Anesth Pain Med.
2019 Apr;14(2):202-207. 10.17085/apm.2019.14.2.202.
The efficacy of vitamin C on postlaparoscopic shoulder pain: a double-blind randomized controlled trial
- Affiliations
-
- 1Departments of Anesthesiology and Pain Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea. anespc@naver.com
- KMID: 2447970
- DOI: http://doi.org/10.17085/apm.2019.14.2.202
Abstract
- BACKGROUND
This study evaluated the effect of vitamin C on post-laparoscopic shoulder pain (PLSP) in patients undergoing benign gynecological surgery during the first 72 h.
METHODS
Sixty patients (aged 20 to 60 years, with American Society of Anesthesiologists physical status classification I or II) scheduled for elective laparoscopic hysterectomy were enrolled in this study. The vitamin C group (Group C) received 500 mg of vitamin C in 50 ml of isotonic saline infusion intravenously twice a day from the day of surgery to the third day after surgery. Patients in the saline group (Group S) received the same volume of isotonic saline over the same period. Post-operative analgesic consumption, pain scores of the incision site and the shoulder, and the incidence of PLSP were all evaluated at 1, 6, 24, 48, and 72 h following surgery.
RESULTS
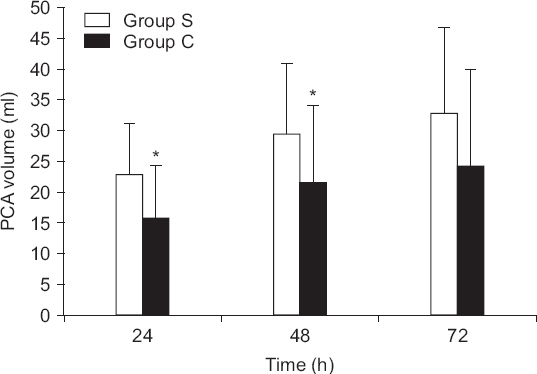
Cumulative post-operative fentanyl consumption was significantly less in Group C at 24 and 48 h after surgery (P = 0.002, P = 0.012, respectively). The pain intensity of PLSP was also significantly lower in Group C 24 h after the operation (P = 0.002). Additionally, the incidence of PLSP was significantly lower in Group C 24 and 48 h after the operation (P = 0.002, P = 0.035, respectively).
CONCLUSIONS
Perioperative intravenous administration of vitamin C (500 mg, twice a day) reduced post-operative analgesic consumption and significantly lowered the pain intensity and incidence of PLSP.
MeSH Terms
Figure
Reference
-
1. Kandil TS, El Hefnawy E. Shoulder pain following laparoscopic cholecystectomy: factors affecting the incidence and severity. J Laparoendosc Adv Surg Tech A. 2010; 20:677–82. DOI: 10.1089/lap.2010.0112. PMID: 20701547.2. Lee DH, Song T, Kim KH, Lee KW. Incidence, natural course, and characteristics of postlaparoscopic shoulder pain. Surg Endosc. 2018; 32:160–5. DOI: 10.1007/s00464-017-5651-5. PMID: 28643053.3. Song T, Kim KH, Lee KW. The intensity of postlaparoscopic shoulder pain is positively correlated with the amount of residual pneumoperitoneum. J Minim Invasive Gynecol. 2017; 24:9849.e1. DOI: 10.1016/j.jmig.2017.06.002. PMID: 28602786.4. Rebec GV, Pierce RC. A vitamin as neuromodulator: ascorbate release into the extracellular fluid of the brain regulates dopaminergic and glutamatergic transmission. Prog Neurobiol. 1994; 43:537–65. DOI: 10.1016/0301-0082(94)90052-3.5. Carr AC, McCall C. The role of vitamin C in the treatment of pain: new insights. J Transl Med. 2017; 15:77. DOI: 10.1186/s12967-017-1179-7. PMID: 28410599. PMCID: PMC5391567.6. Majewska MD, Bell JA. Ascorbic acid protects neurons from injury induced by glutamate and NMDA. Neuroreport. 1990; 1:194–6. DOI: 10.1097/00001756-199011000-00004.7. Majewska MD, Bell JA, London ED. Regulation of the NMDA receptor by redox phenomena: inhibitory role of ascorbate. Brain Res. 1990; 537:328–32. DOI: 10.1016/0006-8993(90)90379-P.8. Jensen NH. [Reduced pain from osteoarthritis in hip joint or knee joint during treatment with calcium ascorbate. A randomized, placebo-controlled cross-over trial in general practice]. Ugeskr Laeger. 2003; 165:2563–6. Danish. PMID: 12854267.9. Besse JL, Gadeyne S, Galand-Desmé S, Lerat JL, Moyen B. Effect of vitamin C on prevention of complex regional pain syndrome type I in foot and ankle surgery. Foot Ankle Surg. 2009; 15:179–82. DOI: 10.1016/j.fas.2009.02.002. PMID: 19840748.10. Jeon Y, Park JS, Moon S, Yeo J. Effect of intravenous high dose vitamin C on postoperative pain and morphine use after laparo- scopic colectomy: a randomized controlled trial. Pain Res Manag. 2016; 2016:9147279. DOI: 10.1155/2016/9147279. PMID: 27872555. PMCID: PMC5107231.11. Ayatollahi V, Dehghanpour Farashah S, Behdad S, Vaziribozorg S, Rabbani Anari M. Effect of intravenous vitamin C on postoperative pain in uvulopalatopharyngoplasty with tonsillectomy. Clin Otolaryngol. 