Korean J Radiol.
2019 May;20(5):844-853. 10.3348/kjr.2018.0555.
Learning Curve of C-Arm Cone-beam Computed Tomography Virtual Navigation-Guided Percutaneous Transthoracic Needle Biopsy
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Institute of Radiation Medicine, Seoul, Korea. cmpark.morphius@gmail.com
- 2Department of Radiology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea.
- 3Cancer Research Institute, Seoul National University, Seoul, Korea.
- KMID: 2442718
- DOI: http://doi.org/10.3348/kjr.2018.0555
Abstract
OBJECTIVE
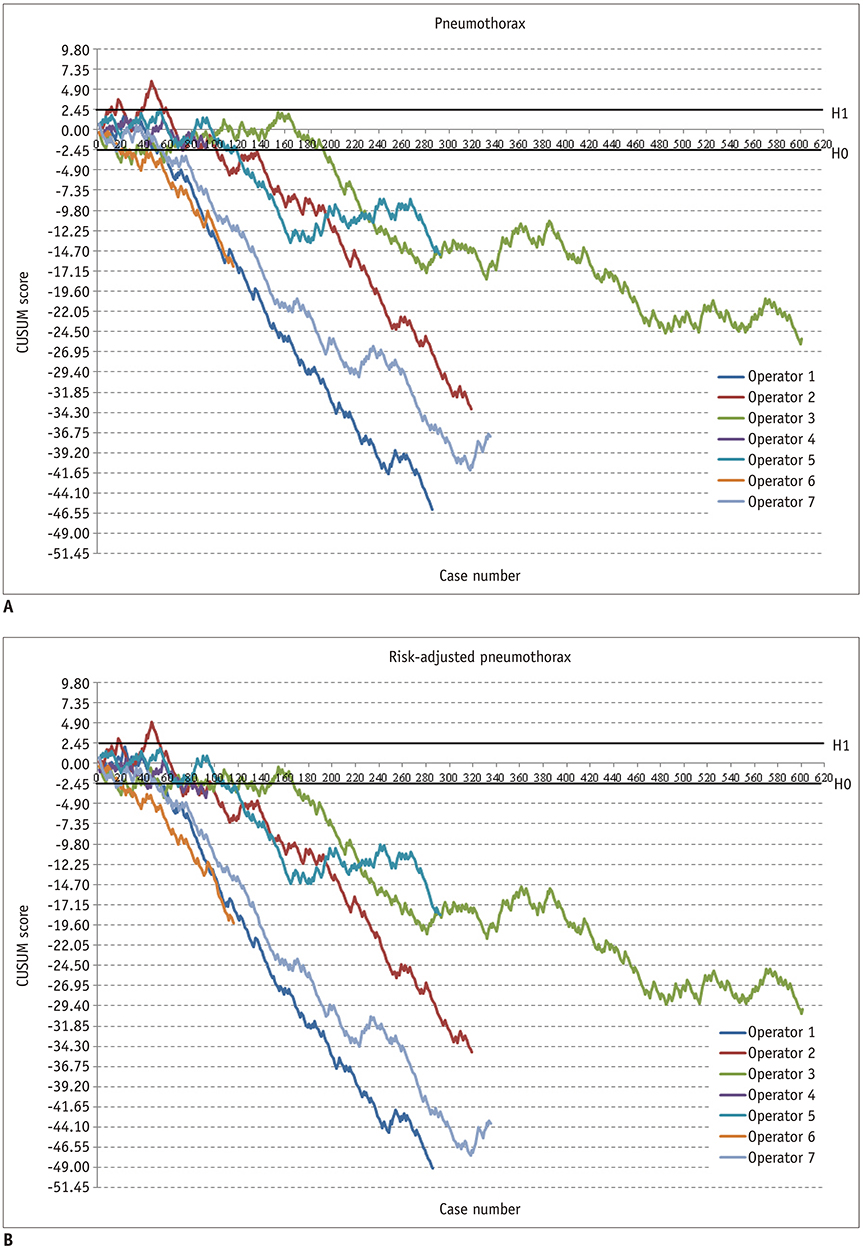
To evaluate the learning curve for C-arm cone-beam computed tomography (CBCT) virtual navigation-guided percutaneous transthoracic needle biopsy (PTNB) and to determine the amount of experience needed to develop appropriate skills for this procedure using cumulative summation (CUSUM).
