Pediatric living donor liver transplantation with homograft replacement of retrohepatic inferior vena cava for advanced hepatoblastoma
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2448773
- DOI: http://doi.org/10.14701/ahbps.2019.23.2.178
Abstract
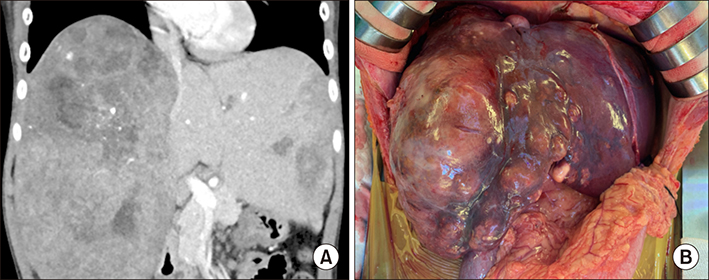
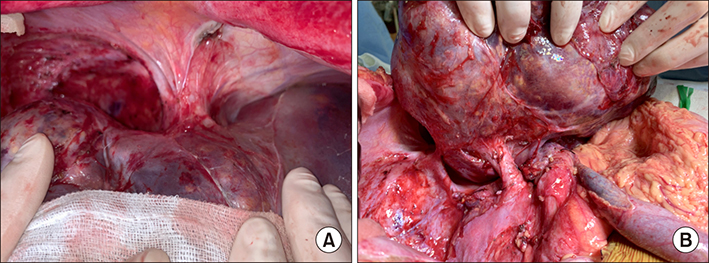
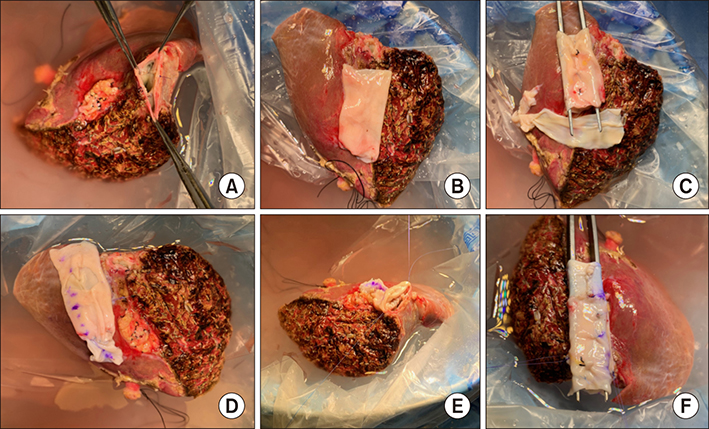
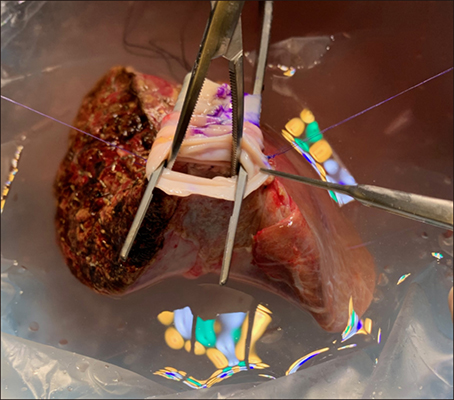
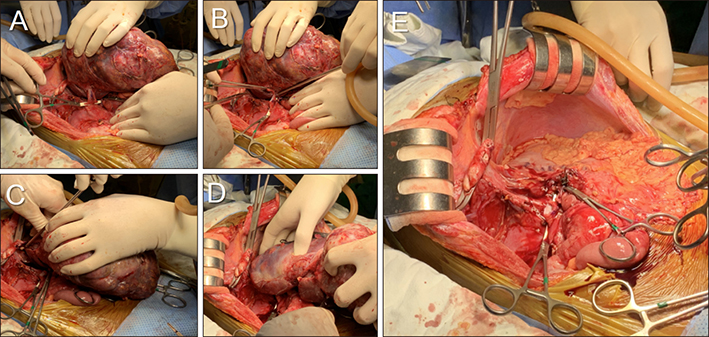
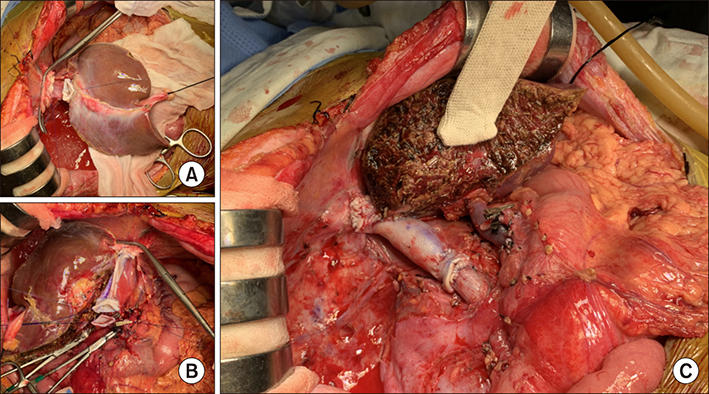
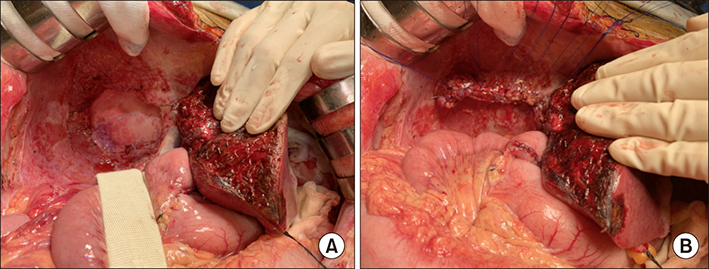
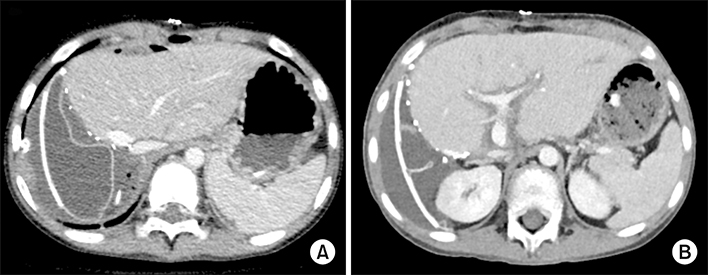
- Replacement of the retrohepatic inferior vena cava (IVC) after concurrent resection of IVC and hepatocellular carcinoma-containing liver is settled as a feasible living donor liver transplantation (LDLT) technique to cope with tumors around the IVC. This technique makes LDLT comparable to deceased-donor liver transplantation (DDLT). In the current Korean setting, the common substitute for IVC is a Dacron graft for adult recipients. In contrast, such a synthetic graft cannot be used for pediatric patients because of ongoing growth. We present one pediatric LDLT case with IVC homograft replacement for advanced hepatoblastoma. The patient was a 8 year-old boy suffering from large multiple hepatoblastomas. The tumors encroached the retrohepatic IVC. Thus there was high risk of residual tumor cells at the IVC, if it was preserved. Thus, we decided to replace IVC at the time of LDLT. After waiting for >1 month, we finally obtained cold-stored IVC homograft and LDLT was performed with the mother's left liver. A 4 cm-long IVC allograft was anastomosed at the back table. The left liver