2017; 42:139–43. DOI: 10.1111/coa.12684. PMID: 27219124.12. Kanazi GE, El-Khatib MF, Yazbeck-Karam VG, Hanna JE, Masri B, Aouad MT. Effect of vitamin C on morphine use after laparoscopic cholecystectomy: a randomized controlled trial. Can J Anaesth. 2012; 59:538–43. DOI: 10.1007/s12630-012-9692-x. PMID: 22402954.13. Cason CL, Seidel SL, Bushmiaer M. Recovery from laparoscopic cholecystectomy procedures. AORN J. 1996; 63:1099–103. 1106-8, 1111-2 passim. DOI: 10.1016/S0001-2092(06)63296-1.14. Madsen MR, Jensen KE. Postoperative pain and nausea after laparoscopic cholecystectomy. Surg Laparosc Endosc. 1992; 2:303–5. PMID: 1341550.15. Mouton WG, Bessell JR, Otten KT, Maddern GJ. Pain after laparoscopy. Surg Endosc. 1999; 13:445–8. DOI: 10.1007/s004649901011. PMID: 10227938.16. Fredman B, Jedeikin R, Olsfanger D, Flor P, Gruzman A. Residual pneumoperitoneum: a cause of postoperative pain after laparoscopic cholecystectomy. Anesth Analg. 1994; 79:152–4. DOI: 10.1213/00000539-199407000-00028. PMID: 8010427.17. Sabzi Sarvestani A, Zamiri M. Residual pneumoperitoneum volume and postlaparoscopic cholecystectomy pain. Anesth Pain Med. 2014; 4:e17366. DOI: 10.5812/aapm.17366. PMID: 25599023. PMCID: PMC4286800.18. Sarli L, Costi R, Sansebastiano G, Trivelli M, Roncoroni L. Pro- spective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy. Br J Surg. 2000; 87:1161–5. DOI: 10.1046/j.1365-2168.2000.01507.x. PMID: 10971421.19. Nutthachote P, Sirayapiwat P, Wisawasukmongchol W, Charuluxananan S. A randomized, double-blind, placebo-controlled trial of oral pregabalin for relief of shoulder pain after laparo- scopic gynecologic surgery. J Minim Invasive Gynecol. 2014; 21:669–73. DOI: 10.1016/j.jmig.2014.01.018. PMID: 24473153.20. Tsai HW, Wang PH, Yen MS, Chao KC, Hsu TF, Chen YJ. Prevention of postlaparoscopic shoulder and upper abdominal pain: a randomized controlled trial. Obstet Gynecol. 2013; 121:526–31. DOI: 10.1097/AOG.0b013e318283fcca. PMID: 23635614.21. Kim HK, Park SK, Zhou JL, Taglialatela G, Chung K, Coggeshall RE, et al. Reactive oxygen species (ROS) play an important role in a rat model of neuropathic pain. Pain. 2004; 111:116–24. DOI: 10.1016/j.pain.2004.06.008. PMID: 15327815.22. Rosa KA, Gadotti VM, Rosa AO, Rodrigues AL, Calixto JB, Santos AR. Evidence for the involvement of glutamatergic system in the antinociceptive effect of ascorbic acid. Neurosci Lett. 2005; 381:185–8. DOI: 10.1016/j.neulet.2005.02.032. PMID: 15882814.23. Fukushima R, Yamazaki E. Vitamin C requirement in surgical patients. Curr Opin Clin Nutr Metab Care. 2010; 13:669–76. DOI: 10.1097/MCO.0b013e32833e05bc. PMID: 20689415.24. Padayatty SJ, Sun H, Wang Y, Riordan HD, Hewitt SM, Katz A, et al. Vitamin C pharmacokinetics: implications for oral and intra- venous use. Ann Intern Med. 2004; 140:533–7. DOI: 10.7326/0003-4819-140-7-200404060-00010. PMID: 15068981.25. Levine M, Conry-Cantilena C, Wang Y, Welch RW, Washko PW, Dhariwal KR, et al. Vitamin C pharmacokinetics in healthy volunteers: evidence for a recommended dietary allowance. Proc Natl Acad Sci U S A. 1996; 93:3704–9. DOI: 10.1073/pnas.93.8.3704. PMID: 8623000. PMCID: PMC39676.26. Topçu HO, Cavkaytar S, Kokanalı K, Guzel AI, Islimye M, Doganay M. A prospective randomized trial of postoperative pain following different insufflation pressures during gynecologic laparoscopy. Eur J Obstet Gynecol Reprod Biol. 2014; 182:81–5. DOI: 10.1016/j.ejogrb.2014.09.003. PMID: 25265495.27. Kang S, Brennan TJ. Mechanisms of postoperative pain. Anesth Pain Med. 2016; 11:236–48. DOI: 10.17085/apm.2016.11.3.236.28. Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surg Clin North Am. 2015; 95:301–18. DOI: 10.1016/j.suc.2014.10.002. PMID: 25814108.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correspondence to editorial on “Safety and efficacy of HK-660S in patients with primary sclerosing cholangitis: A randomized double-blind phase 2a trial”
- Effect of multivitamin on serum 25-hydroxy vitamin D level in postmenopausal women: A randomized, double-blind, placebo-controlled trial
- Additional effect of magnesium sulfate and vitamin C in laparoscopic gynecologic surgery for postoperative pain management: a double-blind randomized controlled trial
- Additional low-pressure pulmonary recruitment for reducing post-laparoscopic shoulder pain in gynecologic laparoscopy: a randomized controlled trial
- Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial