Recovery Rates of Non-Tuberculous Mycobacteria from Clinical Specimens Are Increasing in Korean Tertiary-Care Hospitals
- Affiliations
-
- 1Department of Laboratory Medicine, Pusan National University Hospital, Busan, Korea.
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 3Department of Laboratory Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea. cchl@pusan.ac.kr
- KMID: 2439459
- DOI: http://doi.org/10.3346/jkms.2017.32.8.1263
Abstract
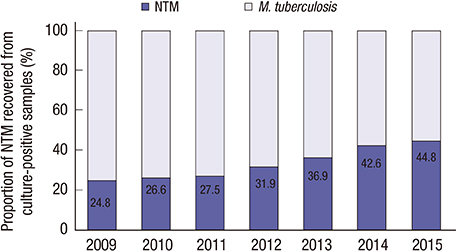
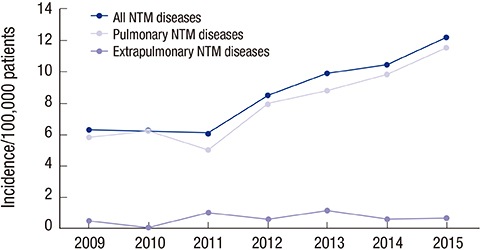
- Non-tuberculous mycobacteria (NTM) are being recognized increasingly as the causative agents of opportunistic infections in humans. This study investigated the epidemiologic trends of NTM recovery from various clinical specimens in 2 Korean tertiary-care hospitals. We reviewed the laboratory records of patient samples cultured for mycobacteria between 2009 and 2015 at 2 tertiary-care hospitals in Korea. The medical records for patients with positive NTM samples were also reviewed. During the study period, 144,540 specimens were cultured for mycobacteria. The proportion of NTM-positive samples increased from 23.3% in 2009 to 48.2% in 2015. The 2 most frequently isolated NTM were Mycobacterium intracellulare (38.3%) and M. avium (23.1%). The number of clinically significant diseases caused by NTM in inpatients and outpatients increased from 6.8 to 12.9 per 100,000 patients over the same period. The rates of recovery of NTM from clinical specimens and the number of patients with NTM infections increased significantly (P < 0.001, testing for trend) between 2009 and 2015.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Changing Epidemiology of Nontuberculous Mycobacterial Lung Diseases in a Tertiary Referral Hospital in Korea between 2001 and 2015
Ryoung-Eun Ko, Seong Mi Moon, Soohyun Ahn, Byung Woo Jhun, Kyeongman Jeon, O Jung Kwon, Hee Jae Huh, Chang-Seok Ki, Nam Yong Lee, Won-Jung Koh
J Korean Med Sci. 2018;33(8):. doi: 10.3346/jkms.2018.33.e65.Treatment of Extrapulmonary Nontuberculous Mycobacterial Diseases
Yu Mi Wi
Infect Chemother. 2019;51(3):245-255. doi: 10.3947/ic.2019.51.3.245.Diagnosis of pulmonary tuberculosis
Byung Woo Jhun, Hee Jae Huh, Won-Jung Koh
J Korean Med Assoc. 2019;62(1):18-24. doi: 10.5124/jkma.2019.62.1.18.Infection Source and Epidemiology of Nontuberculous Mycobacterial Lung Disease
Doosoo Jeon
Tuberc Respir Dis. 2019;82(2):94-101. doi: 10.4046/trd.2018.0026.
