Ann Surg Treat Res.
2021 Mar;100(3):186-192. 10.4174/astr.2021.100.3.186.
Comparison of long-term biliary complications between open and laparoscopic choledochal cyst excision in children
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Pediatric Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2513199
- DOI: http://doi.org/10.4174/astr.2021.100.3.186
Abstract
- Purpose
Cyst excision with hepaticojejunostomy has been the classic procedure for treating choledochal cysts, and the use of laparoscopic treatment has been favored recently. The purpose of this study was to compare the long-term biliary complication of laparoscopic operation with open surgery for choledochal cyst presenting in children.
Methods
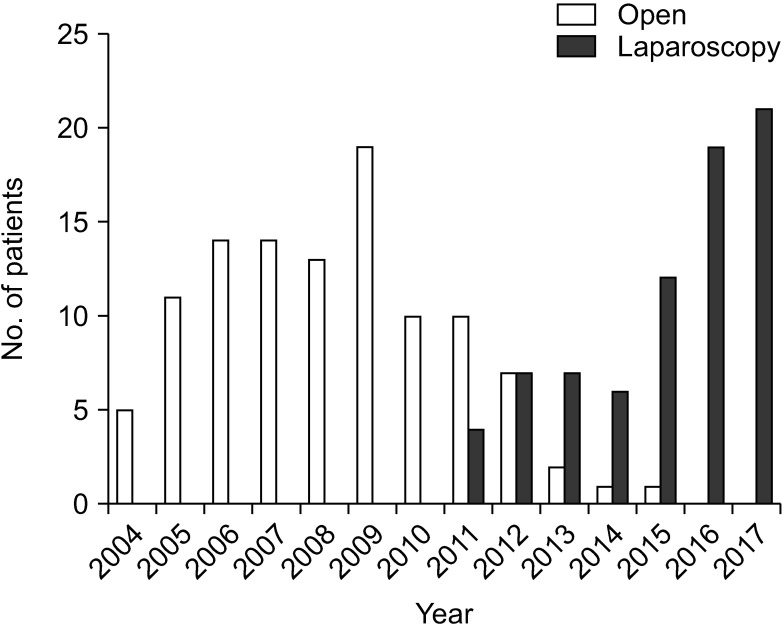
A retrospective study comparing the laparoscopic and open procedures was performed in 185 patients with choledochal cyst in a single children’s hospital. There were 109 patients who were operated with open surgery, and 76 patients operated with laparoscopic surgery. The primary outcome was long-term biliary complications and the secondary outcome included operative time, intraoperative transfusion, length of hospital stay, and other late postoperative complications.
Results
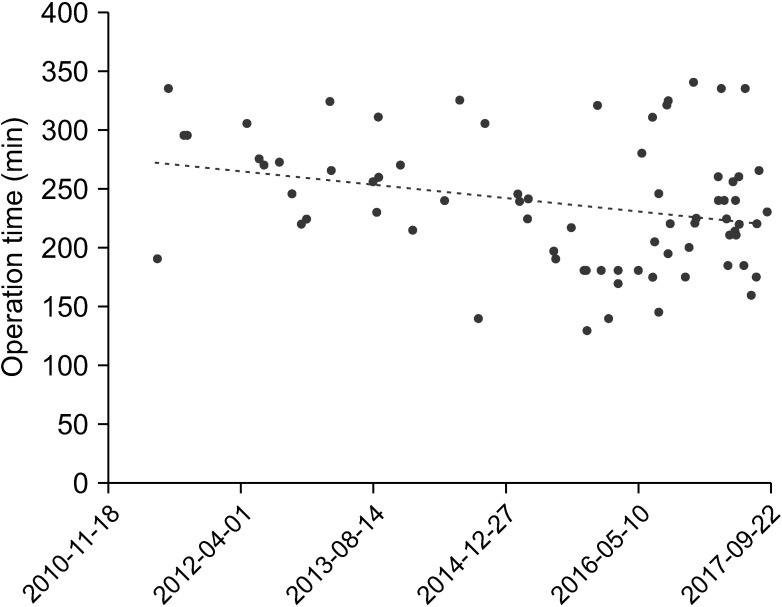
In the patient’s demographics, there was no significant difference between the 2 groups. Notably, it was shown that the operative time was longer in the laparoscopic group. The number of patients requiring blood transfusion intraoperatively was lower in the laparoscopic group. It was noted that the hospital stay was not statistically different. The duration to resumption of diet and duration of drainage were longer in the laparoscopic group. Biliary complications were shown to be significantly higher in the open group. The risk factor for long-term biliary complications was noted with the intraoperative transfusion.
Conclusion
The use of a laparoscopic choledochal cyst excision with hepaticojejunostomy is a safe and feasible technique in a young patient. The long-term biliary complication was lower compared to open surgery, rendering this a good option for pediatric patients.
Keyword
Figure
Reference
-
1. Vater A, Ezler CS. Dissertatio de Scirrhis viscerum occasione sectionis viri tympanite defunte. Wittenburgae. 1723; 881:22.2. Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977; 134:263–269. PMID: 889044.3. Lipsett PA, Pitt HA. Surgical treatment of choledochal cysts. J Hepatobiliary Pancreat Surg. 2003; 10:352–359. PMID: 14598135.
Article4. Farello GA, Cerofolini A, Rebonato M, Bergamaschi G, Ferrari C, Chiappetta A. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc. 1995; 5:354–358. PMID: 8845978.5. Lee JH, Kim SH, Kim HY, Choi YH, Jung SE, Park KW. Early experience of laparoscopic choledochal cyst excision in children. J Korean Surg Soc. 2013; 85:225–229. PMID: 24266013.
Article6. Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:15–26. PMID: 17252293.
Article7. Shen HJ, Xu M, Zhu HY, Yang C, Li F, Li KW, et al. Laparoscopic versus open surgery in children with choledochal cysts: a meta-analysis. Pediatr Surg Int. 2015; 31:529–534. PMID: 25895070.
Article8. Park SW, Koh H, Oh JT, Han SJ, Kim S. Relationship between anomalous pancreaticobiliary ductal union and pathologic inflammation of bile duct in choledochal cyst. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:170–177. PMID: 25349833.
Article9. Yeung F, Chung PH, Wong KK, Tam PK. Biliary-enteric reconstruction with hepaticoduodenostomy following laparoscopic excision of choledochal cyst is associated with better postoperative outcomes: a single-centre experience. Pediatr Surg Int. 2015; 31:149–153. PMID: 25433691.
Article10. Lee KH, Tam YH, Yeung CK, Chan KW, Sihoe JD, Cheung ST, et al. Laparoscopic excision of choledochal cysts in children: an intermediate-term report. Pediatr Surg Int. 2009; 25:355–360. PMID: 19255762.11. Jang JY, Yoon YS, Kang MJ, Kwon W, Park JW, Chang YR, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc. 2013; 27:1648–1652. PMID: 23239299.
Article12. Kim NY, Chang EY, Hong YJ, Park S, Kim HY, Bai SJ, et al. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J. 2015; 56:737–743. PMID: 25837180.
Article13. Margonis GA, Spolverato G, Kim Y, Marques H, Poultsides G, Maithel S, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg. 2015; 19:858–865. PMID: 25519084.
Article14. Diao M, Li L, Cheng W. Recurrence of biliary tract obstructions after primary laparoscopic hepaticojejunostomy in children with choledochal cysts. Surg Endosc. 2016; 30:3910–3915. PMID: 26659232.
Article15. Diao M, Li L, Cheng W. Laparoscopic redo hepaticojejunostomy for children with choledochal cysts. Surg Endosc. 2016; 30:5513–5519. PMID: 27126624.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of laparoscopic excision of choledochal cyst, hepaticojejunostomy, and Roux-en-Y anastomosis using Artisential®
- A case of type IVa choledochal cyst
- Development of Cholangiocarcinoma Arising from Remnant Intrapancreatic Cyst 15 Years after Choledochal Cyst Excision
- Robot-assisted Excision of a Huge Choledochal Cyst and Roux-en-Y Hepaticojejunostomy using the da Vinci(TM) Surgical System
- Type IV-A Choledochal Cyst with Intrahepatic Bile Duct Stricture