Ann Rehabil Med.
2018 Dec;42(6):846-853. 10.5535/arm.2018.42.6.846.
Effects of Ultrasound, Laser and Exercises on Temporomandibular Joint Pain and Trismus Following Head and Neck Cancer
- Affiliations
-
- 1Department of Physical Therapy for Surgery, Faculty of Physical Therapy, Cairo University, Giza, Egypt. gohary75pt@hotmail.com
- 2Faculty of Physical Therapy, Badr University in Cairo, Cairo, Egypt.
- 3Department of Physical Therapy for Musculoskeletal Disorders and Its Surgery, Faculty of Physical Therapy, Cairo University, Giza, Egypt.
- KMID: 2448906
- DOI: http://doi.org/10.5535/arm.2018.42.6.846
Abstract
OBJECTIVE
To compare the effects of low intensity ultrasound (LIUS), traditional exercise therapy (TET), low level laser therapy (LLLT) and TET on temporomandibular joint (TMJ) pain and trismus following recovery from head and neck cancer (HNC).
METHODS
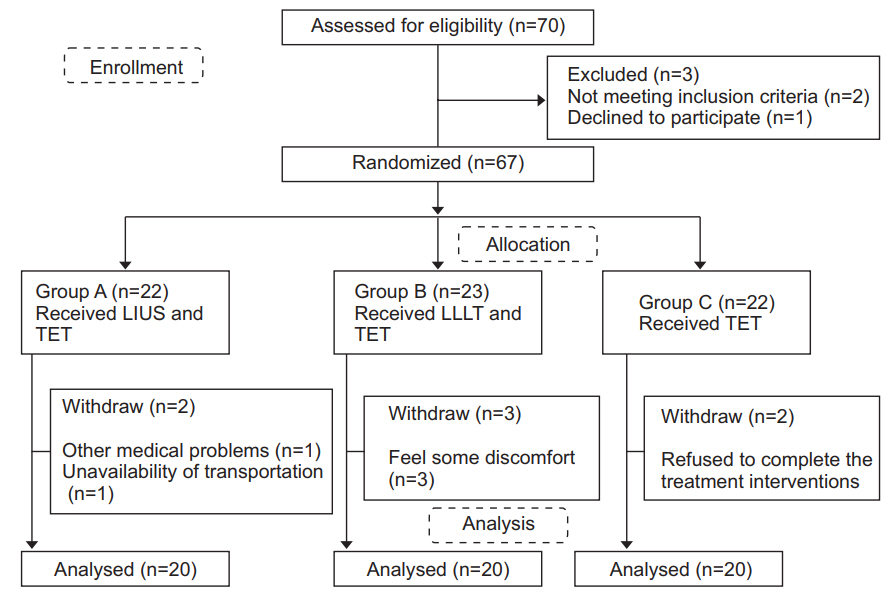
Sixty participants following, who had experienced HNC, were randomly allocated to three groups of 20 people each. Each group received different therapy. Group A received LIUS and TET; group B received LLLT and TET; while group C received TET. All 60 participants were evaluated under the visual analog scale (VAS), the University of Washington Quality of Life questionnaire (UW-QOL) and the Vernier caliper scale (VCS) at the beginning of the therapies and after 4 weeks.
RESULTS
ANOVA test revealed significant improvements across all three groups with outcomes of p < 0.05. The results of the UW-QOL questionnaire showed a significant difference between groups A, B and C in favor of group A (p < 0.05). The VAS results showed a more improvement in group A as compared to group B (p < 0.05), while there was no statistical difference between groups B and C (p>0.05). The VCS results showed more improvement for the individuals in group B as compared to those in group C (p < 0.05), while there was minimal difference between groups A and B (p>0.05).
CONCLUSION
The LIUS and TET are more effective than LLLT and/or TET in reducing TMJ pain and trismus following HNC.
MeSH Terms
Figure
Reference
-
1. Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011; 61:69–90.
Article2. Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007; 57:43–66.
Article3. Boyle P, Levin B. World cancer report 2008. Lyon: International Agency for Research on Cancer Publication;2008.4. Al-Belasy FA. Ultrasound-guided drainage of submasseteric space abscesses. J Oral Maxillofac Surg. 2005; 63:36–41.
