Obstet Gynecol Sci.
2018 Jul;61(4):524-528. 10.5468/ogs.2018.61.4.524.
Primary malignant melanoma of the uterine cervix treated with pembrolizumab after radical surgery: a case report and literature review
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. bksong.kim@samsung.com
- 2Division of Hematology-Oncology, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2439727
- DOI: http://doi.org/10.5468/ogs.2018.61.4.524
Abstract
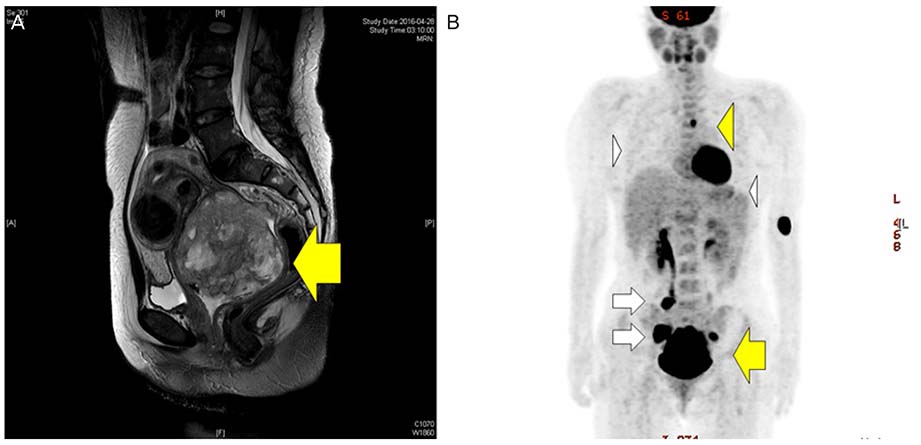
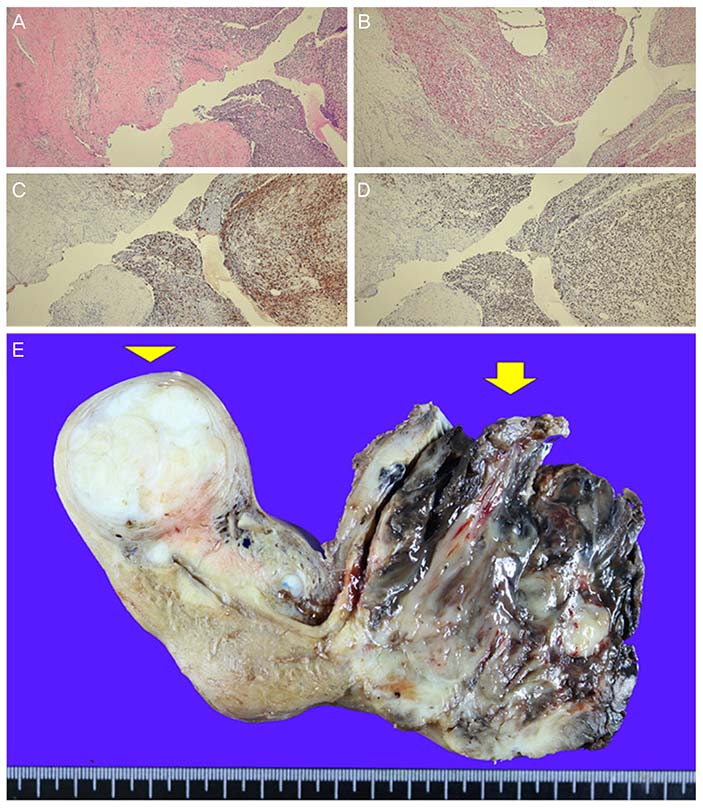
- Malignant melanoma of the genital tract is a rare disease that is usually diagnosed by chance. When a definite diagnosis is delayed, the prognosis is very poor without standardized treatment. Herein, we describe a 40-year-old patient who presented with a history of bloody vaginal discharge for 7 months. Gynecological examination showed an exophytic, hard and pigmented cervical mass involving the upper vagina. The patient was diagnosed with cervical melanoma after a punch biopsy and underwent a radical hysterectomy, upper vaginectomy, bilateral salpingo-oophorectomy and pelvic lymphadenectomy. After surgeries, the patient underwent 2-cycles of adjuvant immunotherapy with pembrolizumab, but died within 8 months. In this report, treatment with pembrolizumab after radical surgery was not effective for this patient who had a primary cervical melanoma that metastasized to bone and lung tissue. We do not know why pembrolizumab was ineffective for this patient, but there are several possible explanations; further research is needed.
