Clin Endosc.
2019 Mar;52(2):100-106. 10.5946/ce.2019.012.
Estimation of Invasion Depth: The First Key to Successful Colorectal ESD
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- 2Division of Gastroenterology, Department of Internal Medicine, College of Medicine, Catholic Photomedicine Research Institute, Seoul, Korea.
- 3Cancer Screening Center/Endoscopy Division, National Cancer Center Hospital, Division of Screening Technology, Center for Public Health Sciences, National Cancer Center, Tokyo, Japan. tamatsud@ncc.go.jp
- KMID: 2447665
- DOI: http://doi.org/10.5946/ce.2019.012
Abstract
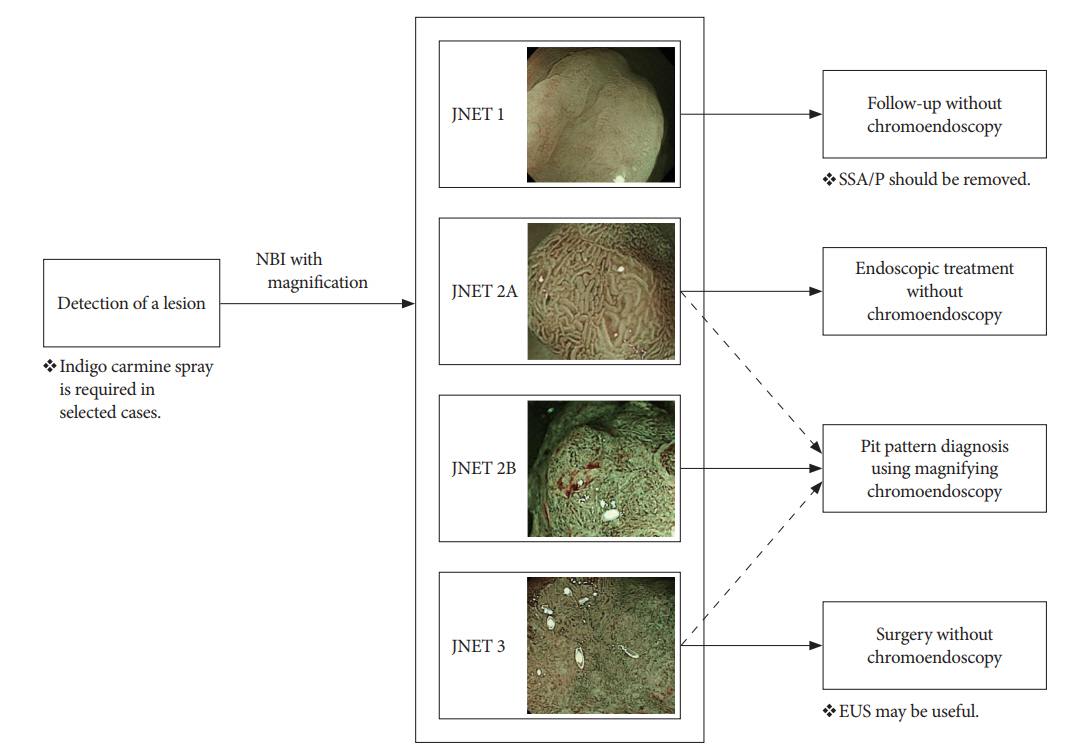
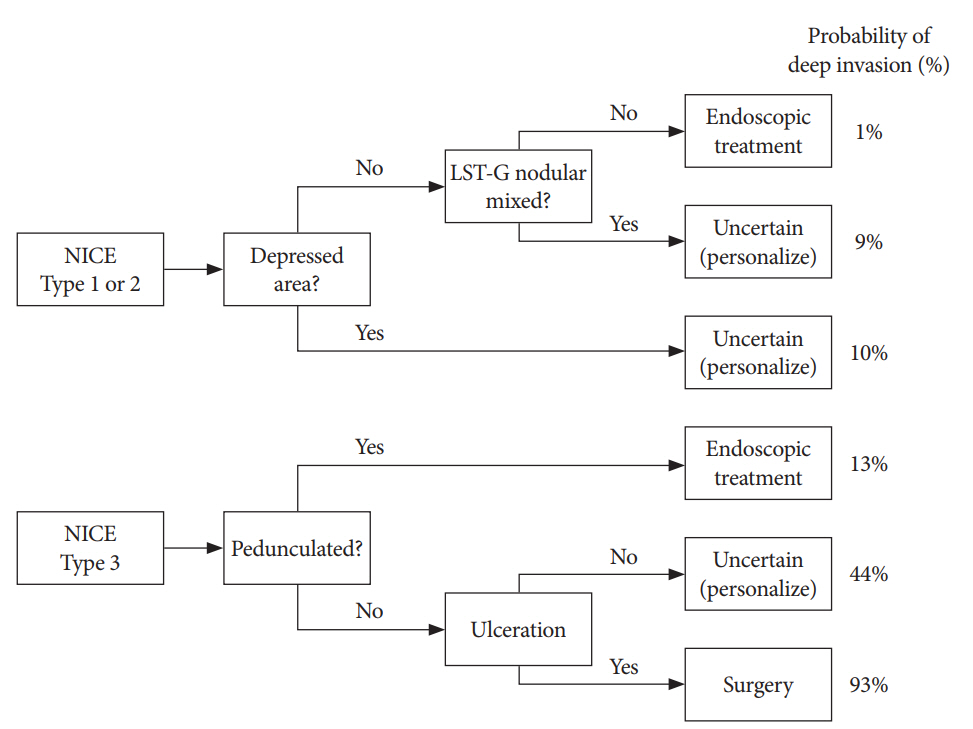
- Colorectal tumors with superficial submucosal invasion, which cannot be removed by snaring, are one of the most optimal indications for colorectal endoscopic submucosal dissection (ESD). Therefore, estimation of the invasion depth is the first key to successful colorectal ESD. Although estimation of the invasion depth based on the gross morphology may be useful in selected cases, its diagnostic accuracy could not reach the clinical requirement. The Japan Narrow-band Imaging (NBI) Expert Team (JNET) classification of NBI magnifying endoscopy findings is a useful method for histologic prediction and invasion depth estimation. However, magnifying chromoendoscopy is still necessary for JNET type 2B lesions to reach a satisfactory diagnostic accuracy. Endocytoscopy with artificial intelligence is a promising technology in invasion depth estimation; however, more data are needed for its clinical application.
MeSH Terms
Figure
Cited by 1 articles
-
Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clin Endosc. 2021;54(5):633-640. doi: 10.5946/ce.2021.216.
Reference
-
1. Morson BC, Whiteway JE, Jones EA, Macrae FA, Williams CB. Histopathology and prognosis of malignant colorectal polyps treated by endoscopic polypectomy. Gut. 1984; 25:437–444.
Article2. Fujimori T, Kawamata H, Kashida H. Precancerous lesions of the colorectum. J Gastroenterol. 2001; 36:587–594.
Article3. Matsuda T, Fujii T, Saito Y, et al. Efficacy of the invasive/non-invasive pattern by magnifying chromoendoscopy to estimate the depth of invasion of early colorectal neoplasms. Am J Gastroenterol. 2008; 103:2700–2706.
