Ann Dermatol.
2019 Apr;31(2):139-145. 10.5021/ad.2019.31.2.139.
Efficacy and Safety of Oral Alitretinoin in Hand Eczema and Palmoplantar Pustulosis in Korean Patients
- Affiliations
-
- 1Department of Dermatology, SMG-SNU Boramae Medical Center, Seoul, Korea. sycho@snu.ac.kr
- 2Institute of Human-Environmental Interface Biology, Medical Research Center, Seoul National University, Seoul, Korea.
- 3Department of Biomedical Science, Seoul National University Graduate School, Seoul, Korea.
- 4Department of Dermatology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2439059
- DOI: http://doi.org/10.5021/ad.2019.31.2.139
Abstract
- BACKGROUND
Previous studies have demonstrated efficacy and safety of oral alitretinoin in hand eczema (HE) whereas in palmoplantar pustulosis (PPP), which can be difficult to distinguish from HE, efficacy of alitretinoin is still controversial.
OBJECTIVE
This study aimed to investigate the efficacy and safety of oral alitretinoin in HE and PPP and factors that affect the response of these disorders to alitretinoin.
METHODS
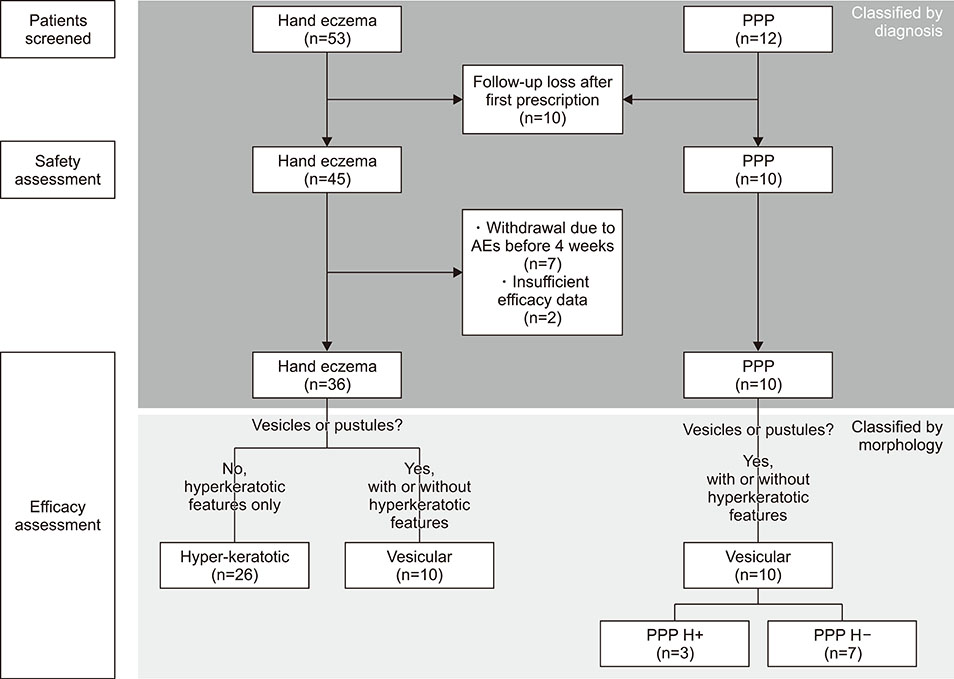
We retrospectively analyzed Korean adult patients with moderate-to-severe HE and PPP treated with oral alitretinoin, 46 patients for efficacy assessment and 55 patients for safety assessment.
RESULTS
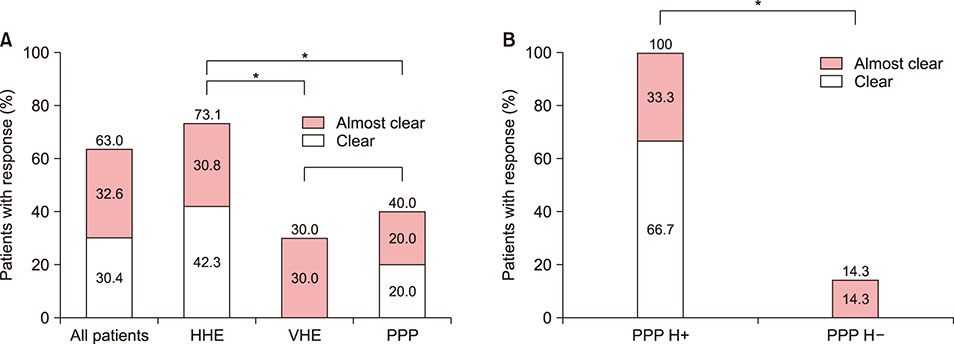
Among 46 patients who were treated with alitretinoin for at least 1 month, 29 patients (61.1% in HE and 40.0% in PPP) showed response to alitretinoin in the median 14 weeks after treatment. Hyperkeratotic HE showed higher response rate than either vesicular HE or PPP (p=0.026 and p=0.026, respectively). However, PPP with hyperkeratotic features showed as much response as hyperkeratotic HE (p=0.554). When responders and non-responders in total patients were compared, morphology, not diagnosis or initial severity, was the only significantly different factor between the two groups. After alitretinoin discontinuation in responders, relapse rate was 63.6% (7/11) and median time to relapse was 150 days (range, 76~730 days). Adverse events occurred in 47.3% (26/55); however, there were no serious adverse events.
CONCLUSION
In HE or PPP, lesions with hyperkeratotic morphology can be predicted to respond well to alitretinoin regardless of diagnosis.
