J Korean Diabetes.
2019 Mar;20(1):33-41. 10.4093/jkd.2019.20.1.33.
Interventional and Surgical Treatment of Peripheral Artery Disease in Diabetic Patients
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. kimsang978@naver.com
- KMID: 2442351
- DOI: http://doi.org/10.4093/jkd.2019.20.1.33
Abstract
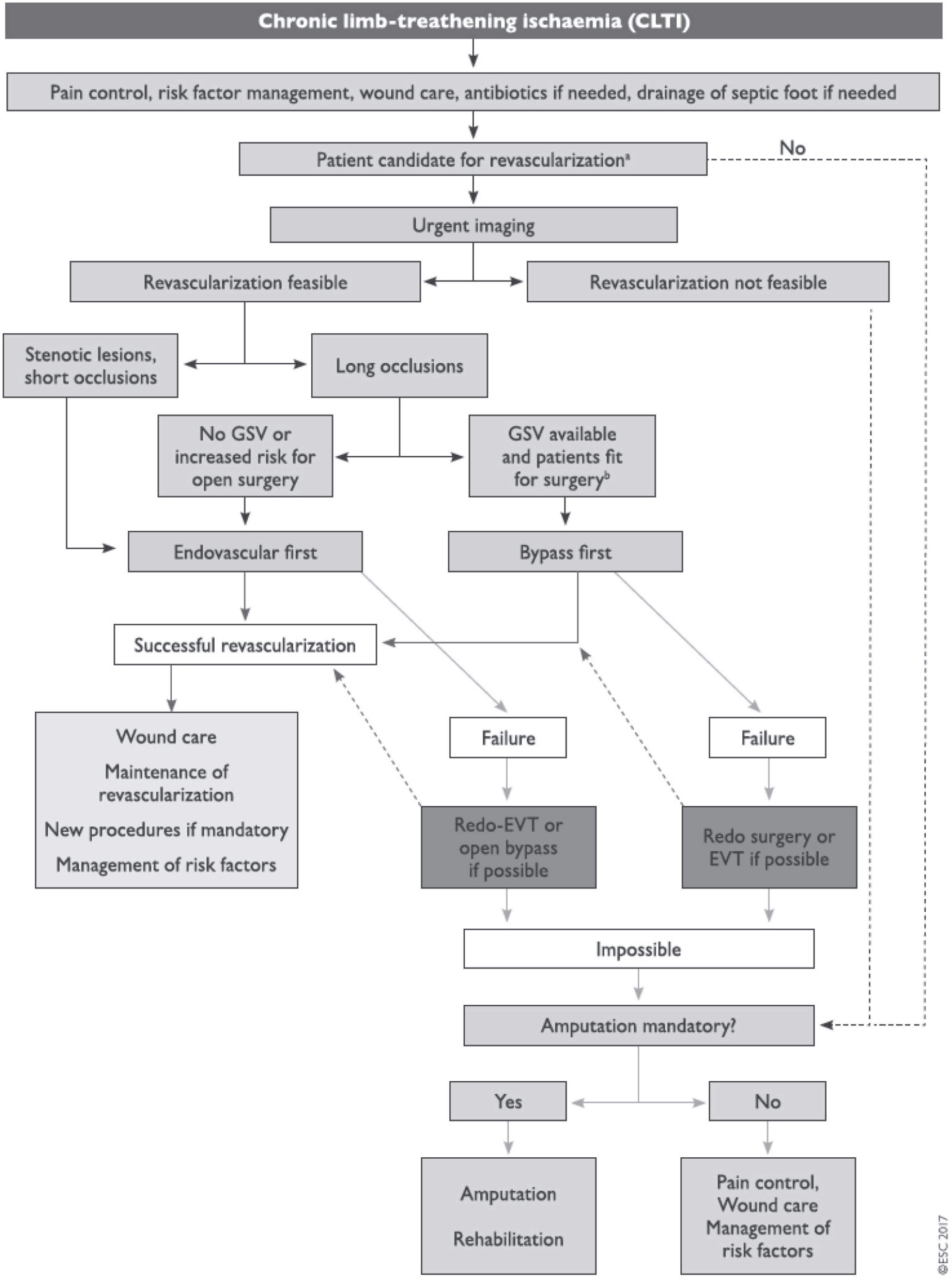
- After diagnosis of peripheral artery disease in diabetic patients, revascularization can be considered in those who are not improved after guideline-directed medical therapy. Recently, more aggressive approaches with interventional treatment have been recommended. Before revascularization therapy, it is important to differentiate patients with claudication or critical limb ischemia, and the final goal and treatment modality of interventional treatments should be based on clinical diagnosis. For patients with claudication, the goal of revascularization is improvement of functional capacity or quality of life; however, in more severe forms of critical limb ischemia, the purpose of revascularization is limb salvage and ultimately saving patient's life. With improvement of vascular interventions, interventional treatment for peripheral artery disease is preferred, although surgical treatment might show better results than intervention in some cases.
