Transl Clin Pharmacol.
2019 Mar;27(1):24-32. 10.12793/tcp.2019.27.1.24.
Characterization of circadian blood pressure patterns using non-linear mixed effects modeling
- Affiliations
-
- 1Department of Pharmacology, Yonsei University College of Medicine, Seoul 03722, Korea. kspark@yuhs.ac
- 2Brain Korea 21 Plus Project for Medical Science, Yonsei University, Seoul 03722, Korea.
- 3Ministry of Food and Drug Safety, Cheongju 28159, Korea.
- KMID: 2442243
- DOI: http://doi.org/10.12793/tcp.2019.27.1.24
Abstract
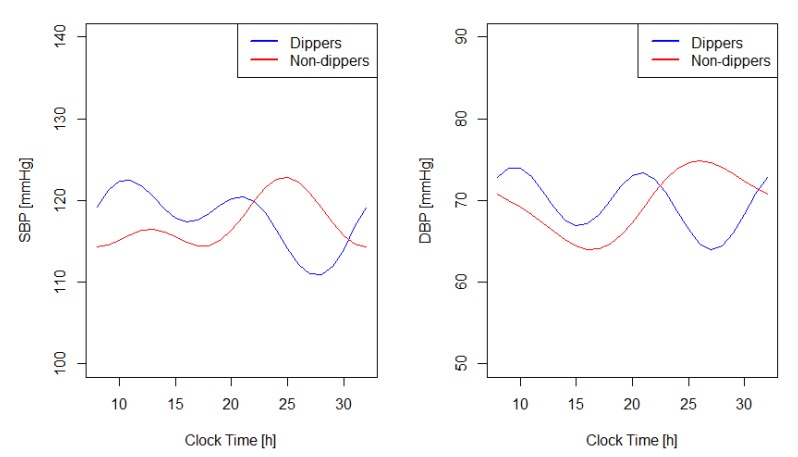
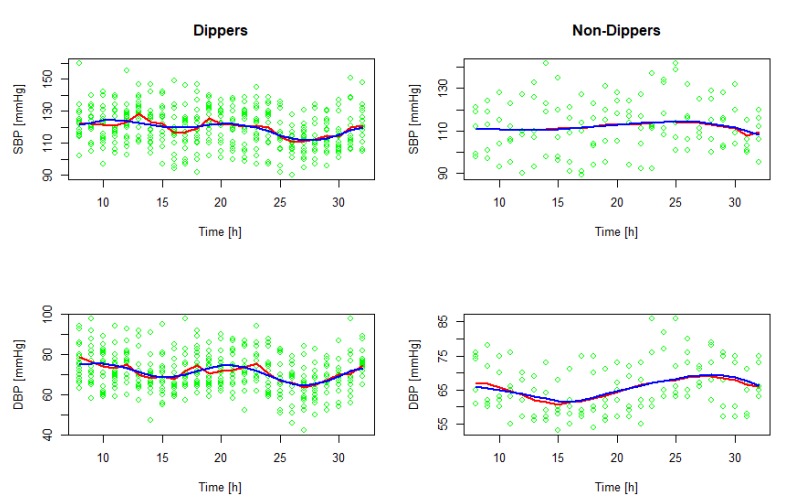
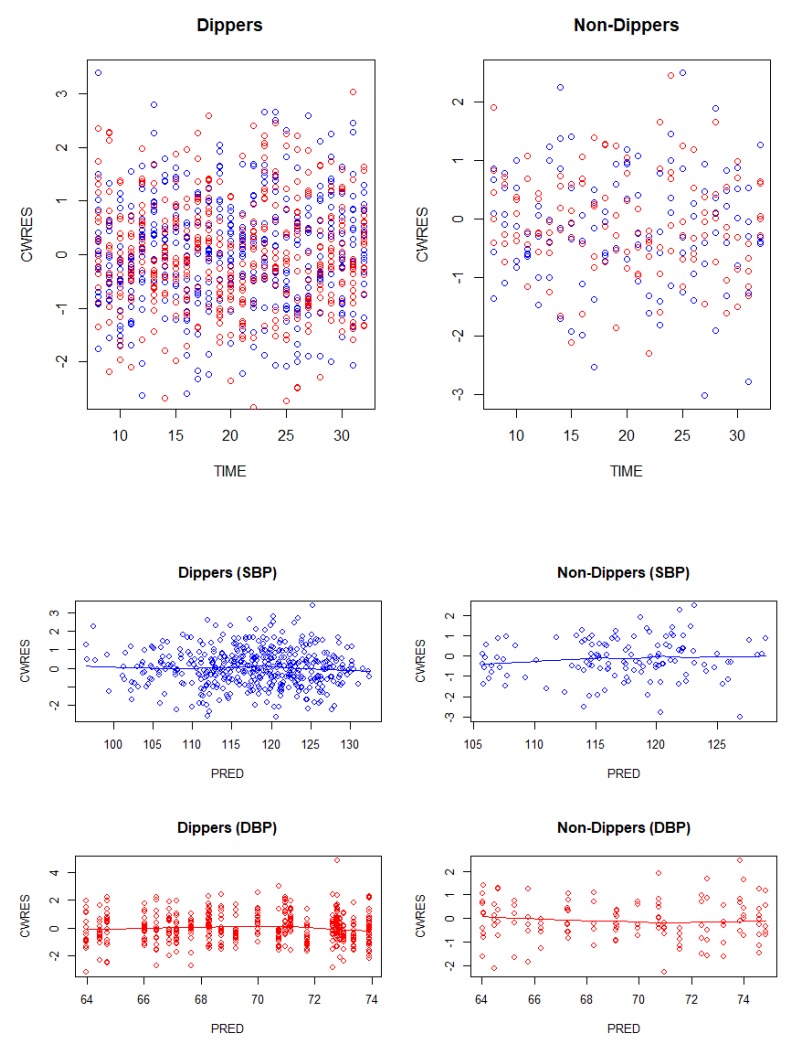
