Korean J Neurotrauma.
2019 Apr;15(1):50-54. 10.13004/kjnt.2019.15.e1.
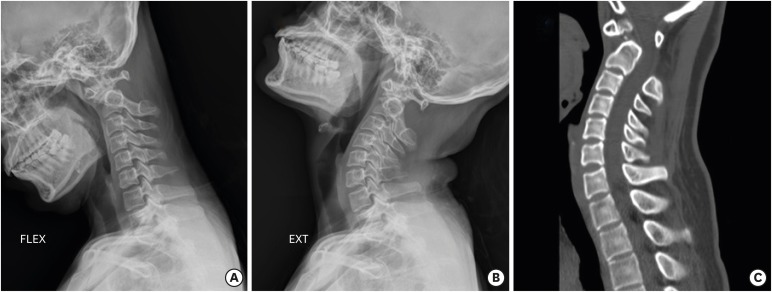
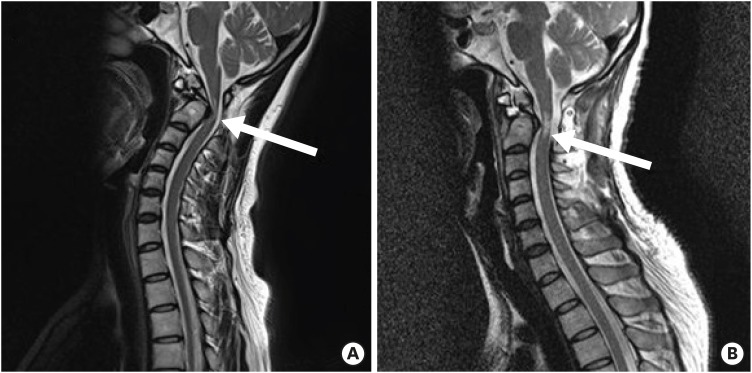
What Causes Severe Myelopathy Resulting in Acute Quadriplegia after a Surgery for Atlantoaxial Subluxation due to Os Odontoideum? A Case Report
- Affiliations
-
- 1Department of Neurosurgery, Inje University Busan Paik Hospital, Inje University School of Medicine, Busan, Korea. shpaeng@empas.com
- KMID: 2444206
- DOI: http://doi.org/10.13004/kjnt.2019.15.e1
Abstract
- A case of acute quadriplegia resulting from reduction of atlantoaxial subluxation due to os odontoideum is rare. Patient with os odontoideum are at a greater risk for atlantoaxial instability and resultant spinal cord compression. In our case, the patient exhibited mild myelopathic symptoms before the onset of acute quadriplegia. Owing to the clinical presentations, the spinal cord not only seemed to suffer a mechanical compression but also an insufï¬ciency of blood supply to the spinal artery and its branches. No other report has described the findings from magnetic resonance imaging before and after the onset of acute myelopathy after surgery. The aim of our case report is to highlight the pathophysiology and appropriate management strategy of a patient with severe progressive spinal cord myelopathy after surgery, secondary to chronic atlantoaxial subluxation due to os odontoideum. This case depicts the presence of this rare yet possible complication, and emphasizes the importance of preoperative evaluation in cases with chronic progressive myelopathy. Moreover, urgent postoperative treatment and rehabilitation are important for the recovery of neurological symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Arvin B, Fournier-Gosselin MP, Fehlings MG. Os odontoideum: etiology and surgical management. Neurosurgery. 2010; 66:22–31. PMID: 20173524.2. Bach CM, Arbab D, Thaler M. Treatment strategies for severe C1C2 luxation due to congenital os odontoideum causing tetraplegia. Eur Spine J. 2013; 22:29–35. PMID: 22581189.
Article3. Fercakova A, Halat G, Marsala M, Lukacova N, Marsala J. Graded postischemic reoxygenation reduces lipid peroxidation and reperfusion injury in the rabbit spinal cord. Brain Res. 1992; 593:159–167. PMID: 1450926.
Article4. Hasegawa K, Homma T, Chiba Y. Upper extremity palsy following cervical decompression surgery results from a transient spinal cord lesion. Spine (Phila Pa 1976). 2007; 32:E197–E202. PMID: 17413460.
Article5. Klimo P Jr, Kan P, Rao G, Apfelbaum R, Brockmeyer D. Os odontoideum: presentation, diagnosis, and treatment in a series of 78 patients. J Neurosurg Spine. 2008; 9:332–342. PMID: 18939918.
Article6. Moore WM Jr, Hollier LH. The influence of severity of spinal cord ischemia in the etiology of delayed-onset paraplegia. Ann Surg. 1991; 213:427–431. PMID: 2025062.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Indirect Decompression using Segmental Screw Fixation for Cervical Myelopathy Caused by C1-2 Subluxation: Technical Note
- Retro-odontoid Synovial Cyst with Os Odontoideum and Atlantoaxial Instability
- A Concomitant Occurrence of the Atlantoaxial Subluxation with Rare Vertebral Formation and Segmentation Defects
- Cervical Myelopathy Resulting From Non-Rheumatoid Atlantoaxial Subluxation
- Quadriplegia and Dyspnea Caused by Os Odontoideum in a Down Syndrome Patient: A case report