J Korean Ophthalmol Soc.
2019 Jun;60(6):594-599. 10.3341/jkos.2019.60.6.594.
Primary Intraocular T-cell Lymphoma
- Affiliations
-
- 1Department of Ophthalmology, Chungnam National University College of Medicine, Daejeon, Korea. youngjoonjo@gmail.com
- 2Department of Pathology, Chungnam National University College of Medicine, Daejeon, Korea.
- KMID: 2449714
- DOI: http://doi.org/10.3341/jkos.2019.60.6.594
Abstract
- PURPOSE
Intraocular lymphoma can be divided into primary and secondary usually involving B-cell lymphoma. Intraocular T-cell lymphoma is mostly secondary lymphoma while primary intraocular T-cell lymphoma is extremely rare. We report a case of primary T-cell lymphoma.
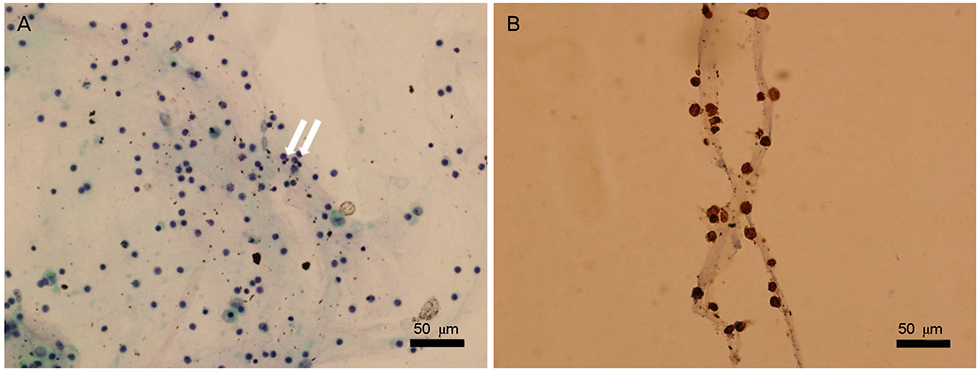
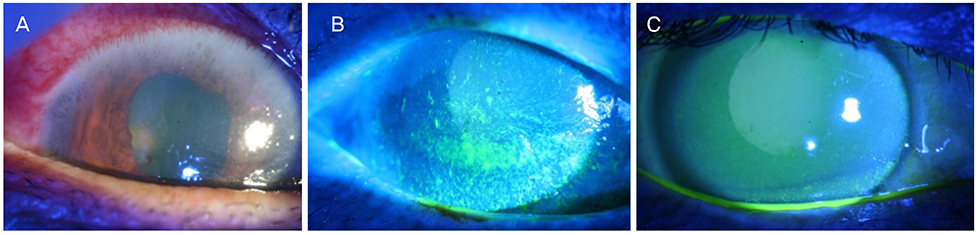
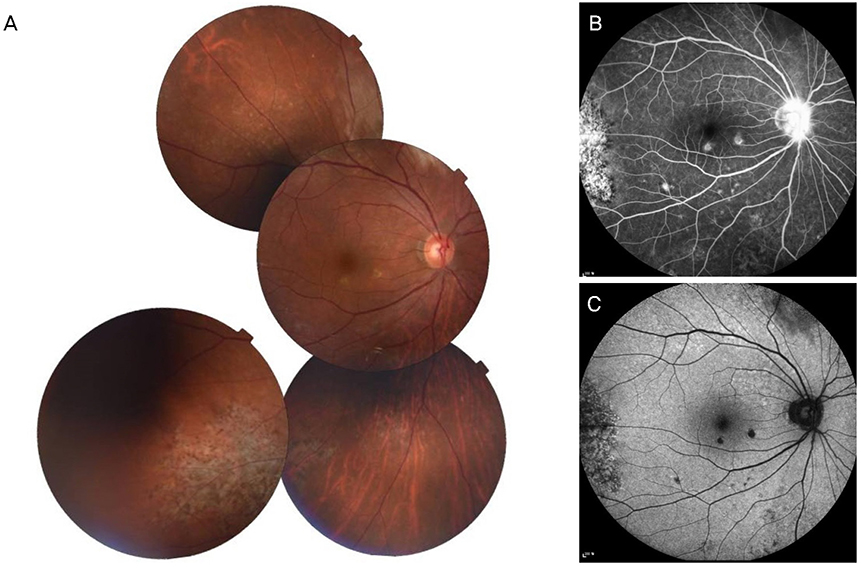
CASE SUMMARY
A 62-year-old male without any systemic disease presented with a floater in the right eye. A fundus examination showed multiple whitish retinal infiltrations in the right eye. Intraocular lymphoma was suspected, and systemic examination was performed, but all results were normal. During steroid treatment, previous lesions were enlarged, new lesions developed, and a diagnosis of primary T-cell lymphoma was made by diagnostic vitrectomy. Consecutive intravitreal injections of methotrexate were performed. After eight injections, the vitreous and retinal lesions improved but we decided to terminate the injections due to corneal epitheliopathy. The corneal epitheliopathy was recovered and the patient is currently undergoing periodic follow-ups without progression of the lesion.