graft with IVC interposition was implanted along standard procedure similar to DDLT. The patient recovered uneventfully and is undergoing scheduled adjuvant chemotherapy. We have performed >20 cases of IVC replacement in adult recipients with hepatocellular carcinoma or Budd-Chiari syndrome, but all vessel substitutes were synthetic, because sizable IVC homograft is unavailable. In pediatric recipients, various vein homografts such as iliac vein, IVC and other large-sized veins, can be used depending on body size of recipient and availability of vessel grafts.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Changes in the indications for living donor liver transplantation: single-institution experience of 3,145 cases over 10 years
Sang-Hyun Kang, Shin Hwang, Chul-Soo Ahn, Ki-Hun Kim, Deok-Bog Moon, Tae-Yong Ha, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Jung-Man Namgoong, Young-In Yoon, Hui-Dong Cho, Jae-Hyun Kwon, Yong-Kyu Chung, Jin-Uk Choi, Sung-Gyu Lee
Korean J Transplant. 2020;34(1):47-54. doi: 10.4285/kjt.2020.34.1.47.Living-donor liver transplantation with inferior vena cava replacement in an infant recipient with advanced hepatoblastoma
Jung-Man Namgoong, Shin Hwang, Seak Hee Oh, Kyung Mo Kim, Gil-Chun Park, Chul-Soo Ahn, Hyunhee Kwon, Yu Jeong Cho, Yong Jae Kwon
Ann Hepatobiliary Pancreat Surg. 2020;24(1):72-77. doi: 10.14701/ahbps.2020.24.1.72.Patch venoplasty for resecting tumor invading the retrohepatic inferior vena cava using total and selective hepatic vascular exclusion
Sung-Min Kim, Shin Hwang, Deok-Bog Moon, Dong-Hwan Jung, Sung-Gyu Lee
Ann Hepatobiliary Pancreat Surg. 2021;25(4):536-543. doi: 10.14701/ahbps.2021.25.4.536.