Reference
-
1. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, Holland SM, Horsburgh R, Huitt G, Iademarco MF, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007; 175:367–416.2. Saleeb P, Olivier KN. Pulmonary nontuberculous mycobacterial disease: new insights into risk factors for susceptibility, epidemiology, and approaches to management in immunocompetent and immunocompromised patients. Curr Infect Dis Rep. 2010; 12:198–203.3. Khan K, Wang J, Marras TK. Nontuberculous mycobacterial sensitization in the United States: national trends over three decades. Am J Respir Crit Care Med. 2007; 176:306–313.4. Billinger ME, Olivier KN, Viboud C, de Oca RM, Steiner C, Holland SM, Prevots DR. Nontuberculous mycobacteria-associated lung disease in hospitalized persons, United States, 1998–2005. Emerg Infect Dis. 2009; 15:1562–1569.5. Thomson RM. NTM working group at Queensland TB Control Centre and Queensland Mycobacterial Reference Laboratory. Changing epidemiology of pulmonary nontuberculous mycobacteria infections. Emerg Infect Dis. 2010; 16:1576–1583.6. Cook JL. Nontuberculous mycobacteria: opportunistic environmental pathogens for predisposed hosts. Br Med Bull. 2010; 96:45–59.7. Ryoo SW, Shin S, Shim MS, Park YS, Lew WJ, Park SN, Park YK, Kang S. Spread of nontuberculous mycobacteria from 1993 to 2006 in Koreans. J Clin Lab Anal. 2008; 22:415–420.8. Chae DR, Kim YI, Kee SJ, Kim YH, Chi SY, Ban HJ, Kwon YS, Oh IJ, Kim KS, Kim SO, et al. The impact of the 2007 ATS/IDSA diagnostic criteria for nontuberculous mycobacterial disease on the diagnosis of nontuberculous mycobacterial lung disease. Respiration. 2011; 82:124–129.9. Pfyffer GE. Mycobacterium: general characteristics, laboratory detection, and staining procedures. In : Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW, editors. Manual of Clinical Microbiology. 11th ed. Washington, D.C.: ASM Press;2015. p. 536–569.10. Lee SK, Lee EJ, Kim SK, Chang J, Jeong SH, Kang YA. Changing epidemiology of nontuberculous mycobacterial lung disease in South Korea. Scand J Infect Dis. 2012; 44:733–738.11. Koh WJ, Chang B, Jeong BH, Jeon K, Kim SY, Lee NY, Ki CS, Kwon OJ. Increasing recovery of nontuberculous mycobacteria from respiratory specimens over a 10-year period in a tertiary referral hospital in South Korea. Tuberc Respir Dis (Seoul). 2013; 75:199–204.12. Park YS, Lee CH, Lee SM, Yang SC, Yoo CG, Kim YW, Han SK, Shim YS, Yim JJ. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis. 2010; 14:1069–1071.13. Sakatani M. The non-tuberculous mycobacteriosis. Kekkaku. 2005; 80:25–30.14. Management of opportunist mycobacterial infections: Joint Tuberculosis Committee Guidelines 1999. Subcommittee of the Joint Tuberculosis Committee of the British Thoracic Society. Thorax. 2000; 55:210–218.15. Ding LW, Lai CC, Lee LN, Hsueh PR. Disease caused by non-tuberculous mycobacteria in a university hospital in Taiwan, 1997–2003. Epidemiol Infect. 2006; 134:1060–1067.16. Simner PJ, Stenger S, Richter E, Brown-Elliott BA, Wallace RJ, Wengenack NL. Mycobacterium: laboratory characteristics of slowly growing mycobacteria. In : Jorgensen JH, Pfaller MA, Carroll KC, Funke G, Landry ML, Richter SS, Warnock DW, editors. Manual of Clinical Microbiology. 11th ed. Washington, D.C.: ASM Press;2015. p. 570–594.17. Falkinham JO 3rd. Ecology of nontuberculous mycobacteria--where do human infections come from? Semin Respir Crit Care Med. 2013; 34:95–102.18. Hong KS, Ahn JH, Choi EY, Jin HJ, Shin KC, Chung JH, Lee KH. Microbiologic distribution and clinical features of nontuberculous mycobacteria in the tertiary hospital in Daegu. Yeungnam Univ J Med. 2015; 32:71–79.19. Glassroth J. Pulmonary disease due to nontuberculous mycobacteria. Chest. 2008; 133:243–251.20. Kim CK, Sung H, Park YJ, Chang CL. A proposal for laboratory workflow changes for efficient tuberculosis control. Ann Clin Microbiol. 2013; 16:61–68.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Three Egg-based Solid Media for Culture of Mycobacteria from Clinical Specimens
- Identification of Mycobacteria Species by HPLC and Species Distribution during Five Years at Ulsan University Hospital
- Increasing Recovery of Nontuberculous Mycobacteria from Respiratory Specimens over a 10-Year Period in a Tertiary Referral Hospital in South Korea
- Identification of Mycobacteria using High Performance Liquid Chromatography in Clinical Specimens
- Increasing Trend of Isolation of Non-Tuberculous Mycobacteria in a Tertiary University Hospital in South Korea