of the first 100 consecutive cases. Surg Endosc. 2008; 22:177–182.
Article16. Miyano T, Yamataka A, Kato Y, Segawa O, Lane G, Takamizawa S, et al. Hepaticoenterostomy after excision of choledochal cyst in children: a 30-year experience with 180 cases. J Pediatr Surg. 1996; 31:1417–1421.
Article17. She WH, Chung HY, Lan LC, Wong KK, Saing H, Tam PK. Management of choledochal cyst: 30 years of experience and results in a single center. J Pediatr Surg. 2009; 44:2307–2311.
Article18. Darzi SA, Munz Y. The impact of minimally invasive surgical techniques. Annu Rev Med. 2004; 55:223–237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Initial Experience of Robot-assisted Resection of Choledochal Cyst in Children
- A case of type IVa choledochal cyst
- A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
- Comparison of surgical outcomes of intracorporeal hepaticojejunostomy in the excision of choledochal cysts using laparoscopic versus robot techniques
- Comparison of long-term biliary complications between open and laparoscopic choledochal cyst excision in children