Predictors of the Therapeutic Efficacy and Consideration of the Best Combination Therapy of Sodium-Glucose Co-transporter 2 Inhibitors
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea. edgo@yuhs.ac
- 2Brain Korea 21 Plus Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- 3Institute of Endocrine Research, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2442769
- DOI: http://doi.org/10.4093/dmj.2018.0057
Abstract
- BACKGROUND
We investigated the predictive markers for the therapeutic efficacy and the best combination of sodium-glucose co-transporter 2 (SGLT2) inhibitors (empagliflozin, dapagliflozin, and ipragliflozin) therapy in patients with type 2 diabetes mellitus (T2DM).
METHODS
A total of 804 patients with T2DM who had taken SGLT2 inhibitor as monotherapy or an add-on therapy were analyzed. Multivariate regression analyses were performed to identify the predictors of SGLT2 inhibitor response including the classes of baseline anti-diabetic medications.
RESULTS
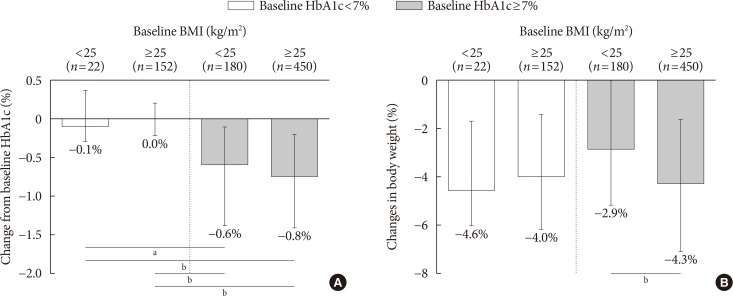
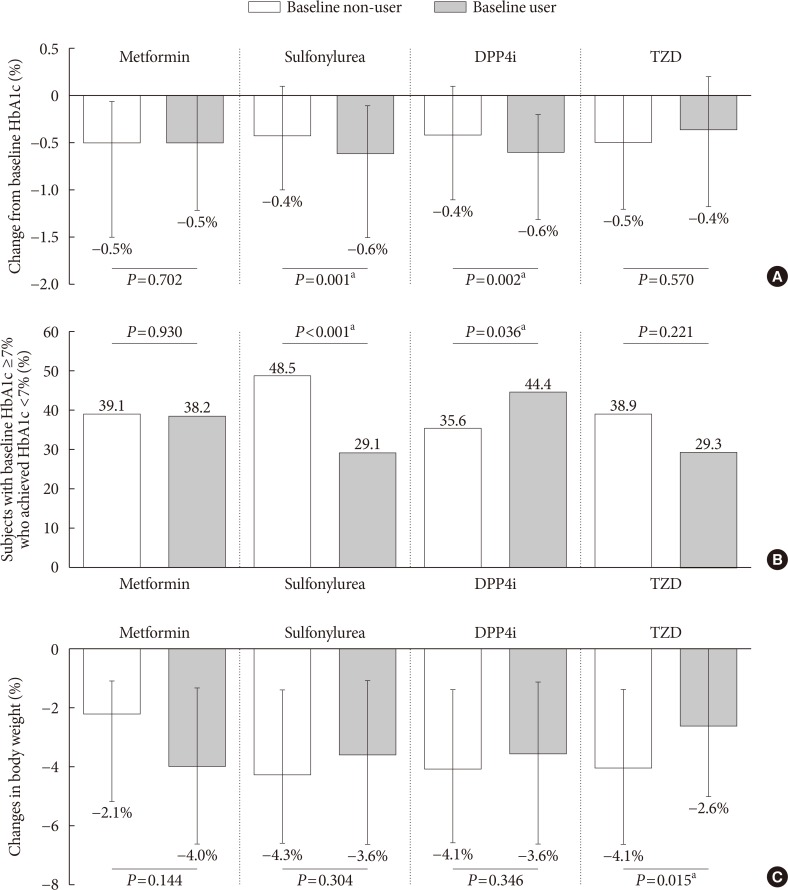
After adjusting for age, sex, baseline body mass index (BMI), diabetes duration, duration of SGLT2 inhibitor use, initial glycosylated hemoglobin (HbA1c) level, estimated glomerular filtration rate (eGFR), and other anti-diabetic agent usage, multivariate analysis revealed that shorter diabetes duration, higher initial HbA1c and eGFR were associated with better glycemic response. However, baseline BMI was inversely correlated with glycemic status; lean subjects with well-controlled diabetes and obese subjects with inadequately controlled diabetes received more benefit from SGLT2 inhibitor treatment. In addition, dipeptidyl peptidase 4 (DPP4) inhibitor use was related to a greater reduction in HbA1c in patients with higher baseline HbA1c ≥7%. Sulfonylurea users experienced a larger change from baseline HbA1c but the significance was lost after adjustment for covariates and metformin and thiazolidinedione use did not affect the glycemic outcome.
