Anesth Pain Med.
2019 Apr;14(2):222-229. 10.17085/apm.2019.14.2.222.
Thoracic interfascial plane block for multimodal analgesia after breast lumpectomy
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chungnam National University Hospital, Daejeon, Korea. koho0127@gmail.com
- KMID: 2447974
- DOI: http://doi.org/10.17085/apm.2019.14.2.222
Abstract
- BACKGROUND
Thoracic interfascial plane block is useful as a component of multimodal analgesia in patients undergoing mastectomy. However, multimodal analgesia tends not to be provided during lumpectomy as it is one of the less aggressive procedures among breast cancer surgeries. Therefore, we investigated the effects of thoracic interfascial plane block as more effective analgesia after breast lumpectomy.
METHODS
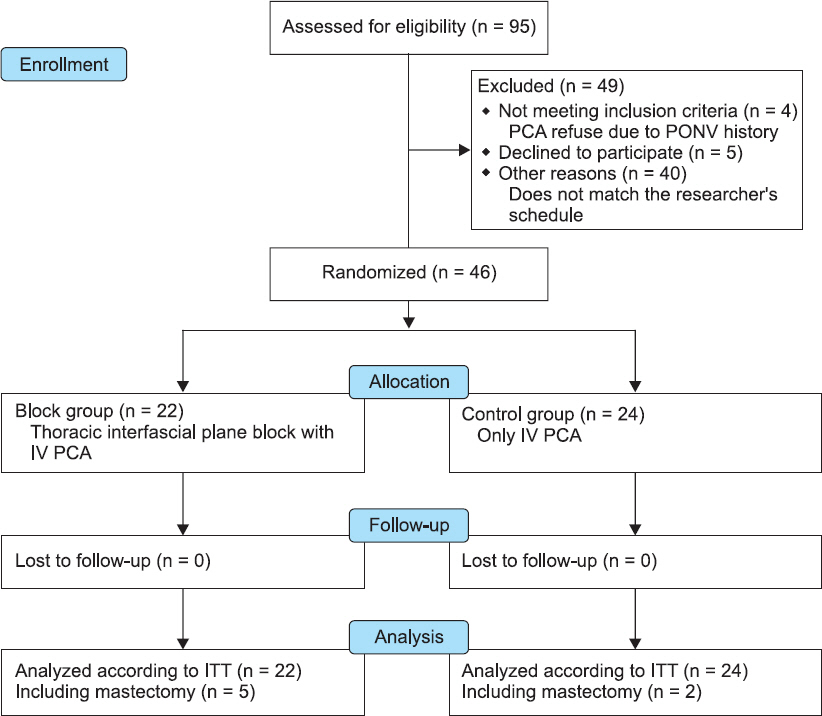
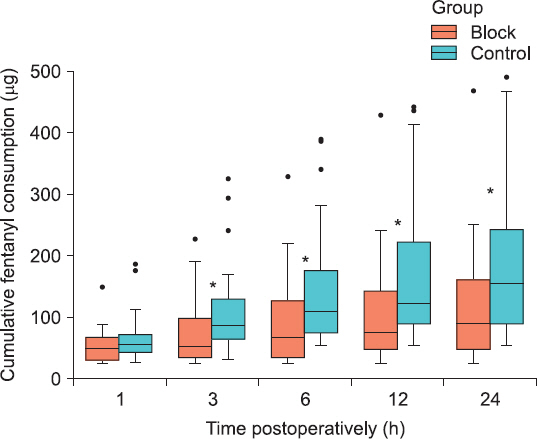
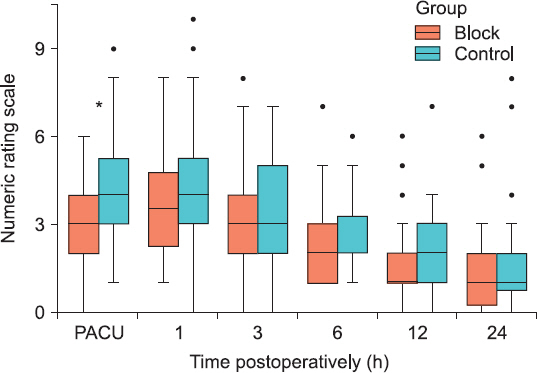
Forty six patients (20-80 years old, female) with breast cancer scheduled to undergo lumpectomy were randomly assigned to two groups. Postoperative pain control in the control group consisted only of intravenous patient-controlled analgesia (PCA). In the block group, intravenous PCA was used after serratus intercostal fascial plane block and pecto-intercostal fascial plane block. The primary outcome was the 24 h cumulative postoperative fentanyl consumption. Pain severity, additional rescue analgesic requirement, side effects, and patient satisfaction were also evaluated.