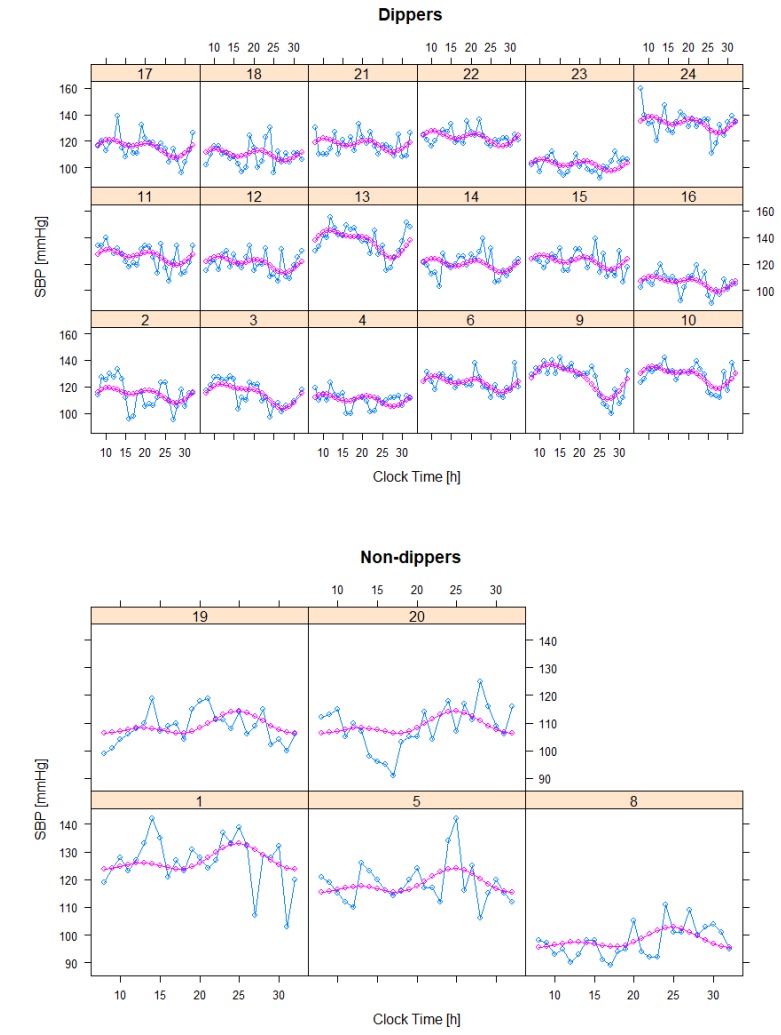
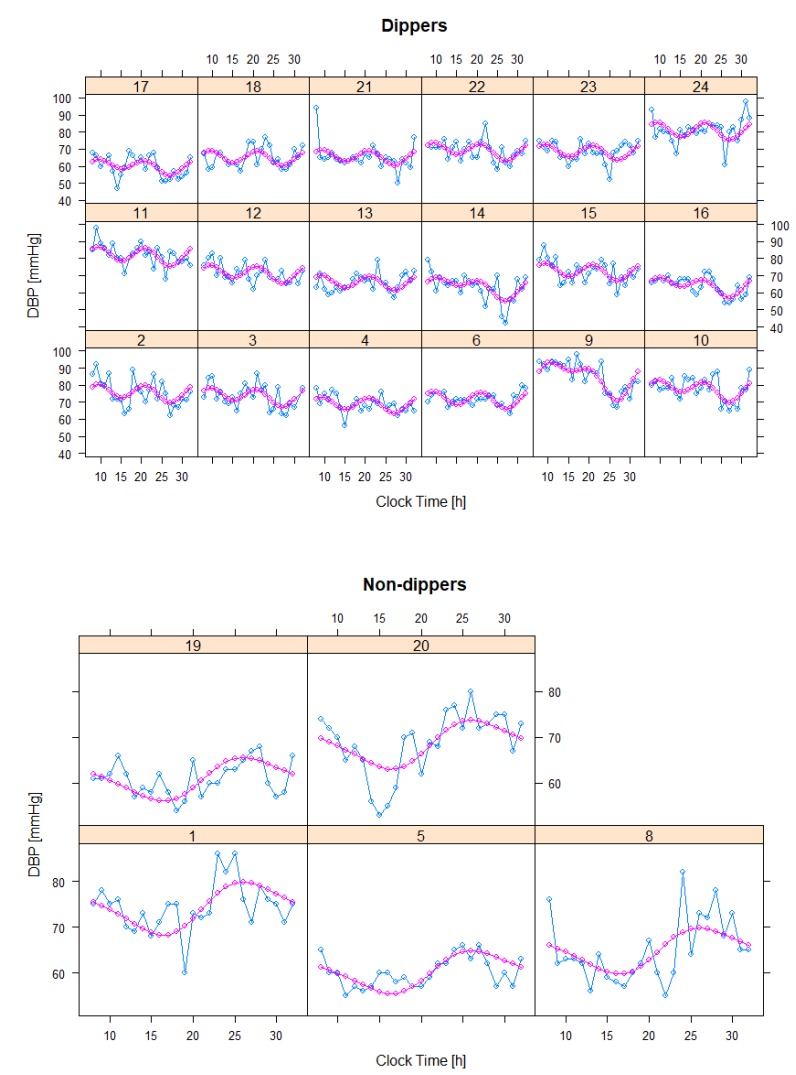
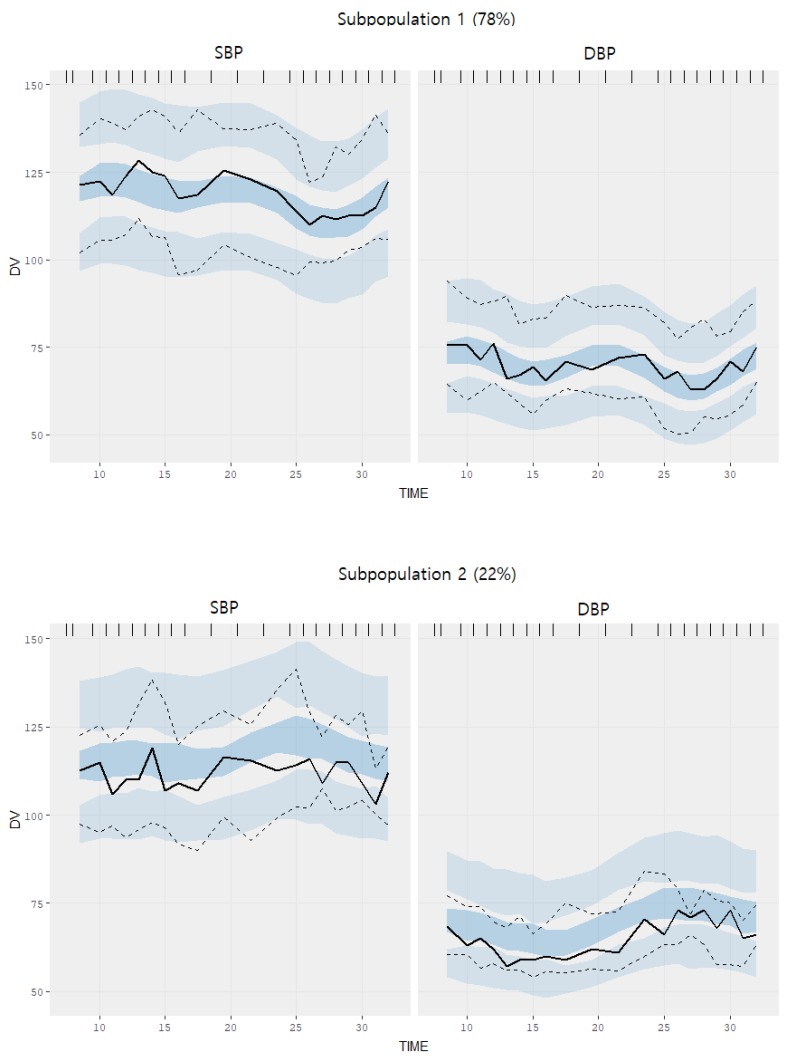
- Characterizing the time course of baseline or pre-drug blood pressure is important in acquiring unbiased estimates of antihypertensive drug effect. In this study, we recruited 23 healthy male volunteers and measured systolic (SBP) and diastolic blood pressure (DBP) over 24 hours on an hourly basis. Using a non-linear mixed effects model, circadian rhythm observed in blood pressure measurements was described by incorporating two cosine functions with periods 24 and 12 hours. A mixture model was applied to identify subgroups exhibiting qualitatively different circadian rhythms. Our results suggested that 78% of the study population, defined as "˜dippers', demonstrated a typical circadian profile with a morning rise and a nocturnal dip. The remaining 22% of the subjects defined as "˜non-dippers', however, were not adequately described using the typical profile and demonstrated an elevation of blood pressure during night-time. Covariate search identified weight as being positively correlated with mesor of SBP. Visual predictive checks using 1,000 simulated datasets were performed for model validation. Observations were in agreement with predicted values in "˜dippers', but deviated slightly in "˜non-dippers'. Our work is expected to serve as a useful reference in assessing systematic intra-day blood pressure fluctuations and antihypertensive effects as well as assessing drug safety of incrementally modified drugs.
Figure
Reference
-
1. Sirgo MA, Mills RJ, DeQuattro V. Effects of antihypertensive agents on circadian blood pressure and heart rate patterns. Review. Arch Intern Med. 1988; 148:2547–2552. PMID: 3058070.
Article2. Degaute JP, van de Borne P, Linkowski P, Van Cauter E. Quantitative analysis of the 24-hour blood pressure and heart rate patterns in young men. Hypertension. 1991; 18:199–210. PMID: 1885228.
