J Korean Med Sci.
2017 Aug;32(8):1275-1280. 10.3346/jkms.2017.32.8.1275.
Uric Acid Level Has a U-shaped Association with Clinical Outcomes in Patients with Vasospastic Angina
- Affiliations
-
- 1Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. cardiochoi@skku.edu
- 2Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2439461
- DOI: http://doi.org/10.3346/jkms.2017.32.8.1275
Abstract
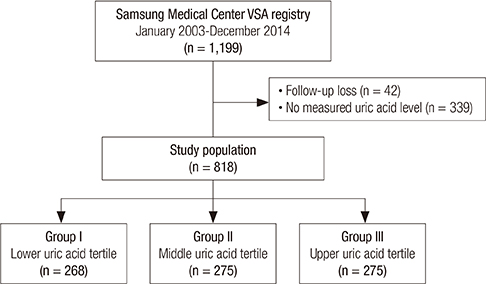
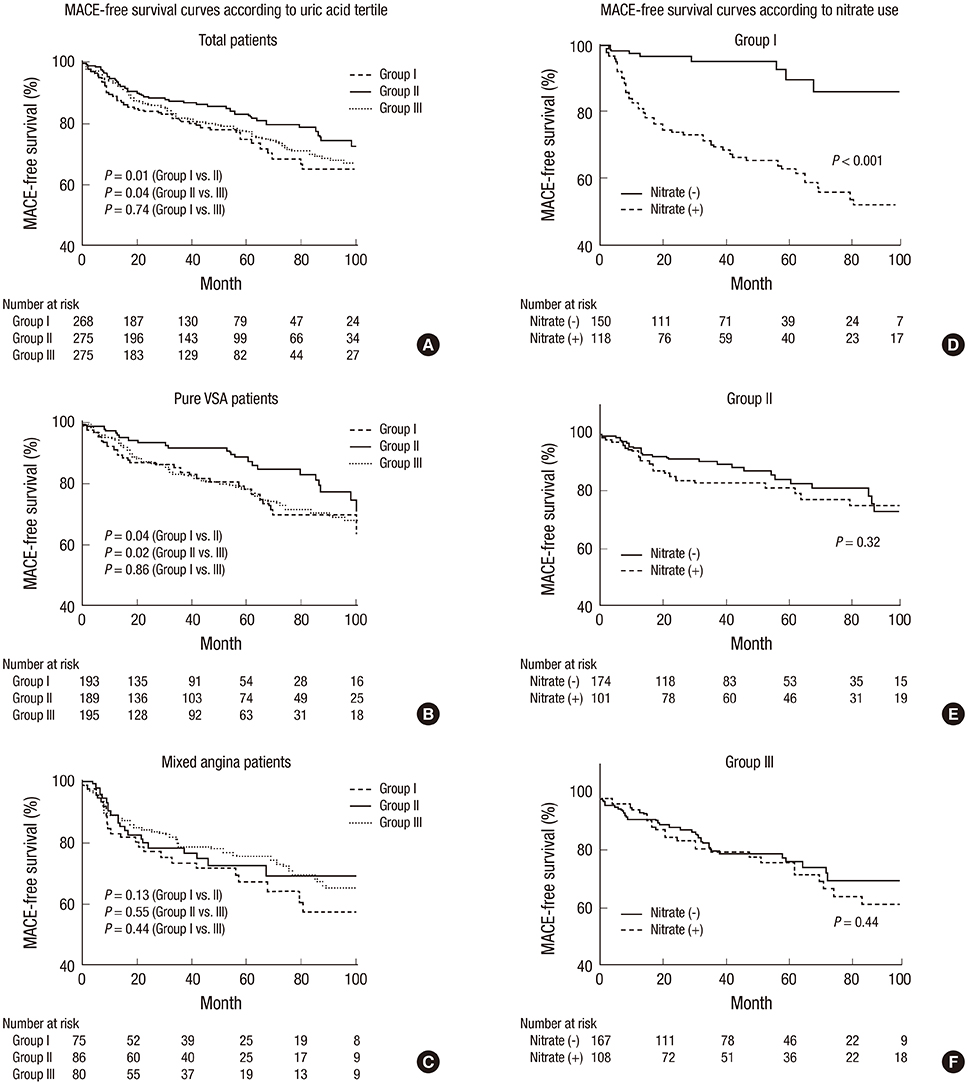
- No data are available on the association of serum uric acid and vasospastic angina (VSA) which has endothelial dysfunction as a possible pathophysiologic mechanism. Low uric acid level might cause adverse outcomes in VSA in connection with endothelial dysfunction. We enrolled 818 VSA patients whose uric acid level was measured at admission. Patients were categorized according to tertiles of uric acid level: group I, ≤ 4.8 mg/dL; group II, 4.9-5.9 mg/dL; and group III, ≥ 6.0 mg/dL. Primary outcome was major adverse cardiac events (MACEs), defined as a composite of cardiac death, acute myocardial infarction (MI), ischemic stroke, coronary revascularization, and rehospitalization for angina. Median follow-up duration was 49.2 months. Median uric acid values were 4.1 mg/dL for group I, 5.4 mg/dL for group II, and 6.7 mg/dL for group III. In the overall population, group II had a significantly lower incidence of MACE compared to group I (47 [17.1%] vs. 66 [24.6%]; hazard ratio [HR], 1.52; 95% confidence interval [CI], 1.02-2.26; P = 0.040) and a tendency of lower incidence of MACEs compared to Group III (47 [17.1%] vs. 62 [22.5%]; HR, 1.44; 95% CI, 0.98-2.13; P = 0.067). Among group I patients, those who received nitrates had a higher incidence of MACEs than those without nitrate therapy (P < 0.001). Low uric acid level was associated with adverse clinical outcomes, while high uric acid level had a trend toward an increase in it. Use of nitrate in patients with low uric acid level might have adverse effects on clinical outcomes of VSA.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Hyperuricemia is Associated With an Increased Prevalence of Metabolic Syndrome in a General Population and a Decreased Prevalence of Diabetes in Men
Hyemin Jeong, Ji Eun Moon, Chan Hong Jeon
J Rheum Dis. 2020;27(4):247-260. doi: 10.4078/jrd.2020.27.4.247.Letter to the Editor: When Claiming a U-shaped Association between Uric Acid Levels and Major Adverse Cardiac Events, Perhaps Show the Evidence?
Ivo Abraham
J Korean Med Sci. 2018;33(6):. doi: 10.3346/jkms.2018.33.e50.Reliability and Quality of Korean YouTube Videos for Education Regarding Gout
