Ann Rehabil Med.
2019 Apr;43(2):129-141. 10.5535/arm.2019.43.2.129.
Intensive Rehabilitation Therapy Following Brain Tumor Surgery: A Pilot Study of Effectiveness and Long-Term Satisfaction
- Affiliations
-
- 1Department of Rehabilitation Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. kmin@cha.ac.kr
- 2Rehabilitation and Regeneration Research Center, CHA University, Seongnam, Korea.
- 3Department of Neurosurgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
- KMID: 2448995
- DOI: http://doi.org/10.5535/arm.2019.43.2.129
Abstract
OBJECTIVE
To evaluate the effectiveness of intensive rehabilitation to support recovery of neurological function after brain tumor surgery and assess long-term satisfaction.
METHODS
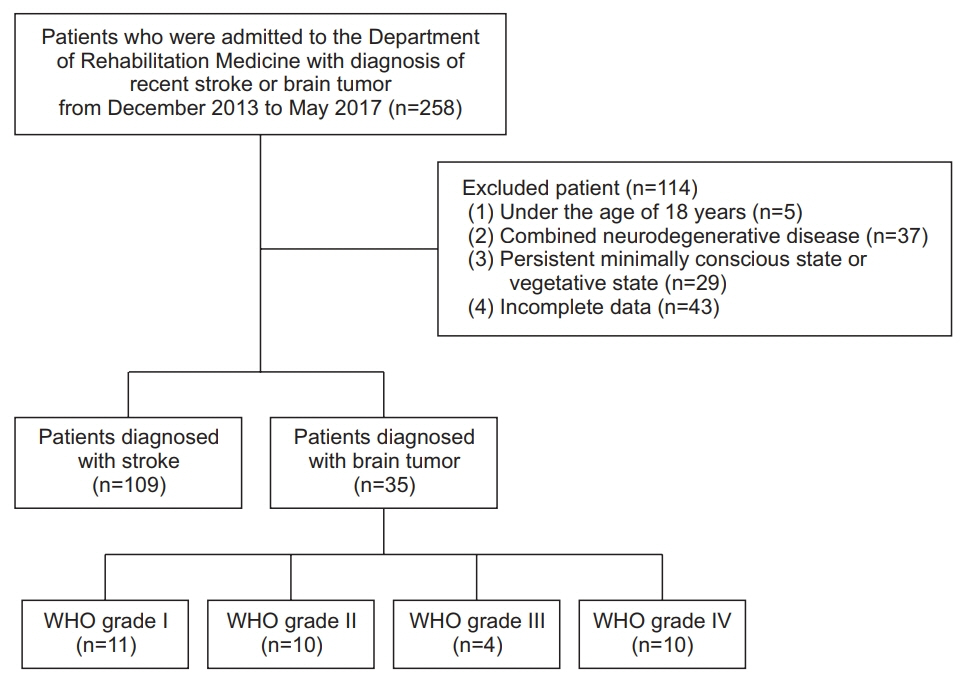
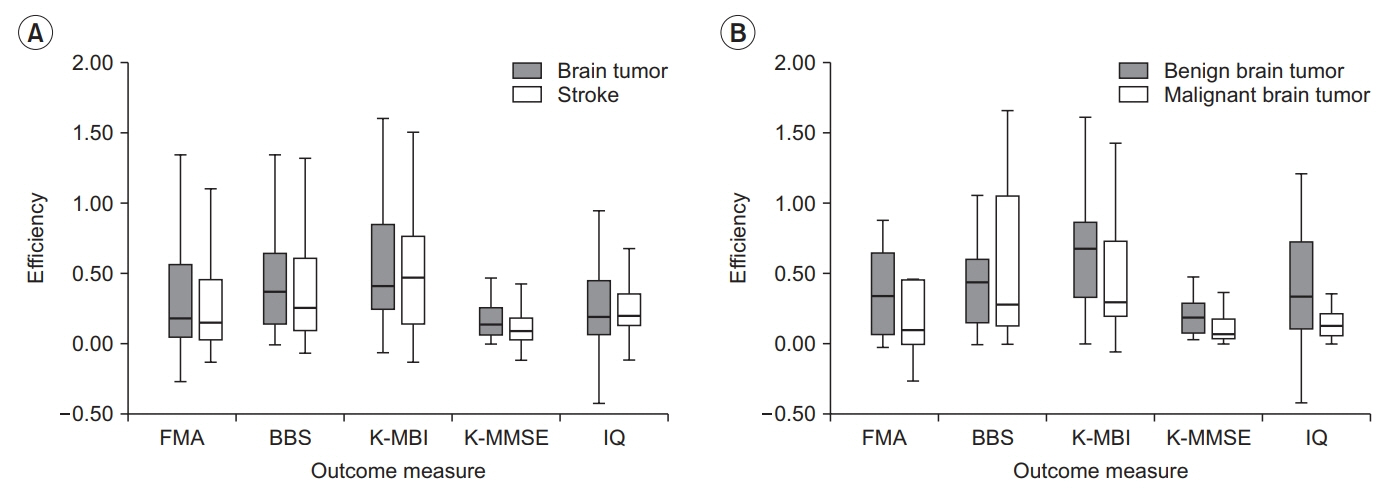
This retrospective study included patients with neurological impairment after brain tumor surgery who underwent intensive rehabilitation therapy between December 2013 and May 2017. To assess effectiveness of rehabilitation, functional outcomes (motor, cognition, and activities of daily living [ADL]) were compared between brain tumor group and a control group enrolling stroke patients who received equivalent rehabilitation during the study period. Long-term satisfaction with rehabilitation was evaluated by surveying family caregivers.
RESULTS
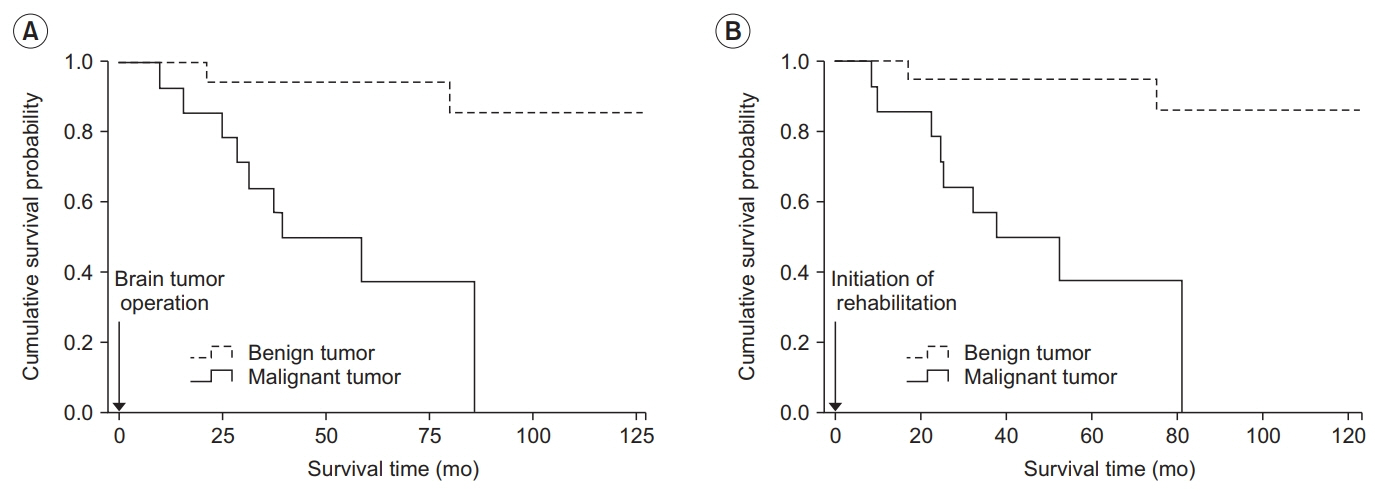
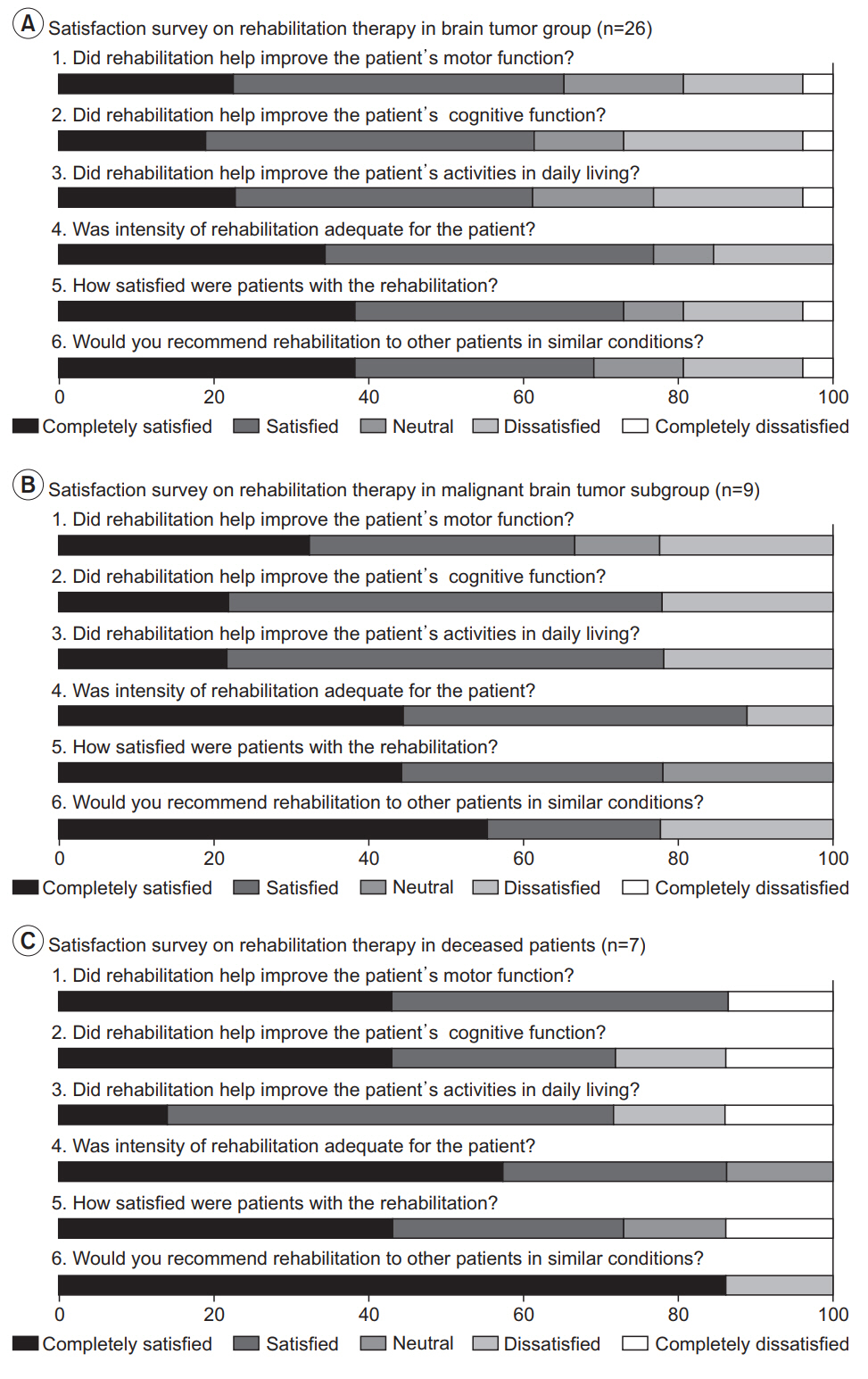
This study included 21 patients with benign brain tumor, 14 with malignant brain tumor, and 108 with stroke. Significant and similar improvement in motor, cognition, and ADL function were noted in both the brain tumor group and the stroke group. Malignancy status did not influence the extent of functional improvement. According to medical records and surveys, 9 (69.2%) patients with malignant tumor and 2 (11.8%) with benign tumor had expired by the time of the survey. Most family caregivers confirmed that rehabilitation was effective for functional improvement (>60%), expressing overall satisfaction and stating they would recommend such therapy to patients with similar conditions (approximately 70%).