Article3. O'Brien E, Sheridan J, O'Malley K. Dippers and non-dippers. Lancet. 1988; 2:397.4. Ohkubo T, Hozawa A, Yamaguchi J, Kikuya M, Ohmori K, Michimata M, et al. Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study. J Hypertens. 2002; 20:2183–2189. PMID: 12409956.5. Metoki H, Ohkubo T, Kikuya M, Asayama K, Obara T, Hashimoto J, et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: the Ohasama study. Hypertension. 2006; 47:149–154. DOI: 10.1161/01.HYP.0000198541.12640.0f. PMID: 16380533.6. Che X, Mou S, Zhang W, Zhang M, Gu L, Yan Y, et al. The impact of non-dipper circadian rhythm of blood pressure on left ventricular hypertrophy in patients with non-dialysis chronic kidney disease. Acta Cardiol. 2017; 72:149–155. DOI: 10.1080/00015385.2017.1291133. PMID: 28597784.
Article7. Baumgart P. Circadian rhythm of blood pressure: internal and external time triggers. Chronobiol Int. 1991; 8:444–450. PMID: 1799926.
Article8. Tanigawara Y, Yoshihara K, Kuramoto K, Arakawa K. Comparative pharmacodynamics of olmesartan and azelnidipine in patients with hypertension: a population pharmacokinetic/pharmacodynamic analysis. Drug Metab Pharmacokinet. 2009; 24:376–388. PMID: 19745564.
Article9. Chae D, Son M, Kim Y, Son H, Park K. Mechanistic model for blood pressure and heart rate changes produced by telmisartan in human beings. Basic Clin Pharmacol Toxicol. 2018; 122:139–148. DOI: 10.1111/bcpt.12856. PMID: 28805311.
Article10. Staessen J, Celis H, De Cort P, Fagard R, Thijs L, Amery A. Methods for describing the diurnal blood pressure curve. J Hypertens Suppl. 1991; 9:S16–S18. PMID: 1795193.11. Hempel G, Karlsson MO, de Alwis DP, Toublanc N, McNay J, Schaefer HG. Population pharmacokinetic-pharmacodynamic modeling of moxonidine using 24-hour ambulatory blood pressure measurements. Clin Pharmacol Ther. 1998; 64:622–635. DOI: 10.1016/S0009-9236(98)90053-4. PMID: 9871427.
Article12. van Rijn-Bikker PC, Snelder N, Ackaert O, van Hest RM, Ploeger BA, van Montfrans GA, et al. Nonlinear mixed effects modeling of the diurnal blood pressure profile in a multiracial population. Am J Hypertens. 2013; 26:1103–1113. DOI: 10.1093/ajh/hpt088. PMID: 23939415.
Article13. Sällström B, Visser SA, Forsberg T, Peletier LA, Ericson AC, Gabrielsson J. A pharmacodynamic turnover model capturing asymmetric circadian baselines of body temperature, heart rate and blood pressure in rats: challenges in terms of tolerance and animal-handling effects. J Pharmacokinet Pharmacodyn. 2005; 32:835–859. DOI: 10.1007/s10928-005-0087-2. PMID: 16328099.
Article14. Millar Craig MW, Mann S, Balasubramanian V, Raftery EB. Blood pressure circadian rhythm in essential hypertension. Clin Sci Mol Med Suppl. 1978; 4:391s–393s. PMID: 282095.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circadian Biorhythmicity in Normal Pressure Hydrocephalus - A Case Series Report
- Blood Pressure Variation and Cardiovascular Risks
- The Relation of Epicardial Fat Thickness, Neutrophil to Lymphocyte Ratio and Circadian Rhythm of Blood Pressure
- Decreased potency of fimasartan in liver cirrhosis was quantified using mixed-effects analysis
- The Circadian Rhythms of Blood Pressure and Heart Rate in the Hypertensive Subjects: Dippers and Non-Dippers