MeSH Terms
Figure
Reference
-
1.Writing Committee Members. Gerhard-Herman MD., Gornik HL., Barrett C., Barshes NR., Corriere MA., Drachman DE., Fleisher LA., Fowkes FGR., Hamburg NM., Kinlay S., Lookstein R., Misra S., Mureebe L., Olin JW., Patel RAG., Regensteiner JG., Schanzer A., Shishehbor MH., Stewart KJ., Treat-Jacobson D., Walsh ME. ACC/AHA Task Force Members, Halperin JL, Levine GN, Al-Khatib SM, Birtcher KK, Bozkurt B, Brindis RG, Cigarroa JE, Curtis LH, Fleisher LA, Gentile F, Gidding S, Hlatky MA, Ikonomidis J, Joglar J, Pressler SJ, Wijeysundera DN. 2016 AHA/ACC guideline on the management of patients with lower extremity peripheral artery disease: executive summary. Vasc Med. 2017. 22:NP1–43.
Article2.Aboyans V., Ricco JB., Bartelink MEL., Björck M., Brodmann M., Cohnert T., Collet JP., Czerny M., De Carlo M., Debus S., Espinola-Klein C., Kahan T., Kownator S., Mazzolai L., Naylor AR., Roffi M., Röther J., Sprynger M., Tendera M., Tepe G., Venermo M., Vlachopoulos C., Desormais I. ESC Scientific Document Group. 2017 ESC guidelines on the diagnosis and treatment of peripheral arterial diseases, in collaboration with the European Society for Vascular Surgery (ESVS): document covering atherosclerotic disease of extracranial carotid and vertebral, mesenteric, renal, upper and lower extremity arteriesEndorsed by: the European Stroke Organization (ESO) the task force for the diagnosis and treatment of peripheral arterial diseases of the European Society of Cardiology (ESC) and of the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018. 39:763–816.3.Jelnes R., Gaardsting O., Hougaard Jensen K., Baekgaard N., Tønnesen KH., Schroeder T. Fate in intermittent claudication: outcome and risk factors. Br Med J (Clin Res Ed). 1986. 293:1137–40.
Article4.Leng GC., Lee AJ., Fowkes FG., Whiteman M., Dunbar J., Housley E., Ruckley CV. Incidence, natural history and cardiovascular events in symptomatic and asymptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1996. 25:1172–81.
Article5.TASC Steering Committee. Jaff MR., White CJ., Hiatt WR., Fowkes GR., Dormandy J., Razavi M., Reekers J., Norgren L. An update on methods for revascularization and expansion of the TASC lesion classification to include below-the-knee arteries: a supplement to the inter-society consensus for the management of peripheral arterial disease (TASC II). Vasc Med. 2015. 20:465–78.
Article6.Udoff EJ., Barth KH., Harrington DP., Kaufman SL., White RI. Hemodynamic significance of iliac artery stenosis: pressure measurements during angiography. Radiology. 1979. 132:289–93.
