J Korean Ophthalmol Soc.
2019 May;60(5):414-420. 10.3341/jkos.2019.60.5.414.
Changes in Total Tear Protein and Lipocalin Concentration According to Frequency of Artificial Tear Usage
- Affiliations
-
- 1Cheil Eye Hospital, Daegu, Korea. jck50ey@daum.net
- 2Department of Ophthalmology, Chung-Ang University College of Medicine, Seoul, Korea.
- KMID: 2445133
- DOI: http://doi.org/10.3341/jkos.2019.60.5.414
Abstract
- PURPOSE
To investigate the effect of frequent use of artificial tears on dry eye syndrome (DES) by analyzing the changes in total protein concentration, lipocalin concentration, and the ratio of lipocalin-to-total protein concentration in tears.
METHODS
A prospective study was performed on 24 eyes of patients with DES and 24 eyes of control subjects. Artificial eye drops were applied a total of eight times (15-minutes intervals) to all participants. The concentrations of total protein and lipocalin in tears were analyzed before, and after one, two, four, and eight applications. The ratio of lipocalin-to-total protein concentration was also analyzed.
RESULTS
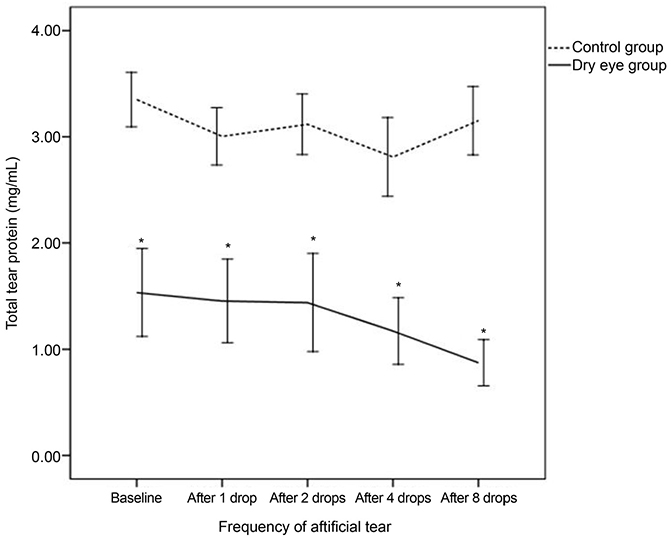
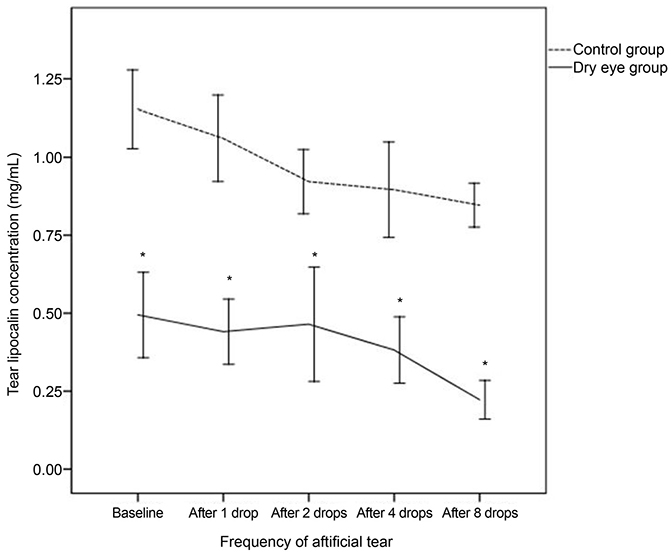
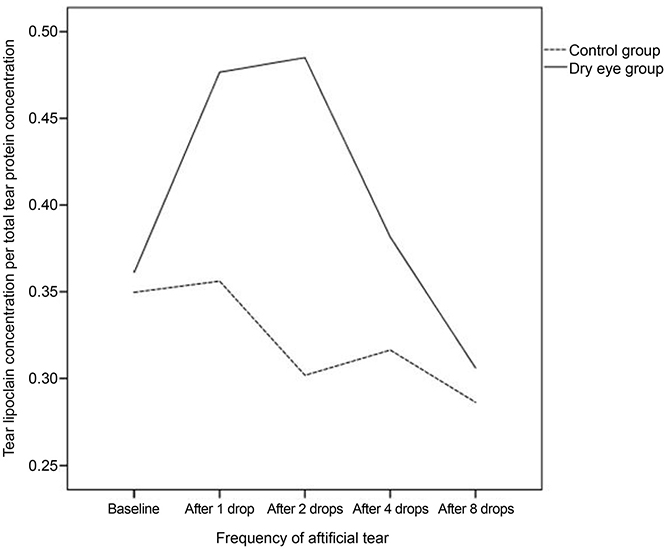
Total tear potein concentration of 3.35 mg/mL had decreased to 3.16 mg/mL after use of artificial tears for control while it had decreased from 1.53 to 0.87 mg/mL for patients. Both groups showed significant decrease (p = 0.04, p < 0.01, respectively). Lipocalin concentration also showed significant decreases in both control and DES patients for all applications (from 1.15 to 0.85 mg/mL for control, and from 0.49 to 0.22 mg/mL for DES patients, both, p < 0.01). The change in the ratio of lipocalin-to-total protein concentration was significant in the control group (p = 0.03) but not in the patient group (p = 0.21).