Bon San Koo, Dam Kim, Jae-Bum Jun
J Korean Med Sci. 2021;36(45):e303. doi: 10.3346/jkms.2021.36.e303.
Reference
-
1. Palmer TM, Nordestgaard BG, Benn M, Tybjærg-Hansen A, Davey Smith G, Lawlor DA, Timpson NJ. Association of plasma uric acid with ischaemic heart disease and blood pressure: mendelian randomisation analysis of two large cohorts. BMJ. 2013; 347:f4262.2. Kanbay M, Segal M, Afsar B, Kang DH, Rodriguez-Iturbe B, Johnson RJ. The role of uric acid in the pathogenesis of human cardiovascular disease. Heart. 2013; 99:759–766.3. Brodov Y, Behar S, Boyko V, Chouraqui P. Effect of the metabolic syndrome and hyperuricemia on outcome in patients with coronary artery disease (from the Bezafibrate Infarction Prevention Study). Am J Cardiol. 2010; 106:1717–1720.4. Iso T, Kurabayashi M. Extremely low levels of serum uric acid are associated with endothelial dysfunction in humans. Circ J. 2015; 79:978–980.5. Nieto FJ, Iribarren C, Gross MD, Comstock GW, Cutler RG. Uric acid and serum antioxidant capacity: a reaction to atherosclerosis? Atherosclerosis. 2000; 148:131–139.6. Morelli M, Carta AR, Kachroo A, Schwarzschild MA. Pathophysiological roles for purines: adenosine, caffeine and urate. Prog Brain Res. 2010; 183:183–208.7. Sugihara S, Hisatome I, Kuwabara M, Niwa K, Maharani N, Kato M, Ogino K, Hamada T, Ninomiya H, Higashi Y, et al. Depletion of uric acid due to SLC22A12 (URAT1) loss-of-function mutation causes endothelial dysfunction in hypouricemia. Circ J. 2015; 79:1125–1132.8. Kaneda H, Taguchi J, Kuwada Y, Hangaishi M, Aizawa T, Yamakado M, Ogasawara K, Aizawa T, Ohno M. Coronary artery spasm and the polymorphisms of the endothelial nitric oxide synthase gene. Circ J. 2006; 70:409–413.9. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17.10. Stern S, Bayes de Luna A. Coronary artery spasm: a 2009 update. Circulation. 2009; 119:2531–2534.11. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010; 74:1745–1762.12. Yoo SY, Shin DH, Jeong JI, Yoon J, Ha DC, Cho SW, Cheong SS. Long-term prognosis and clinical characteristics of patients with variant angina. Korean Circ J. 2008; 38:651–658.13. Culleton BF, Larson MG, Kannel WB, Levy D. Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med. 1999; 131:7–13.14. De Luca G, Secco GG, Santagostino M, Venegoni L, Iorio S, Cassetti E, Verdoia M, Coppo L, Di Mario C, Bellomo G, et al. Uric acid does not affect the prevalence and extent of coronary artery disease. Results from a prospective study. Nutr Metab Cardiovasc Dis. 2012; 22:426–433.15. Yu MA, Sánchez-Lozada LG, Johnson RJ, Kang DH. Oxidative stress with an activation of the renin-angiotensin system in human vascular endothelial cells as a novel mechanism of uric acid-induced endothelial dysfunction. J Hypertens. 