MATERIALS AND METHODS
We retrospectively reviewed 2042 CBCT virtual navigation-guided PTNBs performed by 7 novice operators between March 2011 and December 2014. Learning curves for CBCT virtual navigation-guided PTNB with respect to its diagnostic performance and the occurrence of biopsy-related pneumothorax were analyzed using standard and risk-adjusted CUSUM (RA-CUSUM). Acceptable failure rates were determined as 0.06 for diagnostic failure and 0.25 for PTNB-related pneumothorax.
RESULTS
Standard CUSUM indicated that 6 of the 7 operators achieved an acceptable diagnostic failure rate after a median of 105 PTNB procedures (95% confidence interval [CI], 14-240), and 6 of the operators achieved acceptable pneumothorax occurrence rate after a median of 79 PTNB procedures (95% CI, 27-155). RA-CUSUM showed that 93 (95% CI, 39-142) and 80 (95% CI, 38-127) PTNB procedures were required to achieve acceptable diagnostic performance and pneumothorax occurrence, respectively.
CONCLUSION
The novice operators' skills in performing CBCT virtual navigation-guided PTNBs improved with increasing experience over a wide range of learning periods.
Keyword
MeSH Terms
Figure
Reference
-
1. Ost DE, Gould MK. Decision making in patients with pulmonary nodules. Am J Respir Crit Care Med. 2012; 185:363–372.
Article2. Callister ME, Baldwin DR, Akram AR, Barnard S, Cane P, Draffan J, et al. British Thoracic Society guidelines for the investigation and management of pulmonary nodules: accredited by NICE. Thorax. 2015; 70:ii1–ii54.
Article3. Gould MK, Fletcher J, Iannettoni MD, Lynch WR, Midthun DE, Naidich DP, et al. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines. Chest. 2007; 132:3 Suppl. 108S–130S.4. Wisnivesky JP, Henschke CI, Yankelevitz DF. Diagnostic percutaneous transthoracic needle biopsy does not affect survival in stage I lung cancer. Am J Respir Crit Care Med. 2006; 174:684–688.
Article5. Choo JY, Park CM, Lee NK, Lee SM, Lee HJ, Goo JM. Percutaneous transthoracic needle biopsy of small (≤1 cm) lung nodules under C-arm cone-beam CT virtual navigation guidance. Eur Radiol. 2013; 23:712–719.6. Lee SM, Park CM, Lee KH, Bahn YE, Kim JI, Goo JM. C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: clinical experience in 1108 patients. Radiology. 2014; 271:291–300.
Article7. Lim HJ, Park CM, Yoon SH, Bae JS, Goo JM. Cone-beam CT virtual navigation-guided percutaneous needle biopsy of suspicious pleural metastasis: a pilot study. Korean J Radiol. 2018; 19:872–879.
Article8. Page ES. Continuous inspection schemes. Biometrika. 1954; 41:100–115.
Article9. Yelle LE. The learning curve: historical review and comprehensive survey. Decision sciences. 1979; 10:302–328.
Article10. Biau DJ, Resche-Rigon M, Godiris-Petit G, Nizard RS, Porcher R. Quality control of surgical and interventional procedures: a review of the CUSUM. Qual Saf Health Care. 2007; 16:203–207.
Article11. Rogers CA, Reeves BC, Caputo M, Ganesh JS, Bonser RS, Angelini GD. Control chart methods for monitoring cardiac surgical performance and their interpretation. J Thorac Cardiovasc Surg. 2004; 128:811–819.