CONCLUSION
A better response to SGLT2 inhibitors is expected in Korean T2DM patients who have higher baseline HbA1c and eGFR with a shorter diabetes duration. Moreover, the add-on of an SGLT2 inhibitor to a DPP4 inhibitor is likely to show the greatest glycemic response.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Sodium-Glucose Cotransporter-2 Inhibitor for Renal Function Preservation in Patients with Type 2 Diabetes Mellitus: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Tae Jung Oh, Ju-Young Moon, Kyu Yeon Hur, Seung Hyun Ko, Hyun Jung Kim, Taehee Kim, Dong Won Lee, Min Kyong Moon, ,
Diabetes Metab J. 2020;44(4):489-497. doi: 10.4093/dmj.2020.0172.Effect of Dapagliflozin as an Add-on Therapy to Insulin on the Glycemic Variability in Subjects with Type 2 Diabetes Mellitus (DIVE): A Multicenter, Placebo-Controlled, Double-Blind, Randomized Study
Seung-Hwan Lee, Kyung-Wan Min, Byung-Wan Lee, In-Kyung Jeong, Soon-Jib Yoo, Hyuk-Sang Kwon, Yoon-Hee Choi, Kun-Ho Yoon
Diabetes Metab J. 2021;45(3):339-348. doi: 10.4093/dmj.2019.0203.Efficacy and Safety of Evogliptin Add-on Therapy to Dapagliflozin/Metformin Combinations in Patients with Poorly Controlled Type 2 Diabetes Mellitus: A 24-Week Multicenter Randomized Placebo-Controlled Parallel-Design Phase-3 Trial with a 28-Week Extension
Jun Sung Moon, Il Rae Park, Hae Jin Kim, Choon Hee Chung, Kyu Chang Won, Kyung Ah Han, Cheol-Young Park, Jong Chul Won, Dong Jun Kim, Gwan Pyo Koh, Eun Sook Kim, Jae Myung Yu, Eun-Gyoung Hong, Chang Beom Lee, Kun-Ho Yoon
Diabetes Metab J. 2023;47(6):808-817. doi: 10.4093/dmj.2022.0387.
Reference
-
1. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010; 87:4–14. PMID: 19896746.
Article2. Emerging Risk Factors Collaboration. Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, Di Angelantonio E, Ingelsson E, Lawlor DA, Selvin E, Stampfer M, Stehouwer CD, Lewington S, Pennells L, Thompson A, Sattar N, White IR, Ray KK, Danesh J. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010; 375:2215–2222. PMID: 20609967.3. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352:837–853. PMID: 9742976.4. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008; 359:1577–1589. PMID: 18784090.
Article5. Hayward RA, Reaven PD, Wiitala WL, Bahn GD, Reda DJ, Ge L, McCarren M, Duckworth WC, Emanuele NV. VADT Investigators. Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015; 372:2197–2206. PMID: 26039600.
Article6. Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in U.S. diabetes care, 1999–2010. N Engl J Med. 2013; 368:1613–1624. PMID: 23614587.
Article7. Montvida O, Shaw J, Atherton JJ, Stringer F, Paul SK. Long-term trends in antidiabetes drug usage in the U.S.: real-world evidence in patients newly diagnosed with type 2 diabetes. Diabetes Care. 2018; 41:69–78. PMID: 29109299.
