Korean J Radiol.
2019 Apr;20(4):589-598. 10.3348/kjr.2018.0306.
Prediction of Treatment Outcome of Chemotherapy Using Perfusion Computed Tomography in Patients with Unresectable Advanced Gastric Cancer
- Affiliations
-
- 1Department of Radiology, Seoul National University Hospital, Seoul, Korea. shkim7071@gmail.com
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Hallym University Sacred Heart Hospital, Seoul, Korea.
- 4Institute of Radiation Medicine, Seoul National University Medical Research Center, Seoul, Korea.
- KMID: 2440482
- DOI: http://doi.org/10.3348/kjr.2018.0306
Abstract
OBJECTIVE
To evaluate whether data acquired from perfusion computed tomography (PCT) parameters can aid in the prediction of treatment outcome after palliative chemotherapy in patients with unresectable advanced gastric cancer (AGC).
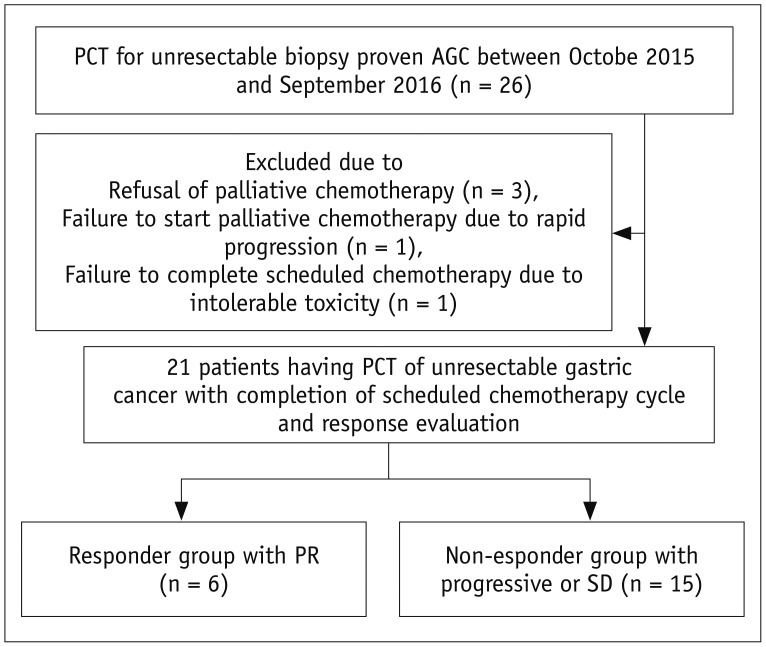
MATERIALS AND METHODS
Twenty-one patients with unresectable AGCs, who underwent both PCT and palliative chemotherapy, were prospectively included. Treatment response was assessed according to Response Evaluation Criteria in Solid Tumors version 1.1 (i.e., patients who achieved complete or partial response were classified as responders). The relationship between