Article4. Hewett DG, Sakata S. Classifications for optical diagnosis of colorectal lesions: not 2B with JNET. Gastrointest Endosc. 2017; 85:822–828.5. Watanabe T, Itabashi M, Shimada Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol. 2015; 20:207–239.
Article6. Kitajima K, Fujimori T, Fujii S, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol. 2004; 39:534–543.
Article7. Repici A, Hassan C, De Paula Pessoa D, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy. 2012; 44:137–150.
Article8. Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015; 27:417–434.
Article9. Tanaka S, Oka S, Chayama K. Colorectal endoscopic submucosal dissection: present status and future perspective, including its differentiation from endoscopic mucosal resection. J Gastroenterol. 2008; 43:641–651.
Article10. Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, et al. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015; 47:829–854.
Article11. Bahin FF, Heitman SJ, Rasouli KN, et al. Wide-field endoscopic mucosal resection versus endoscopic submucosal dissection for laterally spreading colorectal lesions: a cost-effectiveness analysis. Gut. 2018; 67:1965–1973.
Article12. Kudo S, Lambert R, Allen JI, et al. Nonpolypoid neoplastic lesions of the colorectal mucosa. Gastrointest Endosc. 2008; 68(4 Suppl):S3–S47.
Article13. Ikehara H, Saito Y, Matsuda T, Uraoka T, Murakami Y. Diagnosis of depth of invasion for early colorectal cancer using magnifying colonoscopy. J Gastroenterol Hepatol. 2010; 25:905–912.
Article14. Park W, Kim B, Park SJ, et al. Conventional endoscopic features are not sufficient to differentiate small, early colorectal cancer. World J Gastroenterol. 2014; 20:6586–6593.
Article15. Choi HJ, Lee BI, Choi H, et al. Diagnostic accuracy and interobserver agreement in predicting the submucosal invasion of colorectal tumors using gross findings, pit patterns, and microvasculatures. Clin Endosc. 2013; 46:168–171.
Article16. Sano Y, Ikematsu H, Fu KI, et al. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointest Endosc. 2009; 69:278–283.
Article17. Kanao H, Tanaka S, Oka S, Hirata M, Yoshida S, Chayama K. Narrow-band imaging magnification predicts the histology and invasion depth of colorectal tumors. Gastrointest Endosc. 2009; 69(3 Pt 2):631–636.