Article5. Brooke RI. Facial trismus and myofascial pain associated with infections and malignant disease. Oral Surg Oral Med Oral Pathol. 1988; 66:450.6. Gomez DR, Zhung JE, Gomez J, Chan K, Wu AJ, Wolden SL, et al. Intensity-modulated radiotherapy in postoperative treatment of oral cavity cancers. Int J Radiat Oncol Biol Phys. 2009; 73:1096–103.
Article7. Goldstein M, Maxymiw WG, Cummings BJ, Wood RE. The effects of antitumor irradiation on mandibular opening and mobility: a prospective study of 58 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 88:365–73.
Article8. Wang CJ, Huang EY, Hsu HC, Chen HC, Fang FM, Hsiung CY. The degree and time-course assessment of radiation-induced trismus occurring after radiotherapy for nasopharyngeal cancer. Laryngoscope. 2005; 115:1458–60.
Article9. Ichimura K, Tanaka T. Trismus in patients with malignant tumours in the head and neck. J Laryngol Otol. 1993; 107:1017–20.
Article10. Chua DT, Lo C, Yuen J, Foo YC. A pilot study of pentoxifylline in the treatment of radiation-induced trismus. Am J Clin Oncol. 2001; 24:366–9.
Article11. Buchbinder D, Currivan RB, Kaplan AJ, Urken ML. Mobilization regimens for the prevention of jaw hypomobility in the radiated patient: a comparison of three techniques. J Oral Maxillofac Surg. 1993; 51:863–7.
Article12. Gray RJ, Quayle AA, Hall CA, Schofield MA. Physiotherapy in the treatment of temporomandibular joint disorders: a comparative study of four treatment methods. Br Dent J. 1994; 176:257–61.
Article13. Leung MS, Cheing GL. Effects of deep and superficial heating in the management of frozen shoulder. J Rehabil Med. 2008; 40:145–50.
Article14. Shiraishi R, Masaki C, Toshinaga A, Okinaga T, Nishihara T, Yamanaka N, et al. The effects of low-intensity pulsed ultrasound exposure on gingival cells. J Periodontol. 2011; 82:1498–503.
Article15. Hashish I, Harvey W, Harris M. Anti-inflammatory effects of ultrasound therapy: evidence for a major placebo effect. Br J Rheumatol. 1986; 25:77–81.
Article16. McNeely ML, Armijo Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther. 2006; 86:710–25.
Article17. Nicolakis P, Erdogmus B, Kopf A, Ebenbichler G, Kollmitzer J, Piehslinger E, et al. Effectiveness of exercise therapy in patients with internal derangement of the temporomandibular joint. J Oral Rehabil. 2001; 28:1158–64.
Article18. Ferrante M, Petrini M, Trentini P, Perfetti G, Spoto G. Effect of low-level laser therapy after extraction of impacted lower third molars. Lasers Med Sci. 2013; 28:845–9.
Article19. Alan H, Yolcu U, Koparal M, Ozgur C, Ozturk SA, Malkoc S. Evaluation of the effects of the low-level laser therapy on swelling, pain, and trismus after removal of impacted lower third molar. Head Face Med. 2016; 12:25.
Article20. Wu VW, Lam YN. Radiation-induced temporo-mandibular joint disorder in post-radiotherapy nasopharyngeal carcinoma patients: assessment and treatment. J Med Radiat Sci. 2016; 63:124–32.
Article21. Agrawal J, Shenai PK, Chatra L, Kumar PY. Evaluation of normal range of mouth opening using three finger index: South India perspective study. Indian J Dent Res. 2015; 26:361–5.
Article22. Ringash J, Bezjak A. A structured review of quality of life instruments for head and neck cancer patients. Head Neck. 2001; 23:201–13.
Article23. Kanatas AN, Rogers SN. A national survey of healthrelated quality of life questionnaires in head and neck oncology. Ann R Coll Surg Engl. 2004; 86:6–10.