CONCLUSION
Intensive rehabilitation may help promote functional improvement following brain tumor surgery regardless of malignancy compared with stroke patients. Family caregivers expressed overall satisfaction with rehabilitation at long-term follow-up. These findings support the provision of intensive rehabilitation therapy for neurologic function recovery following brain tumor surgery.
MeSH Terms
Figure
Reference
-
1. Prados MD, Berger MS, Wilson CB. Primary central nervous system tumors: advances in knowledge and treatment. CA Cancer J Clin. 1998; 48:331–60.
Article2. Geler-Kulcu D, Gulsen G, Buyukbaba E, Ozkan D. Functional recovery of patients with brain tumor or acute stroke after rehabilitation: a comparative study. J Clin Neurosci. 2009; 16:74–8.
Article3. DeLisa JA. A history of cancer rehabilitation. Cancer. 2001; 92(4 Suppl):970–4.
Article4. Jung KW, Yoo H, Kong HJ, Won YJ, Park S, Lee SH. Population-based survival data for brain tumors in Korea. J Neurooncol. 2012; 109:301–7.
Article5. Giordana MT, Clara E. Functional rehabilitation and brain tumour patients: a review of outcome. Neurol Sci. 2006; 27:240–4.
Article6. Giovagnoli AR, Tamburini M, Boiardi A. Quality of life in brain tumor patients. J Neurooncol. 1996; 30:71–80.
Article7. Olar A, Aldape KD. Using the molecular classification of glioblastoma to inform personalized treatment. J Pathol. 2014; 232:165–77.
Article8. Han EY, Chun MH, Kim BR, Kim HJ. Functional improvement after 4-week rehabilitation therapy and effects of attention deficit in brain tumor patients: comparison with subacute stroke patients. Ann Rehabil Med. 2015; 39:560–9.
Article9. Kirshblum S, O’Dell MW, Ho C, Barr K. Rehabilitation of persons with central nervous system tumors. Cancer. 2001; 92(4 Suppl):1029–38.
Article10. Lehmann JF, DeLisa JA, Warren CG, deLateur BJ, Bryant PL, Nicholson CG. Cancer rehabilitation: assessment of need, development, and evaluation of a model of care. Arch Phys Med Rehabil. 1978; 59:410–9.11. Huang ME, Cifu DX, Keyser-Marcus L. Functional outcome after brain tumor and acute stroke: a comparative analysis. Arch Phys Med Rehabil. 1998; 79:1386–90.
Article12. O’Dell MW, Barr K, Spanier D, Warnick RE. Functional outcome of inpatient rehabilitation in persons with brain tumors. Arch Phys Med Rehabil. 1998; 79:1530–4.13. Huang ME, Cifu DX, Keyser-Marcus L. Functional outcomes in patients with brain tumor after inpatient rehabilitation: comparison with traumatic brain injury. Am J Phys Med Rehabil. 2000; 79:327–35.14. Marciniak CM, Sliwa JA, Heinemann AW, Semik PE. Functional outcomes of persons with brain tumors after inpatient rehabilitation. Arch Phys Med Rehabil. 2001; 82:457–63.