Article18. Wada Y, Kudo SE, Kashida H, et al. Diagnosis of colorectal lesions with the magnifying narrow-band imaging system. Gastrointest Endosc. 2009; 70:522–531.
Article19. Aihara H, Saito S, Tajiri H. Rationale for and clinical benefits of colonoscopy with narrow band imaging: pathological prediction and colorectal screening. Int J Colorectal Dis. 2013; 28:1–7.
Article20. Kim JS, Lee BI, Choi H, et al. Brief education on microvasculature and pit pattern for trainees significantly improves estimation of the invasion depth of colorectal tumors. Gastroenterol Res Pract. 2014; 2014:245396.
Article21. Hewett DG, Kaltenbach T, Sano Y, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology. 2012; 143:599–607.e1.
Article22. Hayashi N, Tanaka S, Hewett DG, et al. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc. 2013; 78:625–632.
Article23. Sano Y, Tanaka S, Kudo SE, et al. Narrow-band imaging (NBI) magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Dig Endosc. 2016; 28:526–533.
Article24. Sano Y, Hirata D, Saito Y. Japan NBI Expert Team classification: narrow-band imaging magnifying endoscopic classification of colorectal tumors. Dig Endosc. 2018; 30:543–545.
Article25. Iwatate M, Sano Y, Tanaka S, et al. Validation study for development of the Japan NBI Expert Team classification of colorectal lesions. Dig Endosc. 2018; 30:642–651.
Article26. Komeda Y, Kashida H, Sakurai T, et al. Magnifying narrow band imaging (NBI) for the diagnosis of localized colorectal lesions using the Japan NBI Expert Team (JNET) classification. Oncology. 2017; 93 Suppl 1:49–54.
Article27. Sumimoto K, Tanaka S, Shigita K, et al. Clinical impact and characteristics of the narrow-band imaging magnifying endoscopic classification of colorectal tumors proposed by the Japan NBI Expert Team. Gastrointest Endosc. 2017; 85:816–821.
Article28. Mani S, Bharagava RN. Exposure to crystal violet, its toxic, genotoxic and carcinogenic effects on environment and its degradation and detoxification for environmental safety. Rev Environ Contam Toxicol. 2016; 237:71–104.
Article29. Onishi T, Tamura S, Kuratani Y, Onishi S, Yasuda N. Evaluation of the depth score of type V pit patterns in crypt orifices of colorectal neoplastic lesions. J Gastroenterol. 2008; 43:291–297.
Article30. Kanao H, Tanaka S, Oka S, et al. Clinical significance of type V(I) pit pattern subclassification in determining the depth of invasion of colorectal neoplasms. World J Gastroenterol. 2008; 14:211–217.31. Matsumoto T, Hizawa K, Esaki M, et al. Comparison of EUS and magnifying colonoscopy for assessment of small colorectal cancers. Gastrointest Endosc. 2002; 56:354–360.
Article32. Hurlstone DP, Brown S, Cross SS, Shorthouse AJ, Sanders DS. High magnification chromoscopic colonoscopy or high frequency 20 MHz mini probe endoscopic ultrasound staging for early colorectal neoplasia: a comparative prospective analysis. Gut. 2005; 54:1585–1589.
Article33. Shimura T, Ebi M, Yamada T, et al. Magnifying chromoendoscopy and endoscopic ultrasonography measure invasion depth of early stage colorectal cancer with equal accuracy on the basis of a prospective trial. Clin Gastroenterol Hepatol. 2014; 12:662–668. e1-e2.
Article34. Kudo SE, Wakamura K, Ikehara N, Mori Y, Inoue H, Hamatani S. Diagnosis of colorectal lesions with a novel endocytoscopic classification - a pilot study. Endoscopy. 2011; 43:869–875.
Article35. Takeda K, Kudo SE, Mori Y, et al. Accuracy of diagnosing invasive colorectal cancer using computer-aided endocytoscopy. Endoscopy. 2017; 49:798–802.
Article36. Nishizawa T, Yahagi N. Endoscopic mucosal resection and endoscopic submucosal dissection: technique and new directions. Curr Opin Gastroenterol. 2017; 33:315–319.37. Puig I, López-Cerón M, Arnau A, et al. Accuracy of the narrow-band imaging international colorectal endoscopic classification system in identification of deep invasion in colorectal polyps. Gastroenterology. 2019; 156:75–87.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indications, Knives, and Electric Current: What's the Best?
- The submucosal fibrosis: what does it mean for colorectal endoscopic submucosal dissection?
- Endoscopic Submucosal Dissection for Colorectal Neoplasia: Early Outcomes After 260 Cases
- Debates on Colorectal Endoscopic Submucosal Dissection - Traction for Effective Dissection: Gravity Is Enough
- International Digestive Endoscopy Network to Strengthen Network for Lower Gastrointestinal Diseases Including Inflammatory Bowel Disease and Colorectal Cancer