Article24. Rogers SN, Lowe D. Screening for dysfunction to promote multidisciplinary intervention by using the University of Washington Quality of Life Questionnaire. Arch Otolaryngol Head Neck Surg. 2009; 135:369–75.
Article25. The British Pain Society. Pain scales in multiple languages [Internet]. London: The British Pain Society;c2014; [cited 2018 Nov 15]. Available from: https://www.britishpainsociety.org/british-pain-societypublications/pain-scales-in-multiple-languages/.26. Dijkstra PU, Sterken MW, Pater R, Spijkervet FK, Roodenburg JL. Exercise therapy for trismus in head and neck cancer. Oral Oncol. 2007; 43:389–94.
Article27. Israel HA, Syrop SB. The important role of motion in the rehabilitation of patients with mandibular hypomobility: a review of the literature. Cranio. 1997; 15:74–83.
Article28. Lee LY, Chen SC, Chen WC, Huang BS, Lin CY. Postradiation trismus and its impact on quality of life in patients with head and neck cancer. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015; 119:187–95.
Article29. Pauli N, Johnson J, Finizia C, Andrell P. The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol. 2013; 52:1137–45.
Article30. Carrillo JS, Calatayud J, Manso FJ, Barberia E, Martinez JM, Donado M. A randomized double-blind clinical trial on the effectiveness of helium-neon laser in the prevention of pain, swelling and trismus after removal of impacted third molars. Int Dent J. 1990; 40:31–6.31. Zecha JA, Raber-Durlacher JE, Nair RG, Epstein JB, Elad S, Hamblin MR, et al. Low-level laser therapy/photobiomodulation in the management of side effects of chemoradiation therapy in head and neck cancer: part 2: proposed applications and treatment protocols. Support Care Cancer. 2016; 24:2793–805.
Article32. Roynesdal AK, Bjornland T, Barkvoll P, Haanaes HR. The effect of soft-laser application on postoperative pain and swelling: a double-blind, crossover study. Int J Oral Maxillofac Surg. 1993; 22:242–5.33. Fernando S, Hill CM, Walker R. A randomised double blind comparative study of low level laser therapy following surgical extraction of lower third molar teeth. Br J Oral Maxillofac Surg. 1993; 31:170–2.
Article34. Esposito CJ, Veal SJ, Farman AG. Alleviation of myofascial pain with ultrasonic therapy. J Prosthet Dent. 1984; 51:106–8.
Article35. Rai S, Kaur M, Goel S, Panjwani S, Singh S. Prospective utility of therapeutic ultrasound in dentistry: review with recent comprehensive update. Adv Biomed Res. 2012; 1:47.36. Grieder A, Vinton PW, Cinotti WR, Kangur TT. An evaluation of ultrasonic therapy for temporomandibular joint dysfunction. Oral Surg Oral Med Oral Pathol. 1971; 31:25–31.
Article37. Oh DW, Kim KS, Lee GW. The effect of physiotherapy on post-temporomandibular joint surgery patients. J Oral Rehabil. 2002; 29:441–6.
Article38. Tuncer AB, Ergun N, Tuncer AH, Karahan S. Effectiveness of manual therapy and home physical therapy in patients with temporomandibular disorders: a randomized controlled trial. J Bodyw Mov Ther. 2013; 17:302–8.
Article39. Calixtre LB, Moreira RF, Franchini GH, Alburquerque-Sendin F, Oliveira AB. Manual therapy for the management of pain and limited range of motion in subjects with signs and symptoms of temporomandibular disorder: a systematic review of randomised controlled trials. J Oral Rehabil. 2015; 42:847–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myositis Associated with Infratemporal Space Abscess in Patient with Myxofibrosarcoma of Nasal Cavity: Case Report
- Airway Management for General Anesthesia in a Patient with Severe Trismus due to Temporomandibular Joint Ankylosis : A case report
- Mouth opening limitation caused by coronoid hyperplasia: a report of four cases
- Use of Intermaxillary Traction Appliances and Exercises to Strengthen the Masticatory Muscles of Patients with Anterior Open Bite Caused by Temporomandibular Joint Osteoarthritis: Case Reports
- Absorbed doses in organs of the head and neck from conventional temporomandibular joint tomography