Clin Endosc.
2019 May;52(3):278-282. 10.5946/ce.2018.114.
Primary Gastric Small Cell Carcinoma (Presenting as Linitis Plastica) Diagnosed Using Endoscopic Ultrasound-Guided Biopsy: A Case Report
- Affiliations
-
- 1Department of Internal Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea. imdrkim@naver.com
- 2Department of Surgery, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju, Korea.
- KMID: 2449770
- DOI: http://doi.org/10.5946/ce.2018.114
Abstract
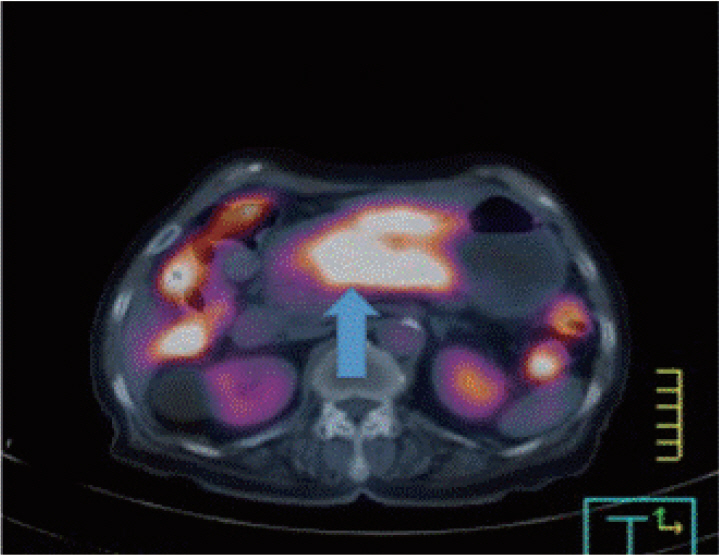
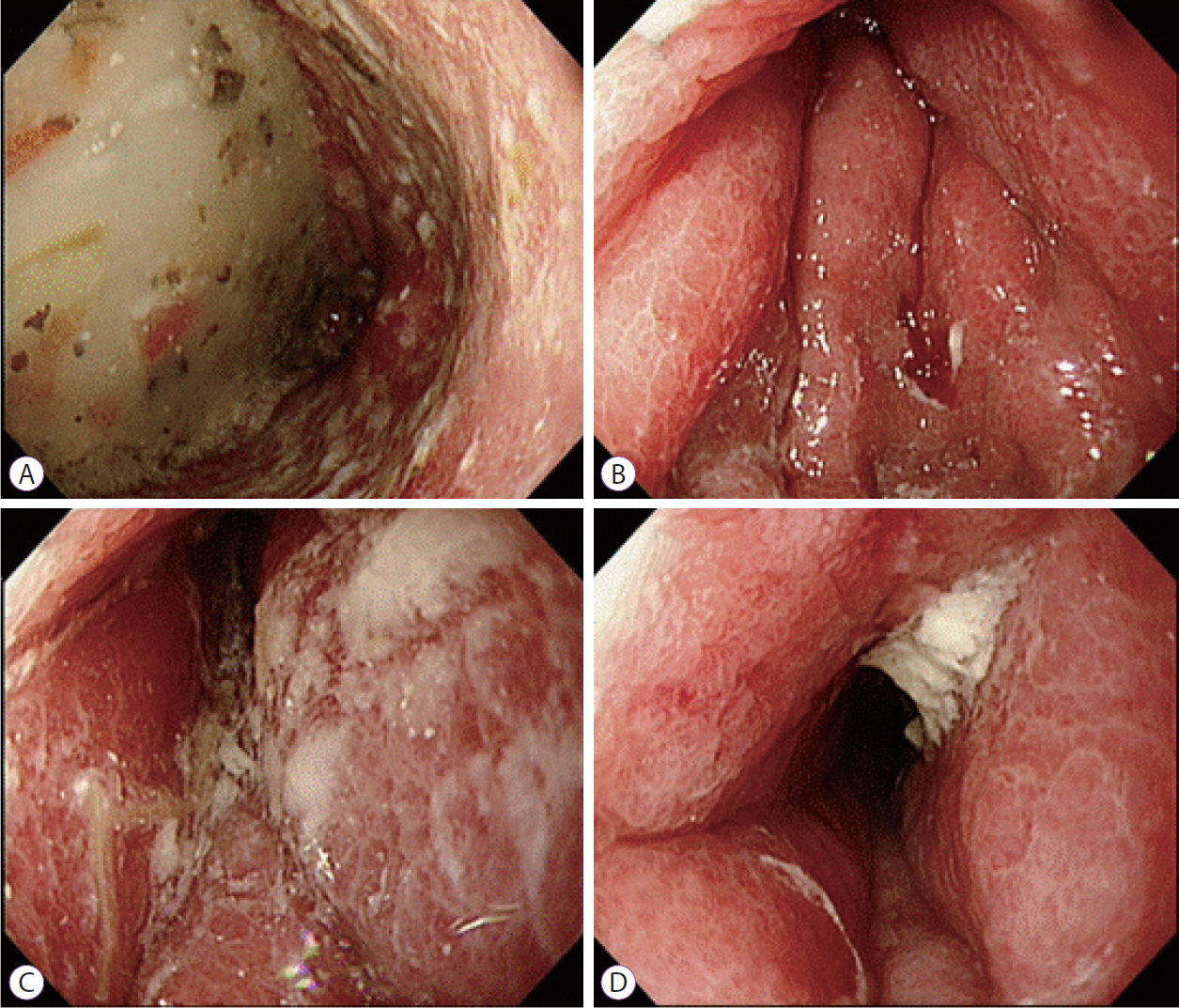
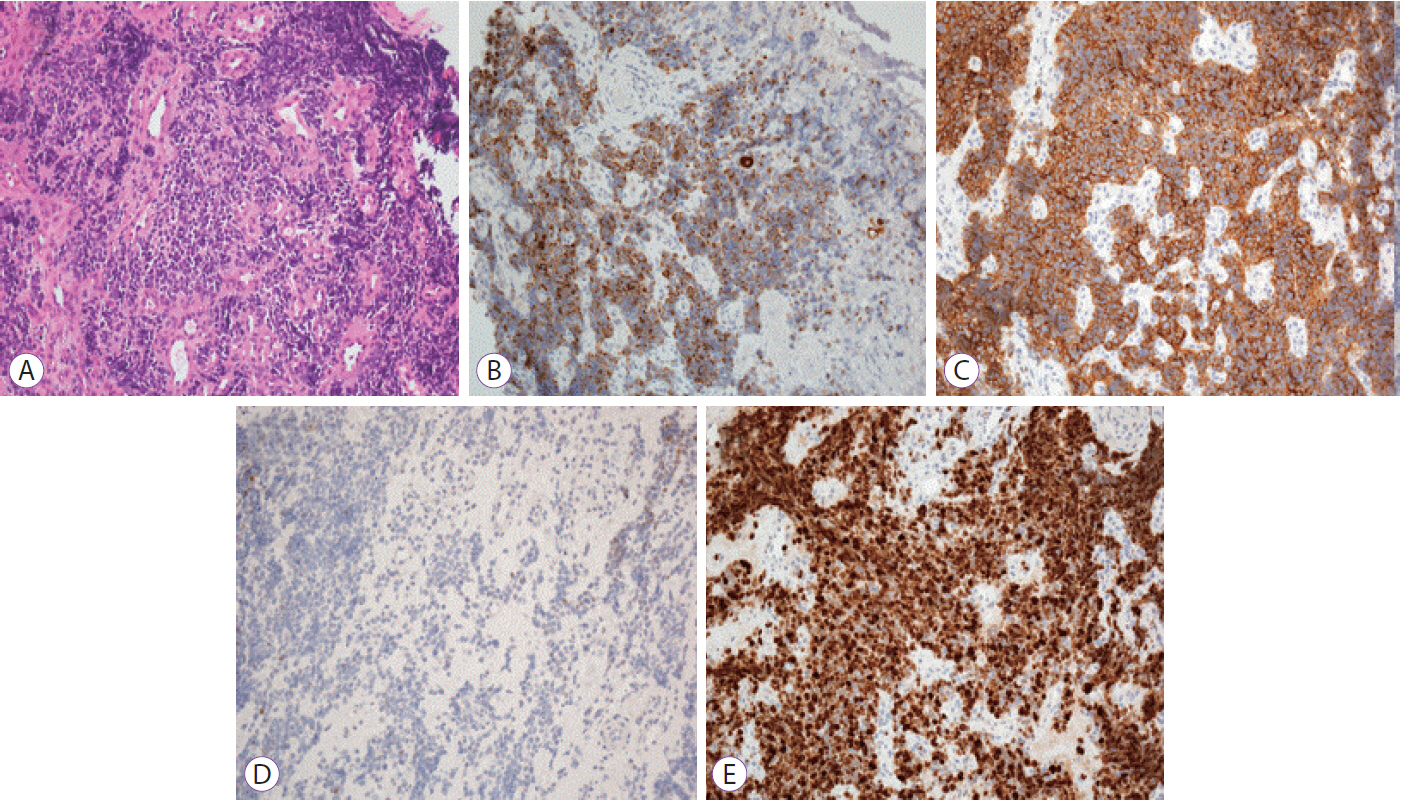
- Small cell carcinomas are the most aggressive, highly malignant neuroendocrine tumors; among these, gastric small cell carcinoma (GSCC) is extremely rare. Here we report a case of a patient with primary GSCC, presenting as linitis plastic, who was diagnosed using endoscopic ultrasound (EUS)-guided biopsy. With undiagnosed linitis plastica, an 80-year-old woman was referred to our institution. Abdominal computed tomography revealed irregular wall thickening extending from the gastric body to the antrum. Endoscopy suspected to have Borrmann type IV advanced gastric cancer. EUS of the stomach showed diffuse submucosal thickening of the gastric wall, mainly the antrum. EUS-guided bite-on-bite biopsy confirmed the diagnosis of GSCC. In general, GSCC is difficult to diagnose and careful examination is necessary to determine the therapeutic strategy; however, EUS is particularly helpful in the differential diagnosis of a lesion presenting as linitis plastica.