Article12. Komatsu R, Kasuya Y, Yogo H, Sessler DI, Mascha E, Yang D, et al. Learning curves for bag-and-mask ventilation and orotracheal intubation: an application of the cumulative sum method. Anesthesiology. 2010; 112:1525–1531.13. Cundy TP, Gattas NE, White AD, Najmaldin AS. Learning curve evaluation using cumulative summation analysis-a clinical example of pediatric robot-assisted laparoscopic pyeloplasty. J Pediatr Surg. 2015; 50:1368–1373.
Article14. Usluer O, Kaya SO. Endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal lymphadenopathy: effect of the learning curve. Interact Cardiovasc Thorac Surg. 2014; 19:693–695.
Article15. Kemp SV, El Batrawy SH, Harrison RN, Skwarski K, Munavvar M, Rosell A, et al. Learning curves for endobronchial ultrasound using analysis. Thorax. 2010; 65:534–538.16. Groth SS, Whitson BA, D’Cunha J, Maddaus MA, Alsharif M, Andrade RS. Endobronchial ultrasound-guided fine-needle aspiration of mediastinal lymph nodes: a single institution's early learning curve. Ann Thorac Surg. 2008; 86:1104–1109. discussion 1109-1110.
Article17. Sun J, Xie F, Zheng X, Jiang Y, Zhu L, Mao X, et al. Learning curve of electromagnetic navigation bronchoscopy for diagnosing peripheral pulmonary nodules in a single institution. Translational Cancer Research. 2017; 6:541–551.
Article18. Kim JI, Park CM, Kim H, Lee JH, Goo JM. Non-specific benign pathological results on transthoracic core-needle biopsy: how to differentiate false-negatives? Eur Radiol. 2017; 27:3888–3895.
Article19. Bolsin S, Colson M. The use of the CUSUM technique in the assessment of trainee competence in new procedures. Int J Qual Health Care. 2000; 12:433–438.
Article20. Yan GW, Bhetuwal A, Yan GW, Sun QQ, Niu XK, Zhou Y, et al. A systematic review and meta-analysis of C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules. Pol J Radiol. 2017; 82:152–160.
Article21. Lim WH, Park CM, Yoon SH, Lim HJ, Hwang EJ, Lee JH, et al. Time-dependent analysis of incidence, risk factors and clinical significance of pneumothorax after percutaneous lung biopsy. Eur Radiol. 2018; 28:1328–1337.
Article22. Gupta S, Wallace MJ, Cardella JF, Kundu S, Miller DL, Rose SC. Quality improvement guidelines for percutaneous needle biopsy. J Vasc Interv Radiol. 2010; 21:969–975.
Article23. Matheny ME, Ohno-Machado L, Resnic FS. Risk-adjusted sequential probability ratio test control chart methods for monitoring operator and institutional mortality rates in interventional cardiology. Am Heart J. 2008; 155:114–120.
Article24. Dessolle L, Fréour T, Barrière P, Jean M, Ravel C, Daraï E, et al. How soon can I be proficient in embryo transfer? Lessons from the cumulative summation test for learning curve (LC-CUSUM). Hum Reprod. 2010; 25:380–386.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predicting Factors for Conversion from Fluoroscopy Guided Percutaneous Transthoracic Needle Biopsy to Cone-Beam CT Guided Percutaneous Transthoracic Needle Biopsy
- Cone-Beam CT Virtual Navigation-Guided Percutaneous Needle Biopsy of Suspicious Pleural Metastasis: A Pilot Study
- Transthoracic needle biopsy for diagnosis of lung cancer
- Air Embolization after Computed Tomography-Guided Percutaneous Transthoracic Needle Biopsy
- Combined Fluoroscopy- and CT-Guided Transthoracic Needle Biopsy Using a C-Arm Cone-Beam CT System: Comparison with Fluoroscopy-Guided Biopsy