CONCLUSIONS
A significant decrease was observed in the concentrations of total protein and lipocalin in the DES patient group. The ratio of lipocalin-to-total protein concentration was also significantly decreased when eye drops were applied four times. These results suggested that the frequent use of artificial eye drops exacerbated DES.
MeSH Terms
Figure
Reference
-
1. Lemp MA. Report of the national eye institute/industry workshop on clinical trials in dry eyes. CLAO J. 1995; 21:221–232.2. Srinivasan S, Thangavelu M, Zhang L, et al. iTRAQ quantitative proteomics in the analysis of tears in dry eye patients. Invest Ophthalmol Vis Sci. 2012; 53:5052–5059.
Article3. Ohashi Y, Dogru M, Tsubota K. Laboratory findings in tear fluid analysis. Clin Chim Acta. 2006; 369:17–28.
Article4. Van Haeringen NJ. Clinical biochemistry of tears. Surv Ophthalmol. 1981; 26:84–96.
Article5. Grus FH, Augustin AJ. Protein analysis methods in diagnosis of sicca syndrome. Ophthalmologe. 2000; 97:54–61.6. Grus FH, Augustin AJ. Analysis of tear protein patterns by a neural network as a diagnostical tool for the detection of dry eyes. Electrophoresis. 1999; 20:875–880.
Article7. Kijlstra A, Kuizenga A. Analysis and function of the human tear proteins. Adv Exp Med Biol. 1994; 350:299–308.
Article8. Shigeyasu C, Yamada M, Akune Y. Influence of ophthalmic solutions on tear components. Cornea. 2016; 35:Suppl 1. S71–S77.
Article9. Versura P, Nanni P, Bavelloni A, et al. Tear proteomics in evaporative dry eye disease. Eye (Lond). 2010; 24:1396–1402.
Article10. Versura P, Bavelloni A, Grillini M, et al. Diagnostic performance of a tear protein panel in early dry eye. Mol Vis. 2013; 19:1247–1257.11. Zhou L, Beuerman RW, Chan CM, et al. Identification of tear fluid biomarkers in dry eye syndrome using iTRAQ quantitative proteomics. J Proteome Res. 2009; 8:4889–4905.
Article12. de Souza GA, Godoy LM, Mann M. Identification of 491 proteins in the tear fluid proteome reveals a large number of proteases and protease inhibitors. Genome Biol. 2006; 7:R72.13. Dartt DA. Tear lipocalin: structure and function. Ocul Surf. 2011; 9:126–138.
Article14. Lemp MA, Hamill JR Jr. Factors affecting tear film breakup in normal eyes. Arch Ophthalmol. 1973; 89:103–105.
Article15. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003; 22:640–650.
Article16. Posa A, Bräuer L, Schicht M, et al. Schirmer strip vs. capillary tube method: non-invasive methods of obtaining proteins from tear fluid. Ann Anat. 2013; 195:137–142.
Article17. Fullard RJ, Kissner DM. Purification of the isoforms of tear specific prealbumin. Curr Eye Res. 1991; 10:613–628.
Article18. Inada K. Studies of human tear proteins. 3. Distribution of specific tear prealbumin in lacrimal glands and other ocular adnexa. Jpn J Ophthalmol. 1984; 28:315–330.19. Bläker M, Kock K, Ahlers C, et al. Molecular cloning of human von Ebner's gland protein, a member of the lipocalin superfamily highly expressed in lingual salivary glands. Biochim Biophys Acta. 1993; 1172:131–137.
Article20. Redl B, Holzfeind P, Lottspeich F. cDNA cloning and sequencing reveals human tear prealbumin to be a member of the lipophilic-ligand carrier protein superfamily. J Biol Chem. 1992; 267:20282–20287.
Article21. Glasgow BJ, Marshall G, Gasymov OK, et al. Tear lipocalins: potential lipid scavengers for the corneal surface. Invest Ophthalmol Vis Sci. 1999; 40:3100–3107.22. Glasgow BJ, Abduragimov AR, Farahbakhsh ZT, et al. Tear lipocalins bind a broad array of lipid ligands. Curr Eye Res. 1995; 14:363–372.
Article23. Gasymov OK, Abduragimov AR, Yusifov TN, Glasgow BJ. Binding studies of tear lipocalin: the role of the conserved tryptophan in maintaining structure, stability and ligand affinity. Biochim Biophys Acta. 1999; 1433:307–320.
Article24. Nagyová B, Tiffany JM. Components responsible for the surface tension of human tears. Curr Eye Res. 1999; 19:4–11.
Article25. Shigeyasu C, Hirano S, Akune Y, et al. Evaluation of the frequency of ophthalmic solution application: washout effects of topical saline application on tear components. Curr Eye Res. 2013; 38:722–728.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Quantitative Analysis of Tear Total Protein and Lysozyme in Normal and Diabetes
- Wavefront Aberration Changes after the Instillation of Artificial Tear in Dry Eyes
- Comparative Analysis of the Tear Protein Expression After Photorefractive Keratectomy Using Two-Dimensional Electrophoresis
- Analysis of Tear Composition in Chronic Blepharitis
- The Changes of Tear Osmolarity and Protein After Silicone Punctal Plug Insertion In Dry Eye