Ann Hepatobiliary Pancreat Surg.
2019 May;23(2):192-196. 10.14701/ahbps.2019.23.2.192.
Development of adenocarcinoma at the remnant intrapancreatic cyst 16 years after resection of the choledochal cyst
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2448776
- DOI: http://doi.org/10.14701/ahbps.2019.23.2.192
Abstract
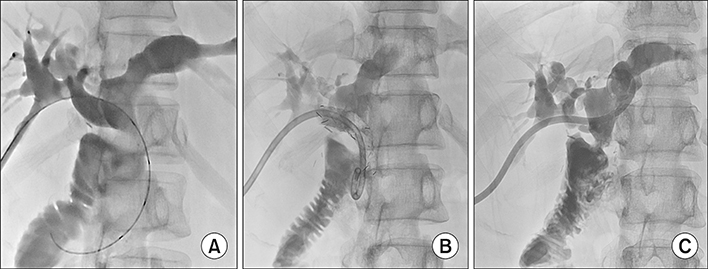
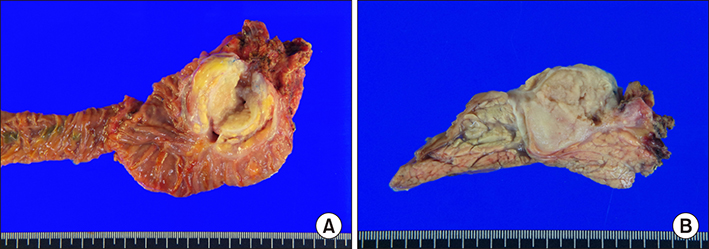
- One of the main reasons to resect choledochal cyst (CC) is to prevent malignant transformation. After resection of CC, the remnant intrapancreatic bile duct is no longer exposed to the enzymatic insult from pancreatic juice activated by the bile. Thus theoretically, the risk of malignant transformation disappears. We present a case showing development of adenocarcinoma from the remnant CC 16 years after resection of CC. A 43 year-old female patient underwent resection of type I CC 16 years ago, leaving a small remnant portion of CC as it was located deep within the pancreas close to the anomalous union of the pancreatobiliary duct. Four years later, intrahepatic ducts were dilated due to anastomotic stricture of the hepaticojejunostomy, which was resolved after repeated balloon dilatation. On follow-up examination at postoperative 16 years, a mass within the pancreas head was identified. As the mass was identified as adenocarcinoma on biopsy, pylorus-preserving pancreatoduodenectomy was performed. Pathologic examination showed a 3.5 cm-sized moderately differentiated adenocarcinoma arising from the remnant CC, with no lymph node metastasis. The patient recovered uneventfully, and is currently undergoing adjuvant chemotherapy. This case indicates that remnant CC can undergo malignant transformation. Therefore, complete resection of CC coupled with life-long follow-up is emphasized.
MeSH Terms
Figure
Cited by 2 articles
-
Development of intrahepatic cholangiocarcinoma at the remnant intrahepatic cyst portion 10 years after resection of type IV choledochal cyst
Suhyeon Ha, Shin Hwang, Lee Na Ryu
Ann Hepatobiliary Pancreat Surg. 2020;24(3):366-372. doi: 10.14701/ahbps.2020.24.3.366.Management of intractable pancreatic leak from iatrogenic pancreatic duct injury following resection of choledochal cyst in an adult patient
Jin Uk Choi, Shin Hwang, Yong-Kyu Chung
Ann Hepatobiliary Pancreat Surg. 2020;24(2):228-233. doi: 10.14701/ahbps.2020.24.2.228.
Reference
-
1. Fan F, Xu DP, Xiong ZX, Li HJ, Xin HB, Zhao H, et al. Clinical significance of intrapancreatic choledochal cyst excision in surgical management of type I choledochal cyst. J Int Med Res. 2018; 46:1221–1229.
Article2. Cho MJ, Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, et al. Surgical experience of 204 cases of adult choledochal cyst disease over 14 years. World J Surg. 2011; 35:1094–1102.
Article3. Ando H, Kaneko K, Ito T, Watanabe Y, Seo T, Harada T, et al. Complete excision of the intrapancreatic portion of choledochal cysts. J Am Coll Surg. 1996; 183:317–321.4. Shimizu T, Suzuki R, Yamashiro Y, Segawa O, Yamataka A, Kuwatsuru R. Magnetic resonance cholangiopancreatography in assessing the cause of acute pancreatitis in children. Pancreas. 2001; 22:196–199.
Article5. Yoon JH. Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. Br J Radiol. 2011; 84:e18–e22.
Article6. Ng DW, Chiow AK, Poh WT, Tan SS. Metachronous cholangiocarcinoma 13 years post resection of choledochal cyst-is long-term follow-up useful?: a case study and review of the literature. Surg Case Rep. 2016; 2:60.