MeSH Terms
Figure
Reference
-
1. Fowler JF, Duh MS, Chang J, Person J, Thorn D, Raut M, et al. A survey-based assessment of the prevalence and severity of chronic hand dermatitis in a managed care organization. Cutis. 2006; 77:385–392.2. Meding B, Järvholm B. Hand eczema in Swedish adults-changes in prevalence between 1983 and 1996. J Invest Dermatol. 2002; 118:719–723.
Article3. Diepgen TL, Andersen KE, Brandao FM, Bruze M, Bruynzeel DP, Frosch P, et al. Hand eczema classification: a cross-sectional, multicentre study of the aetiology and morphology of hand eczema. Br J Dermatol. 2009; 160:353–358.
Article4. Agner T, Andersen KE, Brandao FM, Bruynzeel DP, Bruze M, Frosch P, et al. Hand eczema severity and quality of life: a cross-sectional, multicentre study of hand eczema patients. Contact Dermatitis. 2008; 59:43–47.
Article5. Misiak-Galazka M, Wolska H, Rudnicka L. What do we know about palmoplantar pustulosis? J Eur Acad Dermatol Venereol. 2017; 31:38–44.
Article6. Yoon SY, Park HS, Lee JH, Cho S. Histological differentiation between palmoplantar pustulosis and pompholyx. J Eur Acad Dermatol Venereol. 2013; 27:889–893.
Article7. Mrowietz U, van de Kerkhof PC. Management of palmoplantar pustulosis: do we need to change? Br J Dermatol. 2011; 164:942–946.
Article8. Diepgen TL, Pfarr E, Zimmermann T. Efficacy and tolerability of alitretinoin for chronic hand eczema under daily practice conditions: results of the TOCCATA open study comprising 680 patients. Acta Derm Venereol. 2012; 92:251–255.
Article9. Ruzicka T, Lynde CW, Jemec GB, Diepgen T, Berth-Jones J, Coenraads PJ, et al. Efficacy and safety of oral alitretinoin (9-cis retinoic acid) in patients with severe chronic hand eczema refractory to topical corticosteroids: results of a randomized, double-blind, placebo-controlled, multicentre trial. Br J Dermatol. 2008; 158:808–817.
Article10. Dirschka T, Reich K, Bissonnette R, Maares J, Brown T, Diepgen TL. An open-label study assessing the safety and efficacy of alitretinoin in patients with severe chronic hand eczema unresponsive to topical corticosteroids. Clin Exp Dermatol. 2011; 36:149–154.
Article11. Kwon HI, Kim JE, Ko JY, Ro YS. Efficacy and safety of alitretinoin for chronic hand eczema in Korean patients. Ann Dermatol. 2016; 28:364–370.
Article12. Reich K, Graff O, Mehta N. Oral alitretinoin treatment in patients with palmoplantar pustulosis inadequately responding to standard topical treatment: a randomized phase II study. Br J Dermatol. 2016; 174:1277–1281.
Article13. Irla N, Navarini AA, Yawalkar N. Alitretinoin abrogates innate inflammation in palmoplantar pustular psoriasis. Br J Dermatol. 2012; 167:1170–1174.
Article14. Jang S, Kim MW, Park HS, Yoon HS, Cho S. Helpful clinical features for differential diagnosis of palmoplantar pustulosis and pompholyx. Korean J Dermatol. 2017; 55:36–44.15. Park JY, Cho EB, Park EJ, Park HR, Kim KH, Kim KJ. The histopathological differentiation between palmar psoriasis and hand eczema: a retrospective review of 96 cases. J Am Acad Dermatol. 2017; 77:130–135.
Article16. Aydin O, Engin B, Oğuz O, Ilvan S, Demirkesen C. Non-pustular palmoplantar psoriasis: is histologic differentiation from eczematous dermatitis possible? J Cutan Pathol. 2008; 35:169–173.
Article17. Agner T, Aalto-Korte K, Andersen KE, Foti C, Gimenéz-Arnau A, Goncalo M, et al. Classification of hand eczema. J Eur Acad Dermatol Venereol. 2015; 29:2417–2422.
Article18. Germain P, Chambon P, Eichele G, Evans RM, Lazar MA, Leid M, et al. International Union of Pharmacology. LXIII. Retinoid X receptors. Pharmacol Rev. 2006; 58:760–772.
Article19. Germain P, Chambon P, Eichele G, Evans RM, Lazar MA, Leid M, et al. International Union of Pharmacology. LX. Retinoic acid receptors. Pharmacol Rev. 2006; 58:712–725.
Article20. Hanifin JM, Stevens V, Sheth P, Breneman D. Novel treatment of chronic severe hand dermatitis with bexarotene gel. Br J Dermatol. 2004; 150:545–553.
Article21. Thestrup-Pedersen K, Andersen KE, Menné T, Veien NK. Treatment of hyperkeratotic dermatitis of the palms (eczema keratoticum) with oral acitretin. A single-blind placebo-controlled study. Acta Derm Venereol. 2001; 81:353–355.
Article22. Shi VY, Sivamani RK, Maibach HI. Alitretinoin for the treatment of chronic hand eczema: clinical rationale. Clin Invest (Lond). 2014; 4:763–773.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy and Safety of Alitretinoin for Chronic Hand Eczema in Korean Patients
- Efficacy and Safety of Oral Alitretinoin in Various Refractory Dermatologic Diseases: A Retrospective Study
- Efficacy and Safety of Alitretinoin Therapy in Korean Elderly Patients with Chronic Hand Eczema: A Retrospective Single Center Study
- Alitretinoin Compliance in Patients with Chronic Hand Eczema
- Effect of Oral Alitretinoin Therapy on Trachyonychia