Reference
-
1. Chen CL, Concejero AM, Wang CC, Wang SH, Liu YW, Yang CH, et al. Inferior vena cava replacement in living donor liver transplantation for hepatocellular carcinoma. Liver Transpl. 2009; 15:1637–1640.
Article2. Matsuda H, Sadamori H, Shinoura S, Umeda Y, Yoshida R, Satoh D, et al. Aggressive combined resection of hepatic inferior vena cava, with replacement by a ringed expanded polytetrafluoroethylene graft, in living-donor liver transplantation for hepatocellular carcinoma beyond the Milan criteria. J Hepatobiliary Pancreat Sci. 2010; 17:719–724.
Article3. Moon DB, Lee SG, Hwang S, Kim KH, Ahn CS, Ha TY, et al. No-touch en bloc right lobe living-donor liver transplantation with inferior vena cava replacement for hepatocellular carcinoma close to retrohepatic inferior vena cava: case report. Transplant Proc. 2013; 45:3135–3139.
Article4. Zahr Eldeen F, Abdulfatah MR, Broering D. Inferior vena cava replacement in living-donor liver transplant for hepatocellular carcinoma: first case report in Saudi Arabia. Exp Clin Transplant. 2018; 16:625–627.5. Sasaki K, Kasahara M, Fukuda A, Shigeta T, Tanaka H, Nakagawa S, et al. Living donor liver transplantation with vena cava reconstruction using a cryopreserved allograft for a pediatric patient with Budd-Chiari syndrome. Transplantation. 2009; 87:304–305.
Article6. Yoon YI, Lee SG, Moon DB, Ahn CS, Hwang S, Kim KH, et al. Surgical techniques and long-term outcomes of living-donor liver transplantation with inferior vena cava replacement using atriocaval synthetic interposition graft for Budd-Chiari syndrome. Ann Surg. 2019; 269:e43–e45.
Article7. Yamamichi T, Oue T, Yonekura T, Owari M, Nakahata K, Umeda S, et al. Clinical application of indocyanine green (ICG) fluorescent imaging of hepatoblastoma. J Pediatr Surg. 2015; 50:833–836.
Article8. Inomata Y, Tanaka K, Egawa H, Uemoto S, Kiuchi T, Satomura K, et al. Application of a tissue expander for stabilizing graft position in living-related liver transplantation. Clin Transplant. 1997; 11:56–59.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Retrohepatic inferior vena cava interposition in living donor liver transplantation for a pediatric patient with advanced hepatoblastoma
- Living-donor liver transplantation with inferior vena cava replacement in an infant recipient with advanced hepatoblastoma
- Inferior vena cava stenosis-induced sinusoidal obstructive syndrome after living donor liver transplantation
- Technical refinement of inferior vena cava replacement using a synthetic vascular graft in living donor liver transplantation
- A Case of Living Donor Liver Transplantation for Unresectable Hepatoblastoma