RESULTS
Postoperative fentanyl consumption in the block group was significantly reduced compared with the control group (median, 88.8 [interquartile range, 48.0, 167.6] vs. 155.2 [88.8, 249.2], P = 0.022). The pain score was significantly lower in the block group only in the post-anesthesia care unit (2.9 ± 1.8 vs. 4.3 ± 2.3, P = 0.022). There were no differences in the incidence of postoperative nausea and vomiting and the requirement for additional analgesics between the groups. The satisfaction score was significantly higher in the block group.
CONCLUSIONS
Thoracic interfascial plane block after lumpectomy reduces opioid usage and increases patient satisfaction with postoperative pain control. Thoracic interfascial plane block is useful for multimodal analgesia after lumpectomy.
MeSH Terms
Figure
Reference
-
1. Andersen KG, Kehlet H. Persistent pain after breast cancer treatment: a critical review of risk factors and strategies for prevention. J Pain. 2011; 12:725–46. DOI: 10.1016/j.jpain.2010.12.005. PMID: 21435953.2. Fassoulaki A, Melemeni A, Staikou C, Triga A, Sarantopoulos C. Acute postoperative pain predicts chronic pain and long-term analgesic requirements after breast surgery for cancer. Acta Anaesthesiol Belg. 2008; 59:241–8. PMID: 19235522.3. Iohom G, Abdalla H, O'Brien J, Szarvas S, Larney V, Buckley E, et al. The associations between severity of early postoperative pain, chronic postsurgical pain and plasma concentration of stable nitric oxide products after breast surgery. Anesth Analg. 2006; 103:995–1000. DOI: 10.1213/01.ANE.0000240415.49180.4A. PMID: 17000819.4. Katz J, Jackson M, Kavanagh BP, Sandler AN. Acute pain after thoracic surgery predicts long-term post-thoracotomy pain. Clin J Pain. 1996; 12:50–5. DOI: 10.1097/00002508-199603000-00009. PMID: 8722735.5. Woodworth GE, Ivie RMJ, Nelson SM, Walker CM, Maniker RB. Perioperative breast analgesia: a qualitative review of anatomy and regional techniques. Reg Anesth Pain Med. 2017; 42:609–31. DOI: 10.1097/AAP.0000000000000641. PMID: 28820803.6. Apfel CC, Läärä E, Koivuranta M, Greim CA, Roewer N. A simplified risk score for predicting postoperative nausea and vomiting: conclusions from cross-validations between two centers. Anesthesiology. 1999; 91:693–700. DOI: 10.1097/00000542-199909000-00022.7. Lynch EP, Welch KJ, Carabuena JM, Eberlein TJ. Thoracic epidural anesthesia improves outcome after breast surgery. Ann Surg. 1995; 222:663–9. DOI: 10.1097/00000658-199511000-00009. PMID: 7487214. PMCID: PMC1234994.8. Naja MZ, Ziade MF, Lönnqvist PA. Nerve-stimulator guided paravertebral blockade vs. general anaesthesia for breast surgery: a prospective randomized trial. Eur J Anaesthesiol. 2003; 20:897–903. DOI: 10.1097/00003643-200311000-00007.9. Klein SM, Bergh A, Steele SM, Georgiade GS, Greengrass RA. Thoracic paravertebral block for breast surgery. Anesth Analg. 2000; 90:1402–5. DOI: 10.1097/00000539-200006000-00026. PMID: 10825328.10. Moller JF, Nikolajsen L, Rodt SA, Ronning H, Carlsson PS. Thoracic paravertebral block for breast cancer surgery: a randomized double-blind study. Anesth Analg. 2007; 105:1848–51. DOI: 10.1213/01.ane.0000286135.21333.fd. PMID: 18042892.11. Blanco R, Fajardo M, Parras Maldonado T. Ultrasound description of Pecs II (modified Pecs I): a novel approach to breast surgery. Rev Esp Anestesiol Reanim. 2012; 59:470–5. DOI: 10.1016/j.redar.2012.07.003. PMID: 22939099.12. Blanco R. The 'pecs block': a novel technique for providing analgesia after breast surgery. Anaesthesia. 2011; 66:847–8. DOI: 10.1111/j.1365-2044.2011.06838.x. PMID: 21831090.13. de la Torre PA, García PD, Alvarez SL, Miguel FJ, Pérez MF. A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthet Surg J. 2014; 34:198–200. DOI: 10.1177/1090820X13515902. PMID: 24396082.14. Fajardo-Pérez M, Altınpulluk EY, García-Miguel J, Quintana-Gordon B. Ultrasound-guided continuous interpectoral block for patient undergoing mastectomy and axillary clearance. Turk J Anaesthesiol Reanim. 