tumor response and PCT parameters was evaluated using the Mann-Whitney test and receiver operating characteristic analysis. One-year survival was estimated using the Kaplan-Meier method.
RESULTS
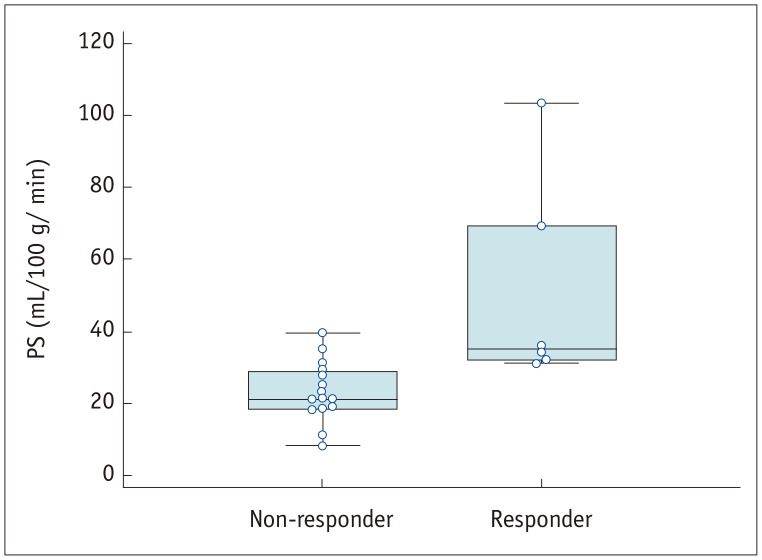
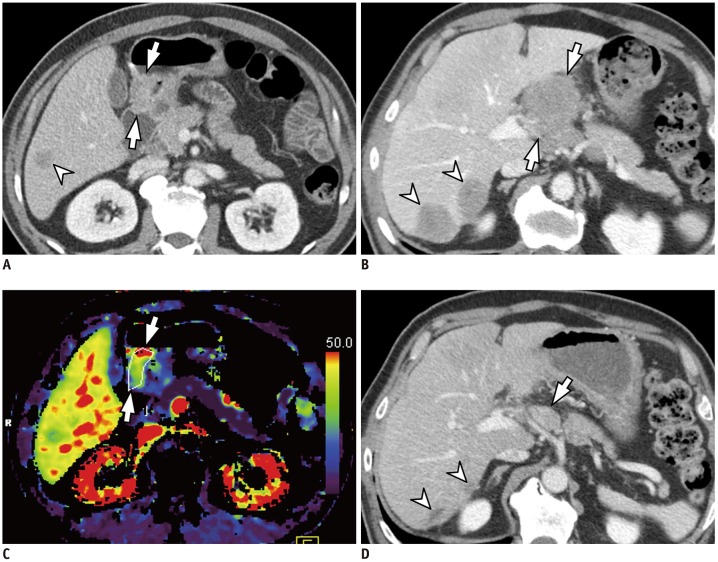
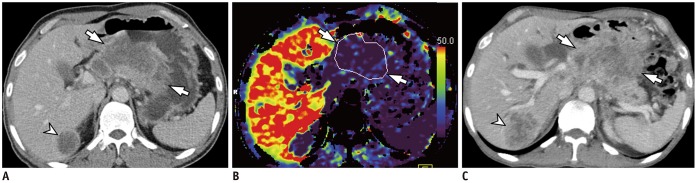
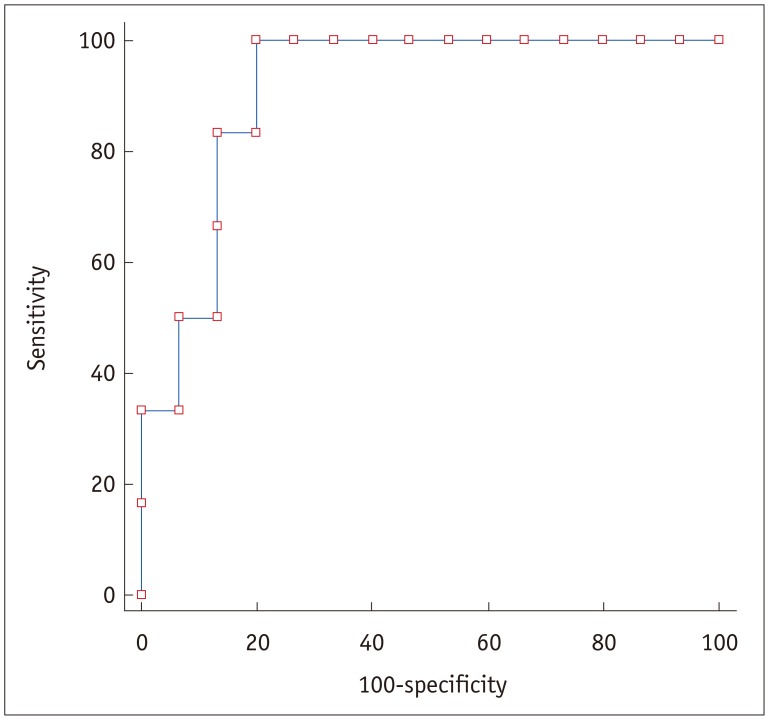
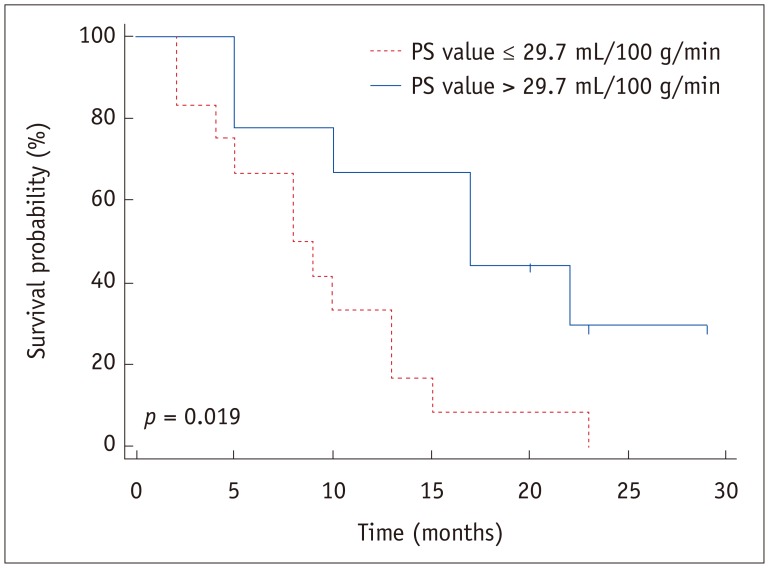
After chemotherapy, six patients exhibited partial response and were allocated to the responder group while the remaining 15 patients were allocated to the non-responder group. Permeability surface (PS) value was shown to be significantly different between the responder and non-responder groups (51.0 mL/100 g/min vs. 23.4 mL/100 g/min, respectively; p = 0.002), whereas other PCT parameters did not demonstrate a significant difference. The area under the curve for prediction in responders was 0.911 (p = 0.004) for PS value, with a sensitivity of 100% (6/6) and specificity of 80% (12/15) at a cut-off value of 29.7 mL/100 g/min. One-year survival in nine patients with PS value > 29.7 mL/100 g/min was 66.7%, which was significantly higher than that in the 12 patients (33.3%) with PS value ≤ 29.7 mL/100 g/min (p = 0.019).