Article7. Shimamura K, Kurosaki I, Sato D, Takano K, Yokoyama N, Sato Y, et al. Intrahepatic cholangiocarcinoma arising 34 years after excision of a type IV-A congenital choledochal cyst: report of a case. Surg Today. 2009; 39:247–251.
Article8. Kumamoto T, Tanaka K, Takeda K, Nojiri K, Mori R, Taniguchi K, et al. Intrahepatic cholangiocarcinoma arising 28 years after excision of a type IV-A congenital choledochal cyst: report of a case. Surg Today. 2014; 44:354–358.9. Goto N, Yasuda I, Uematsu T, Kanemura N, Takao S, Ando K, et al. Intrahepatic cholangiocarcinoma arising 10 years after the excision of congenital extrahepatic biliary dilation. J Gastroenterol. 2001; 36:856–862.
Article10. Nishiyama R, Shinoda M, Tanabe M, Masugi Y, Ueno A, Hibi T, et al. Intrahepatic cholangiocarcinoma arising 33 years after excision of a choledochal cyst: report of a case. Int Surg. 2011; 96:320–325.11. Ohashi T, Wakai T, Kubota M, Matsuda Y, Arai Y, Ohyama T, et al. Risk of subsequent biliary malignancy in patients undergoing cyst excision for congenital choledochal cysts. J Gastroenterol Hepatol. 2013; 28:243–247.
Article12. Thistlethwaite JR, Horwitz A. Choledochal cyst followed by carcinoma of the hepatic duct. South Med J. 1967; 60:872–874.
Article13. Gallagher PJ, Millis RR, Mitchinson MJ. Congenital dilatation of the intrahepatic bile ducts with cholangiocarcinoma. J Clin Pathol. 1972; 25:804–808.
Article14. Chaudhuri PK, Chaudhuri B, Schuler JJ, Nyhus LM. Carcinoma associated with congenital cystic dilation of bile ducts. Arch Surg. 1982; 117:1349–1351.
Article15. Yoshikawa K, Yoshida K, Shirai Y, Sato N, Kashima Y, Coutinho DS, et al. A case of carcinoma arising in the intrapancreatic terminal choledochus 12 years after primary excision of a giant choledochal cyst. Am J Gastroenterol. 1986; 81:378–384.16. Rossi RL, Silverman ML, Braasch JW, Munson JL, ReMine SG. Carcinomas arising in cystic conditions of the bile ducts. A clinical and pathologic study. Ann Surg. 1987; 205:377–384.17. Young WT, Thomas GV, Blethyn AJ, Lawrie BW. Choledochal cyst and congenital anomalies of the pancreatico-biliary junction: the clinical findings, radiology and outcome in nine cases. Br J Radiol. 1992; 65:33–38.
Article18. Kobayashi S, Asano T, Yamasaki M, Kenmochi T, Nakagohri T, Ochiai T. Risk of bile duct carcinogenesis after excision of extrahepatic bile ducts in pancreaticobiliary maljunction. Surgery. 1999; 126:939–944.
Article19. Koike M, Yasui K, Shimizu Y, Kodera Y, Hirai T, Morimoto T, et al. Carcinoma of the hepatic hilus developing 21 years after biliary diversion for choledochal cyst: a case report. Hepatogastroenterology. 2002; 49:1216–1220.20. Suzuki S, Amano K, Harada N, Tanaka S, Hayashi T, Suzuki M, et al. A case of intrahepatic cholangiocarcinoma arising 26 years after excision of congenital biliary dilatation. Jpn J Gastroenterol Surg. 2004; 37:416–421.
Article21. Ono S, Sakai K, Kimura O, Iwai N. Development of bile duct cancer in a 26-year-old man after resection of infantile choledochal cyst. J Pediatr Surg. 2008; 43:E17–E19.
Article22. Han JH, Lee JH, Hwang DW, Song KB, Shin SH, Kwon JW, et al. Robot resection of a choledochal cyst with Roux-en-y hepaticojejunostomy in adults: initial experiences with 22 cases and a comparison with laparoscopic approaches. Ann Hepatobiliary Pancreat Surg. 2018; 22:359–366.
Article23. Margonis GA, Spolverato G, Kim Y, Marques H, Poultsides G, Maithel S, et al. Minimally invasive resection of choledochal cyst: a feasible and safe surgical option. J Gastrointest Surg. 2015; 19:858–865.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of Cholangiocarcinoma Arising from Remnant Intrapancreatic Cyst 15 Years after Choledochal Cyst Excision
- Multiple stone formation in a remnant choledochal cyst
- Two Cases of Plug or Stone in Remnant Intrapancreatic Choledochal Cysts Treated with Endoscopic Retrograde Cholangiopancreatography
- Malignant Degeneration and Hepatic Metastasis Related to Choledochal Cyst with Internal Drainage Procedure: a Case Report
- A case of type IVa choledochal cyst