2017; 45:112–5. DOI: 10.5152/TJAR.2017.43815. PMID: 28439445. PMCID: PMC5396896.15. Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: a randomized clinical trial. Reg Anesth Pain Med. 2015; 40:68–74. DOI: 10.1097/AAP.0000000000000163. PMID: 25376971.16. M N, Pandey RK, Sharma A, Darlong V, Punj J, Sinha R, et al. Pectoral nerve blocks to improve analgesia after breast cancer surgery: a prospective, randomized and controlled trial. J Clin Anesth. 2018; 45:12–7. DOI: 10.1016/j.jclinane.2017.11.027. PMID: 29241077.17. Versyck B, van Geffen GJ, Van Houwe P. Prospective double blind randomized placebo-controlled clinical trial of the pectoral nerves (Pecs) block type II. J Clin Anesth. 2017; 40:46–50. DOI: 10.1016/j.jclinane.2017.03.054. PMID: 28625445.18. Liu V, Mariano ER, Prabhakar C. Pecto-intercostal fascial block for acute poststernotomy pain: a case report. A A Pract. 2018; 10:319–22. DOI: 10.1213/XAA.0000000000000697. PMID: 29293481.19. Hong B, Yoon SH, Youn AM, Kim BJ, Song S, Yoon Y. Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report. Korean J Anesthesiol. 2017; 70:209–12. DOI: 10.4097/kjae.2017.70.2.209. PMID: 28367293. PMCID: PMC5370295.20. Blanco R, Parras T, McDonnell JG, Prats-Galino A. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013; 68:1107–13. DOI: 10.1111/anae.12344. PMID: 23923989.21. Ohgoshi Y, Yokozuka M, Terajima K. [Serratus-intercostal plane block for brest surgery]. Masui. 2015; 64:610–4. Japanese. PMID: 26437549.22. Pérez MF, Duany O, de la Torre PA. Redefining PECS blocks for postmastectomy analgesia. Reg Anesth Pain Med. 2015; 40:729–30. DOI: 10.1097/AAP.0000000000000243. PMID: 26488081.23. Pérez MF, Miguel JG, de la Torre PA. A new approach to pectoralis block. Anaesthesia. 2013; 68:430. DOI: 10.1111/anae.12186. PMID: 23488849.24. Leiman D, Barlow M, Carpin K, Piña EM, Casso D. Medial and lateral pectoral nerve block with liposomal bupivacaine for the management of postsurgical pain after submuscular breast augmentation. Plast Reconstr Surg Glob Open. 2015; 2:e282. DOI: 10.1097/GOX.0000000000000253. PMID: 25587516. PMCID: PMC4292264.25. Jaspars JJ, Posma AN, van Immerseel AA, Gittenberger-de Groot AC. The cutaneous innervation of the female breast and nippleareola complex: implications for surgery. Br J Plast Surg. 1997; 50:249–59. DOI: 10.1016/S0007-1226(97)91155-3.26. Kulhari S, Bharti N, Bala I, Arora S, Singh G. Efficacy of pectoral nerve block versus thoracic paravertebral block for postopera- tive analgesia after radical mastectomy: a randomized controlled trial. Br J Anaesth. 2016; 117:382–6. DOI: 10.1093/bja/aew223. PMID: 27543533.27. Hetta DF, Rezk KM. Pectoralis-serratus interfascial plane block vs thoracic paravertebral block for unilateral radical mastectomy with axillary evacuation. J Clin Anesth. 2016; 34:91–7. DOI: 10.1016/j.jclinane.2016.04.003. PMID: 27687353.28. Torre PA, Jones JW Jr, Álvarez SL, Garcia PD, Miguel FJG, Rubio EMM, et al. [Axillary local anesthetic spread after the thoracic interfacial ultrasound block a cadaveric and radiological evaluation]. Rev Bras Anestesiol. 2017; 67:555–64. Portuguese. DOI: 10.1016/j.bjane.2015.04.007.29. Exadaktylos AK, Buggy DJ, Moriarty DC, Mascha E, Sessler DI. Can anesthetic technique for primary breast cancer surgery affect recurrence or metastasis? Anesthesiology. 2006; 105:660–4. DOI: 10.1097/00000542-200610000-00008. PMID: 17006061. PMCID: PMC1615712.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thoracic interfascial nerve block for breast surgery in a pregnant woman: a case report
- Serratus anterior plane block combined with monitored anesthesia care for surgery of lateral side of breast: a case report
- Rhomboid intercostal and subserratus plane block -a case series-
- Analgesic Effect of Erector Spinae Plane Block at T2 Level in Arm Surgery
- Application of unilateral rhomboid intercostal and subserratus plane block for analgesia after laparoscopic cholecystectomy: a quasi-experimental study