CONCLUSIONS
Although intraocular T-cell lymphoma is a rare condition, this primary T-cell type should be considered when an intraocular lymphoma lesion is suspected.
MeSH Terms
Figure
Reference
-
1. Hong JT, Chae JB, Lee JY, et al. Ocular involvement in patients with primary CNS lymphoma. J Neurooncol. 2011; 102:139–145.2. Suh MH, Yu HG. Clinical manifestations of intraocular lymphoma. J Korean Ophthalmol Soc. 2009; 50:78–84.3. Chaput F, Amer R, Baglivo E, et al. Intraocular T-cell lymphoma: clinical presentation, diagnosis, treatment, and outcome. Ocul Immunol Inflamm. 2017; 25:639–648.4. Hunyor AP, Harper CA, O'Day J, McKelvie PA. Ocular-central nervous system lymphoma mimicking posterior scleritis with exudative retinal detachment. Ophthalmology. 2000; 107:1955–1959.5. Saga T, Ohno S, Matsuda H, et al. Ocular involvement by a peripheral T-cell lymphoma. Arch Ophthalmol. 1984; 102:399–402.6. Lobo A, Larkin G, Clark BJ, et al. Pseudo-hypopyon as the presenting feature in B-cell and T-cell intraocular lymphoma. Clin Exp Ophthalmol. 2003; 31:155–158.7. Char DH, Ljung BM, Deschênes J, Miller TR. Intraocular lymphoma: immunological and cytological analysis. Br J Ophthalmol. 1988; 72:905–911.8. Reddy EK, Bhatia P, Evans RG. Primary orbital lymphomas. Int J Radiat Oncol Biol Phys. 1988; 15:1239–1241.9. Turaka K, Bryan JS, De Souza S, et al. Vitreoretinal lymphoma: changing trends in diagnosis and local treatment modalities at a single institution. Clin Lymphoma Myeloma Leuk. 2012; 12:412–417.10. Hoffman PM, Mckelvie P, Hall AJ, et al. Intraocular lymphoma: a series of 14 patients with clinicopathological features and treatment outcomes. Eye (Lond). 2003; 17:513–521.11. Whitcup SM, de Smet MD, Rubin BI, et al. Intraocular lymphoma. Clinical and histopathologic diagnosis. Ophthalmology. 1993; 100:1399–1406.12. Sagoo MS, Mehta H, Swampillai AJ, et al. Primary intraocular lymphoma. Surv Ophthalmol. 2014; 59:503–516.13. Smith JR, Rosenbaum JT, Wilson DJ, et al. Role of intravitreal methotrexate in the management of primary central nervous system lymphoma with ocular involvement. Ophthalmology. 2002; 109:1709–1716.14. Frenkel S, Hendler K, Siegal T, et al. Intravitreal methotrexate for treating vitreoretinal lymphoma: 10 years of experience. Br J Ophthalmol. 2008; 92:383–388.
Article15. Gorovoy I, Prechanond T, Abia M, et al. Toxic corneal epitheliopathy after intravitreal methotrexate and its treatment with oral folic acid. Cornea. 2013; 32:1171–1173.
Article