Article9. Chao EC, Henry RR. SGLT2 inhibition: a novel strategy for diabetes treatment. Nat Rev Drug Discov. 2010; 9:551–559. PMID: 20508640.10. Ferrannini E, Ramos SJ, Salsali A, Tang W, List JF. Dapagliflozin monotherapy in type 2 diabetic patients with inadequate glycemic control by diet and exercise: a randomized, double-blind, placebo-controlled, phase 3 trial. Diabetes Care. 2010; 33:2217–2224. PMID: 20566676.11. Jung CH, Jang JE, Park JY. A novel therapeutic agent for type 2 diabetes mellitus: SGLT2 inhibitor. Diabetes Metab J. 2014; 38:261–273. PMID: 25215272.
Article12. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE. EMPA-REG OUTCOME Investigators. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–2128. PMID: 26378978.
Article13. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR. CANVAS Program Collaborative Group. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017; 377:644–657. PMID: 28605608.
Article14. Lee JY, Kim G, Kim SR, Lee YH, Lee BW, Cha BS, Kang ES. Clinical parameters affecting dapagliflozin response in patients with type 2 diabetes. Diabetes Metab. 2017; 43:191–194. PMID: 28089373.
Article15. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999; 130:461–470. PMID: 10075613.16. Defronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes. 2009; 58:773–795. PMID: 19336687.17. Ahren B, Landin-Olsson M, Jansson PA, Svensson M, Holmes D, Schweizer A. Inhibition of dipeptidyl peptidase-4 reduces glycemia, sustains insulin levels, and reduces glucagon levels in type 2 diabetes. J Clin Endocrinol Metab. 2004; 89:2078–2084. PMID: 15126524.18. Merovci A, Solis-Herrera C, Daniele G, Eldor R, Fiorentino TV, Tripathy D, Xiong J, Perez Z, Norton L, Abdul-Ghani MA, DeFronzo RA. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J Clin Invest. 2014; 124:509–514. PMID: 24463448.
Article19. Abdul-Ghani M. Where does combination therapy with an SGLT2 inhibitor plus a DPP-4 inhibitor fit in the management of type 2 diabetes? Diabetes Care. 2015; 38:373–375. PMID: 25715413.
Article20. Rosenstock J, Hansen L, Zee P, Li Y, Cook W, Hirshberg B, Iqbal N. Dual add-on therapy in type 2 diabetes poorly controlled with metformin monotherapy: a randomized double-blind trial of saxagliptin plus dapagliflozin addition versus single addition of saxagliptin or dapagliflozin to metformin. Diabetes Care. 2015; 38:376–383. PMID: 25352655.
Article21. DeFronzo RA, Lewin A, Patel S, Liu D, Kaste R, Woerle HJ, Broedl UC. Combination of empagliflozin and linagliptin as second-line therapy in subjects with type 2 diabetes inadequately controlled on metformin. Diabetes Care. 2015; 38:384–393. PMID: 25583754.
Article22. Strojek K, Yoon KH, Hruba V, Elze M, Langkilde AM, Parikh S. Effect of dapagliflozin in patients with type 2 diabetes who have inadequate glycaemic control with glimepiride: a randomized, 24-week, double-blind, placebo-controlled trial. Diabetes Obes Metab. 2011; 13:928–938. PMID: 21672123.
Article23. Bujac S, Del Parigi A, Sugg J, Grandy S, Liptrot T, Karpefors M, Chamberlain C, Boothman AM. Patient characteristics are not associated with clinically important differential response to dapagliflozin: a staged analysis of phase 3 data. Diabetes Ther. 2014; 5:471–482. PMID: 25502227.
Article24. Ferrannini E, Veltkamp SA, Smulders RA, Kadokura T. Renal glucose handling: impact of chronic kidney disease and sodium-glucose cotransporter 2 inhibition in patients with type 2 diabetes. Diabetes Care. 2013; 36:1260–1265. PMID: 23359360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Response: Predictors of the Therapeutic Efficacy and Consideration of the Best Combination Therapy of Sodium-Glucose Co-transporter 2 Inhibitors (Diabetes Metab J 2019;43:158–73)
- Letter: Predictors of the Therapeutic Efficacy and Consideration of the Best Combination Therapy of Sodium-Glucose Co-transporter 2 Inhibitors (Diabetes Metab J 2019;43:158–73)
- Glucose Lowering Effect of SGLT2 Inhibitors: A Review of Clinical Studies
- Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitor
- SGLT2 Inhibitors and Ketoacidosis: Pathophysiology and Management