Article7.Tetteroo E., van Engelen AD., Spithoven JH., Tielbeek AV., van der Graaf Y., Mali WP. Stent placement after iliac angioplasty: comparison of hemodynamic and angiographic criteria. Dutch Iliac Stent Trial Study Group. Radiology. 1996. 201:155–9.
Article8.Vemulapalli S., Dolor RJ., Hasselblad V., Subherwal S., Schmit KM., Heidenfelder BL., Patel MR., Schuyler Jones W. Comparative effectiveness of medical therapy, supervised exercise, and revascularization for patients with intermittent claudication: a network meta-analysis. Clin Cardiol. 2015. 38:378–86.
Article9.Murphy TP., Cutlip DE., Regensteiner JG., Mohler ER 3rd., Cohen DJ., Reynolds MR., Massaro JM., Lewis BA., Cerezo J., Oldenburg NC., Thum CC., Jaff MR., Comerota AJ., Steffes MW., Abrahamsen IH., Goldberg S., Hirsch AT. Supervised exercise, stent revascularization, or medical therapy for claudication due to aortoiliac peripheral artery disease: the CLEVER study. J Am Coll Cardiol. 2015. 65:999–1009.10.Murphy TP., Cutlip DE., Regensteiner JG., Mohler ER., Cohen DJ., Reynolds MR., Massaro JM., Lewis BA., Cerezo J., Oldenburg NC., Thum CC., Goldberg S., Jaff MR., Steffes MW., Comerota AJ., Ehrman J., Treat-Jacobson D., Walsh ME., Collins T., Badenhop DT., Bronas U., Hirsch AT. CLEVER Study Investigators. Supervised exercise versus primary stenting for claudication resulting from aortoiliac peripheral artery disease: six-month outcomes from the claudication: exercise versus endoluminal revascularization (CLEVER) study. Circulation. 2012. 125:130–9.11.Nordanstig J., Taft C., Hensäter M., Perlander A., Osterberg K., Jivegård L. Improved quality of life after 1 year with an invasive versus a noninvasive treatment strategy in claudicants: one-year results of the Invasive Revascularization or Not in Intermittent Claudication (IRONIC) Trial. Circulation. 2014. 130:939–47.12.Malgor RD., Alahdab F., Elraiyah TA., Rizvi AZ., Lane MA., Prokop LJ., Phung OJ., Farah W., Montori VM., Conte MS., Murad MH. A systematic review of treatment of intermittent claudication in the lower extremities. J Vasc Surg. 2015. 61:54S–73S.
Article13.Spronk S., Bosch JL., den Hoed PT., Veen HF., Pattynama PM., Hunink MG. Intermittent claudication: clinical effectiveness of endovascular revascularization versus supervised hospital-based exercise training–randomized controlled trial. Radiology. 2009. 250:586–95.
Article14.Greenhalgh RM., Belch JJ., Brown LC., Gaines PA., Gao L., Reise JA., Thompson SG. Mimic Trial Participants. The adjuvant benefit of angioplasty in patients with mild to moderate intermittent claudication (MIMIC) managed by supervised exercise, smoking cessation advice and best medical therapy: results from two randomised trials for stenotic femoropopliteal and aortoiliac arterial disease. Eur J Vasc Endovasc Surg. 2008. 36:680–8.15.Nordanstig J., Gelin J., Hensäter M., Taft C., Österberg K., Jivegård L. Walking performance and health-related quality of life after surgical or endovascular invasive versus non-invasive treatment for intermittent claudication–a prospective randomised trial. Eur J Vasc Endovasc Surg. 2011. 42:220–7.16.Jones WS., Schmit KM., Vemulapalli S., Subherwal S., Patel MR., Hasselblad V., Heidenfelder BL., Chobot MM., Posey R., Wing L., Sanders GD., Dolor RJ. Treatment strategies for patients with peripheral artery disease. Rockville (MD): Agency for Healthcare Research and Quality (US);2013. May. Report No.: 13-EHC090-EF.17.Antoniou GA., Chalmers N., Georgiadis GS., Lazarides MK., Antoniou SA., Serracino-Inglott F., Smyth JV., Murray D. A meta-analysis of endovascular versus surgical reconstruction of femoropopliteal arterial disease. J Vasc Surg. 2013. 57:242–53.