2010; 28:1234–1242.16. Waring WS, Webb DJ, Maxwell SR. Systemic uric acid administration increases serum antioxidant capacity in healthy volunteers. J Cardiovasc Pharmacol. 2001; 38:365–371.17. Waring WS, McKnight JA, Webb DJ, Maxwell SR. Uric acid restores endothelial function in patients with type 1 diabetes and regular smokers. Diabetes. 2006; 55:3127–3132.18. Pitocco D, Di Stasio E, Romitelli F, Zaccardi F, Tavazzi B, Manto A, Caputo S, Musella T, Zuppi C, Santini SA, et al. Hypouricemia linked to an overproduction of nitric oxide is an early marker of oxidative stress in female subjects with type 1 diabetes. Diabetes Metab Res Rev. 2008; 24:318–323.19. Antón FM, García Puig J, Ramos T, González P, Ordás J. Sex differences in uric acid metabolism in adults: evidence for a lack of influence of estradiol-17 beta (E2) on the renal handling of urate. Metabolism. 1986; 35:343–348.20. Döring A, Gieger C, Mehta D, Gohlke H, Prokisch H, Coassin S, Fischer G, Henke K, Klopp N, Kronenberg F, et al. SLC2A9 influences uric acid concentrations with pronounced sex-specific effects. Nat Genet. 2008; 40:430–436.21. Lim JH, Kim YK, Kim YS, Na SH, Rhee MY, Lee MM. Relationship between serum uric acid levels, metabolic syndrome, and arterial stiffness in Korean. Korean Circ J. 2010; 40:314–320.22. Akpek M, Kaya MG, Uyarel H, Yarlioglues M, Kalay N, Gunebakmaz O, Dogdu O, Ardic I, Elcik D, Sahin O, et al. The association of serum uric acid levels on coronary flow in patients with STEMI undergoing primary PCI. Atherosclerosis. 2011; 219:334–341.23. Lazzeri C, Valente S, Chiostri M, Sori A, Bernardo P, Gensini GF. Uric acid in the acute phase of ST elevation myocardial infarction submitted to primary PCI: its prognostic role and relation with inflammatory markers: a single center experience. Int J Cardiol. 2010; 138:206–209.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Exercise-Induced Vasospastic Angina With Prominent Regional Wall Motion Abnormality
- Interference of Bilirubin in Measurement of Uric Acid
- Diagnostic Significance of ECG Ergonovine Provocation Test in Patients with Vasospastic Angina
- The Vasomotor Tone In Vasospastic Angina
- Letter to the Editor: When Claiming a U-shaped Association between Uric Acid Levels and Major Adverse Cardiac Events, Perhaps Show the Evidence?