CONCLUSION
Perfusion parameter data acquired from PCT demonstrated predictive value for treatment outcome after palliative chemotherapy, reflected by the significantly higher PS value in the responder group compared with the non-responder group.
Keyword
MeSH Terms
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74–108. PMID: 15761078.
Article2. Soerjomataram I, Lortet-Tieulent J, Parkin DM, Ferlay J, Mathers C, Forman D, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet. 2012; 380:1840–1850. PMID: 23079588.
Article3. Lee DH, Kim SH, Joo I, Hur BY, Han JK. Comparison between 18F-FDG PET/MRI and MDCT for the assessment of preoperative staging and resectability of gastric cancer. Eur J Radiol. 2016; 85:1085–1091. PMID: 27161056.
Article4. Glimelius B, Ekström K, Hoffman K, Graf W, Sjödén PO, Haglund U, et al. Randomized comparison between chemotherapy plus best supportive care with best supportive care in advanced gastric cancer. Ann Oncol. 1997; 8:163–168.
Article5. Wöhrer SS, Raderer M, Hejna M. Palliative chemotherapy for advanced gastric cancer. Ann Oncol. 2004; 15:1585–1595. PMID: 15520058.
Article6. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009; 45:228–224. PMID: 19097774.
Article7. Koh TS, Thng CH, Lee PS, Hartono S, Rumpel H, Goh BC, et al. Hepatic metastases: in vivo assessment of perfusion parameters at dynamic contrast-enhanced MR imaging with dual-input two-compartment tracer kinetics model. Radiology. 2008; 249:307–320. PMID: 18695207.
Article8. Harry VN, Semple SI, Parkin DE, Gilbert FJ. Use of new imaging techniques to predict tumour response to therapy. Lancet Oncol. 2010; 11:92–102. PMID: 20129132.
Article9. Chung HH, Kim JW, Han KH, Eo JS, Kang KW, Park NH, et al. Prognostic value of metabolic tumor volume measured by FDG-PET/CT in patients with cervical cancer. Gynecol Oncol. 2011; 120:270–274. PMID: 21109300.
Article10. Kim JW, Jeong YY, Chang NK, Heo SH, Shin SS, Lee JH, et al. Perfusion CT in colorectal cancer: comparison of perfusion parameters with tumor grade and microvessel density. Korean J Radiol. 2012; 13:S89–S97. PMID: 22563293.
Article11. Lv WF, Han JK, Cheng DL, Zhou CZ, Ni M, Lu D. CT perfusion imaging can predict patients' survival and early response to transarterial chemo-lipiodol infusion for liver metastases from colorectal cancers. Korean J Radiol. 2015; 16:810–820. PMID: 26175580.
Article12. Lee DH, Kim SH, Im SA, Oh DY, Kim TY, Han JK. Multiparametric fully-integrated 18-FDG PET/MRI of advanced gastric cancer for prediction of chemotherapy response: a preliminary study. Eur Radiol. 2016; 26:2771–2778. PMID: 26615555.
Article13. Miles KA, Griffiths MR. Perfusion CT: a worthwhile enhancement? Br J Radiol. 2003; 76:220–231. PMID: 12711641.
Article14. Yi CA, Lee KS, Kim EA, Han J, Kim H, Kwon OJ, et al. Solitary pulmonary nodules: dynamic enhanced multi-detector row CT study and comparison with vascular endothelial growth factor and microvessel density. Radiology. 2004; 233:191–199. PMID: 15304661.
Article15. Meijerink MR, van Waesberghe JH, van der Weide L, van den Tol P, Meijer S, van Kuijk C. Total-liver-volume perfusion CT using 3-D image fusion to improve detection and characterization of liver metastases. Eur Radiol. 2008; 2345–2354. PMID: 18491094.