MeSH Terms
Figure
Reference
-
1. Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol. 2007; 56:828–834.
Article2. Myriokefalitaki E, Babbel B, Smith M, Ahmed AS. Primary malignant melanoma of uterine cervix FIGO IIa1: a case report with 40 months ongoing survival and literature review. Gynecol Oncol Case Rep. 2013; 5:52–54.3. Cid JM. Melanoid pigmentation of the endocervix: a neurogenic visceral argument. Ann Anat Pathol (Paris). 1959; 4:617–628.4. Mordel N, Mor-Yosef S, Ben-Baruch N, Anteby SO. Malignant melanoma of the uterine cervix: case report and review of the literature. Gynecol Oncol. 1989; 32:375–380.
Article5. Garbe C, Peris K, Hauschild A, Saiag P, Middleton M, Bastholt L, et al. Diagnosis and treatment of melanoma. European consensus-based interdisciplinary guideline - Update 2016. Eur J Cancer. 2016; 63:201–217.
Article6. van Zeijl MC, van den Eertwegh AJ, Haanen JB, Wouters MW. (Neo)adjuvant systemic therapy for melanoma. Eur J Surg Oncol. 2017; 43:534–543.
Article7. Colombino M, Capone M, Lissia A, Cossu A, Rubino C, De Giorgi V, et al. BRAF/NRAS mutation frequencies among primary tumors and metastases in patients with melanoma. J Clin Oncol. 2012; 30:2522–2529.
Article8. Zak KM, Kitel R, Przetocka S, Golik P, Guzik K, Musielak B, et al. Structure of the complex of human programmed death 1, PD-1, and its ligand PD-L1. Structure. 2015; 23:2341–2348.
Article9. Robert C, Ribas A, Wolchok JD, Hodi FS, Hamid O, Kefford R, et al. Anti-programmed-death-receptor-1 treatment with pembrolizumab in ipilimumab-refractory advanced melanoma: a randomised dose-comparison cohort of a phase 1 trial. Lancet. 2014; 384:1109–1117.
Article10. Ribas A, Hamid O, Daud A, Hodi FS, Wolchok JD, Kefford R, et al. Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA. 2016; 315:1600–1609.
Article11. Ribas A, Puzanov I, Dummer R, Schadendorf D, Hamid O, Robert C, et al. Pembrolizumab versus investigator-choice chemotherapy for ipilimumab-refractory melanoma (KEYNOTE-002): a randomised, controlled, phase 2 trial. Lancet Oncol. 2015; 16:908–918.12. Robert C, Schachter J, Long GV, Arance A, Grob JJ, Mortier L, et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med. 2015; 372:2521–2532.
Article13. Gadiot J, Hooijkaas AI, Kaiser AD, van Tinteren H, van Boven H, Blank C. Overall survival and PD-L1 expression in metastasized malignant melanoma. Cancer. 2011; 117:2192–2201.
Article14. Hino R, Kabashima K, Kato Y, Yagi H, Nakamura M, Honjo T, et al. Tumor cell expression of programmed cell death-1 ligand 1 is a prognostic factor for malignant melanoma. Cancer. 2010; 116:1757–1766.
Article15. Yuan G, Wu L, Li B, An J. Primary malignant melanoma of the cervix: report of 14 cases and review of literature. Oncotarget. 2017; 8:73162–73167.
Article16. Teixeira JC, Salina JR, Teixeira LC, Andrade LA. Primary melanoma of the uterine cervix FIGO stage III B. Sao Paulo Med J. 1998; 116:1778–1780.
Article17. Cantuaria G, Angioli R, Nahmias J, Estape R, Penalver M. Primary malignant melanoma of the uterine cervix: case report and review of the literature. Gynecol Oncol. 1999; 75:170–174.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case report of Primary Malignant Melanoma of the Uterine Cervix
- A Case of Primary Malignant Melanoma of Uterine Cervix
- Primary amelanotic melanoma of the cervix: case report with review of literature
- Primary malignant melanoma of the uterine cervix: A case report
- A Case of Primary Malignant Melanoma of the Vagina: Vulvovaginal Reconstruction Using Gracilis My ocutaneous Flap Afer Radical Surgery