Article15. Huang ME, Wartella JE, Kreutzer JS. Functional outcomes and quality of life in patients with brain tumors: a preliminary report. Arch Phys Med Rehabil. 2001; 82:1540–6.
Article16. Greenberg E, Treger I, Ring H. Rehabilitation outcomes in patients with brain tumors and acute stroke: comparative study of inpatient rehabilitation. Am J Phys Med Rehabil. 2006; 85:568–73.17. Harvey RF, Jellinek HM, Habeck RV. Cancer rehabilitation: an analysis of 36 program approaches. JAMA. 1982; 247:2127–31.
Article18. Haut MW, Haut JS, Bloomfield SS. Family issues in rehabilitation of patients with malignant brain tumors. Neurorehabilitation. 1991; 1:39–47.
Article19. Filley CM, Kleinschmidt-DeMasters BK. Neurobehavioral presentations of brain neoplasms. West J Med. 1995; 163:19–25.20. Kim HJ, Kim DY, Chun MH, Lee SJ. Functional outcomes and characteristics of patients with brain tumors after inpatient rehabilitation: comparison with ischemic stroke. J Korean Acad Rehabil Med. 2010; 34:290–6.21. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016; 131:803–20.
Article22. Sherer M, Meyers CA, Bergloff P. Efficacy of postacute brain injury rehabilitation for patients with primary malignant brain tumors. Cancer. 1997; 80:250–7.
Article23. Granger CV, Hamilton BB, Gresham GE, Kramer AA. The stroke rehabilitation outcome study. Part II. Relative merits of the total Barthel index score and a fouritem subscore in predicting patient outcomes. Arch Phys Med Rehabil. 1989; 70:100–3.24. Alexander MP. Stroke rehabilitation outcome: a potential use of predictive variables to establish levels of care. Stroke. 1994; 25:128–34.
Article25. Nijland RH, van Wegen EE, Harmeling-van der Wel BC, Kwakkel G; EPOS Investigators. Presence of finger extension and shoulder abduction within 72 hours after stroke predicts functional recovery: early prediction of functional outcome after stroke: the EPOS cohort study. Stroke. 2010; 41:745–50.26. Heruti RJ, Lusky A, Dankner R, Ring H, Dolgopiat M, Barell V, et al. Rehabilitation outcome of elderly patients after a first stroke: effect of cognitive status at admission on the functional outcome. Arch Phys Med Rehabil. 2002; 83:742–9.
Article27. Pound P, Gompertz P, Ebrahim S. Patients’ satisfaction with stroke services. Clin Rehabil. 1994; 8:7–17.
Article28. O’Mahony PG, Rodgers H, Thomson RG, Dobson R, James OF. Satisfaction with information and advice received by stroke patients. Clin Rehabil. 1997; 11:68–72.
Article29. Musicco M, Emberti L, Nappi G, Caltagirone C; Italian Multicenter Study on Outcomes of Rehabilitation of Neurological Patients. Early and long-term outcome of rehabilitation in stroke patients: the role of patient characteristics, time of initiation, and duration of interventions. Arch Phys Med Rehabil. 2003; 84:551–8.
Article30. Han B, Haley WE. Family caregiving for patients with stroke: review and analysis. Stroke. 1999; 30:1478–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Short-Term Effects of Intensive Inpatient Rehabilitation in Patients with Brain Tumor: a Single-Center Experience
- Development of Algorithm for Patient Specific Rehabilitation of Acute Stroke Patient
- Erratum: Correction of the Funding Statement: Feasibility and Therapeutic Effects of a Novel Magnet-Based Device for Hand Rehabilitation: a Pilot Study
- Rehabilitation in Intensive Care Unit
- Can the Effectiveness of the Psychoanalytic Therapies Truly Be Proven?: The Effectiveness of the Psychoanalysis and Psychoanalytic Psychotherapy