MeSH Terms
Figure
Reference
-
1. Kim KO, Lee HY, Chun SH, et al. Clinical overview of extrapulmonary small cell carcinoma. J Korean Med Sci. 2006; 21:833–837.
Article2. Wu QQ, Qiang WG, Wang F, et al. Management of primary gastric small cell carcinoma in China. Int J Clin Exp Med. 2015; 8:1589–1597.3. Namikawa T, Kobayashi M, Okabayashi T, et al. Primary gastric small cell carcinoma: report of a case and review of the literature. Med Mol Morphol. 2005; 38:256–261.
Article4. Arai K, Matsuda M. Gastric small-cell carcinoma in Japan: a case report and review of the literature. Am J Clin Oncol. 1998; 21:458–461.5. Fukuda T, Ohnishi Y, Nishimaki T, Ohtani H, Tachikawa S. Early gastric cancer of the small cell type. Am J Gastroenterol. 1988; 83:1176–1179.6. Frances N, Zeichner SB, Francavilla M, Cusnir M. Gastric small-cell carcinoma found on esophagogastroduodenoscopy: a case report and literature review. Case Rep Oncol Med. 2013; 2013:475961.
Article7. Matsusaka T, Watanabe H, Enjoji M. Anaplastic carcinoma of the esophagus. Report of three cases and their histogenetic consideration. Cancer. 1976; 37:1352–1358.
Article8. Matsusaka T, Watanabe H, Enjoji M. Oat-cell carcinoma of the stomach. Fukuoka Igaku Zasshi. 1976; 67:65–73.9. Kusayanagi S, Konishi K, Miyasaka N, et al. Primary small cell carcinoma of the stomach. J Gastroenterol Hepatol. 2003; 18:743–747.
Article10. Chambers LA, Clark WE 2nd. The endoscopic diagnosis of gastroesophageal malignancy. A cytologic review. Acta Cytol. 1986; 30:110–114.11. Bohle W, Scheidig A, Zoller WG. Endosonographic tumor staging for treatment decision in resectable gastric cancer. J Gastrointestin Liver Dis. 2011; 20:135–139.
Article12. Vetro C, Chiarenza A, Romano A, et al. Prognostic assessment and treatment of primary gastric lymphomas: how endoscopic ultrasonography can help in tailoring patient management. Clin Lymphoma Myeloma Leuk. 2014; 14:179–185.13. Songur Y, Okai T, Watanabe H, et al. Endosonographic features of a calcified mucinous gastric carcinoma. Endoscopy. 1995; 27:347.
Article14. Matsui T, Kataoka M, Sugita Y, et al. A case of small cell carcinoma of the stomach. Hepatogastroenterology. 1997; 44:156–160.15. Brenner B, Tang LH, Klimstra DS, Kelsen DP. Small-cell carcinomas of the gastrointestinal tract: a review. J Clin Oncol. 2004; 22:2730–2739.
Article16. Nakamura Y, Otani S, Otaka M, et al. Gastric small cell carcinoma with marked response to neoadjuvant chemotherapy. Int J Clin Oncol. 2005; 10:348–352.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary Linitis Plastica of the Rectum: A Clinico-Pathologic Analysis of Five Cases with Special Reference to Comparison with Gastric Form
- Metastatic Gastric Linitis Plastica from Bladder Cancer Mimicking a Primary Gastric Carcinoma: a Case Report
- A Case of Mantle Cell Lymphoma Exhibiting Features of Gastric Linitis Plastica Type of Advanced Gastric Cancer
- Primary Linitis Plastica of the Colon with Mucinous Adenocarcinoma in Young Woman
- Synchronously Diagnosed Gastric Metastasis from Invasive Lobular Breast Carcinoma, Mimicking Primary Gastric Carcinoma