Article16. Chen TW, Yang ZG, Li Y, Li ZL, Yao J, Sun JY. Quantitative assessment of first-pass perfusion of oesophageal squamous cell carcinoma using 64-section MDCT: initial observation. Clin Radiol. 2009; 64:38–45. PMID: 19070696.
Article17. Zhang H, Pan Z, Du L, Yan C, Ding B, Song Q, et al. Advanced gastric cancer and perfusion imaging using a multidetector row computed tomography: correlation with prognostic determinants. Korean J Radiol. 2008; 9:119–127. PMID: 18385558.
Article18. Satoh A, Shuto K, Okazumi S, Ohira G, Natsume T, Hayano K, et al. Role of perfusion CT in assessing tumor blood flow and malignancy level of gastric cancer. Dig Surg. 2010; 27:253–260. PMID: 20668380.
Article19. Yao J, Yang ZG, Chen TW, Li Y, Yang L. Perfusion changes in gastric adenocarcinoma: evaluation with 64-section MDCT. Abdom Imaging. 2010; 35:195–202. PMID: 19259725.
Article20. Yao J, Yang ZG, Chen HJ, Chen TW, Huang J. Gastric adenocarcinoma: can perfusion CT help to noninvasively evaluate tumor angiogenesis? Abdom Imaging. 2011; 36:15–21. PMID: 20336293.
Article21. Lee DH, Kim SH, Joo I, Han JK. CT Perfusion evaluation of gastric cancer: correlation with histologic type. Eur Radiol. 2018; 28:487–495. PMID: 28779403.
Article22. Kruk-Bachonko J, Krupski W, Czechowski M, Kurys-Denis E, Mądro P, Sierocińska-Sawa J, et al. Perfusion CT - A novel quantitative and qualitative imaging biomarker in gastric cancer. Eur J Radiol. 2017; 95:399–408. PMID: 28987697.
Article23. Shin CI, Kim SH, Lee ES, Lee DH, Hwang EJ, Chung SY, et al. Ultra-low peak voltage CT colonography: effect of iterative reconstruction algorithms on performance of radiologists who use anthropomorphic colonic phantoms. Radiology. 2014; 273:759–771. PMID: 25010640.
Article24. Lundsgaard Hansen M, Fallentin E, Lauridsen C, Law I, Federspiel B, Bæksgaard L, et al. Computed tomography (CT) perfusion as an early predictive marker for treatment response to neoadjuvant chemotherapy in gastroesophageal junction cancer and gastric cancer--a prospective study. PLoS One. 2014; 9:e97605. PMID: 24845062.25. Brix G, Bahner ML, Hoffmann U, Horvath A, Schreiber W. Regional blood flow, capillary permeability, and compartmental volumes: measurement with dynamic CT--initial experience. Radiology. 1999; 210:269–276. PMID: 9885619.
Article26. Raghunand N, Gatenby RA, Gillies RJ. Microenvironmental and cellular consequences of altered blood flow in tumours. Br J Radiol. 2003; 76:S11–S22. PMID: 15456710.
Article27. Bellomi M, Petralia G, Sonzogni A, Zampino MG, Rocca A. CT perfusion for the monitoring of neoadjuvant chemotherapy and radiation therapy in rectal carcinoma: initial experience. Radiology. 2007; 244:486–493. PMID: 17641369.
Article28. Cooper RA, Carrington BM, Loncaster JA, Todd SM, Davidson SE, Logue JP, et al. Tumour oxygenation levels correlate with dynamic contrast-enhanced magnetic resonance imaging parameters in carcinoma of the cervix. Radiother Oncol. 2000; 57:53–59. PMID: 11033189.
Article29. Lim JS, Kim D, Baek SE, Myoung S, Choi J, Shin SJ, et al. Perfusion MRI for the prediction of treatment response after preoperative chemoradiotherapy in locally advanced rectal cancer. Eur Radiol. 2012; 22:1693–1700. PMID: 22427184.
Article30. Goh V, Halligan S, Bartram CI. Quantitative tumor perfusion assessment with multidetector CT: are measurements from two commercial software packages interchangeable? Radiology. 2007; 242:777–782. PMID: 17325066.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chemotherapy for Metastatic Gastric Cancer
- Locally advanced unresectable gastric cancer successfully resected after neoadjuvant chemotherapy with FADE regimen
- Determination of resectability of advanced gastric cancer on U.G.I. series
- Preoperative Chemotherapy in Gastric Cancer
- Neoadjuvant Chemotherapy in Asian Patients With Locally Advanced Gastric Cancer