Article18.Fowkes F., Leng GC. Bypass surgery for chronic lower limb ischaemia. Cochrane Database Syst Rev. 2008. 2:CD002000.
Article19.Aihara H., Soga Y., Mii S., Okazaki J., Yamaoka T., Kamoi D., Shintani Y., Ishikawa T. RECANALISE Registry Investigators. Comparison of long-term outcome after endovascular therapy versus bypass surgery in claudication patients with Trans-Atlantic Inter-Society Consensus-II C and D femoropopliteal disease. Circ J. 2014. 78:457–64.
Article20.Sachwani GR., Hans SS., Khoury MD., King TF., Mitsuya M., Rizk YS., Zachwieja JA., Sayed L. Results of iliac stenting and aortofemoral grafting for iliac artery occlusions. J Vasc Surg. 2013. 57:1030–7.
Article21.Siracuse JJ., Gill HL., Schneider DB., Graham AR., Connolly PH., Jones DW., Meltzer AJ. Assessing the perioperative safety of common femoral endarterectomy in the endovascular era. Vasc Endovascular Surg. 2014. 48:27–33.
Article22.Pereira CE., Albers M., Romiti M., Brochado-Neto FC., Pereira CA. Meta-analysis of femoropopliteal bypass grafts for lower extremity arterial insufficiency. J Vasc Surg. 2006. 44:510–7.
Article23.Twine CP., McLain AD. Graft type for femoropopliteal bypass surgery. Cochrane Database Syst Rev. 2010. 5:CD001487.
Article24.Adam DJ., Beard JD., Cleveland T., Bell J., Bradbury AW., Forbes JF., Fowkes FG., Gillepsie I., Ruckley CV., Raab G., Storkey H. BASIL trial participants. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005. 366:1925–34.25.Bradbury AW., Adam DJ., Bell J., Forbes JF., Fowkes FG., Gillespie I., Raab G., Ruckley CV. Multicentre randomised controlled trial of the clinical and cost-effectiveness of a bypass-surgery-first versus a balloon-angioplasty-first revascularisation strategy for severe limb ischaemia due to infrainguinal disease. The Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial. Health Technol Assess. 2010. 14:1–210. iii-iv.
Article26.Menard MT., Farber A. The BEST-CLI trial: a multidisciplinary effort to assess whether surgical or endovascular therapy is better for patients with critical limb ischemia. Semin Vasc Surg. 2014. 27:82–4.
Article27.Menard MT., Farber A., Assmann SF., Choudhry NK., Conte MS., Creager MA., Dake MD., Jaff MR., Kaufman JA., Powell RJ., Reid DM., Siami FS., Sopko G., White CJ., Rosenfield K. Design and rationale of the Best Endovascular Versus Best Surgical Therapy for Patients With Critical Limb Ischemia (BEST-CLI) Trial. J Am Heart Assoc. 2016. 5:e003219.
Article28.Neville RF., Attinger CE., Bulan EJ., Ducic I., Thomassen M., Sidawy AN. Revascularization of a specific angiosome for limb salvage: does the target artery matter? Ann Vasc Surg. 2009. 23:367–73.
Article29.Acín F., Varela C., López de Maturana I., de Haro J., Bleda S., Rodriguez-Padilla J. Results of infrapopliteal endovascular procedures performed in diabetic patients with critical limb ischemia and tissue loss from the perspective of an angiosome-oriented revascularization strategy. Int J Vasc Med. 2014. 2014:270539.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment of Diabetic Foot Disease
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Diagnosis and Management of Diabetic Foot
- Intraoperative Balloon Angioplasty in Diabetic Foot with Peripheral Artery Occlusive Disease During Amputation: Two Case Reports
- Peripheral Arterial Disease