Prolonged occlusion of the hepatoduodenal ligament to reduce risk of bleeding and tumor spread during recipient hepatectomy for living donor liver transplantation
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. shwang@amc.seoul.kr
- KMID: 2439047
- DOI: http://doi.org/10.14701/ahbps.2019.23.1.61
Abstract
- BACKGROUNDS/AIMS
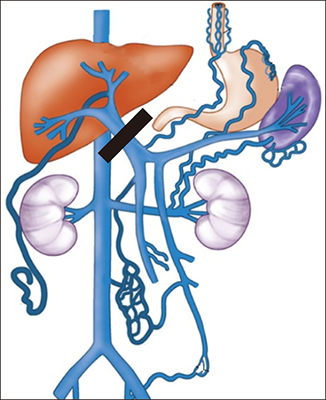
Prevention of excessive bleeding during liver transplantation (LT) operations presents a major challenge. Compared to deceased donor LT, living donor LT (LDLT) is more vulnerable to bleeding because of additional dissection procedures. We herein introduce our technique for prolonged occlusion of the hepatoduodenal ligament applied to recipient hepatectomy for LDLT.
METHODS
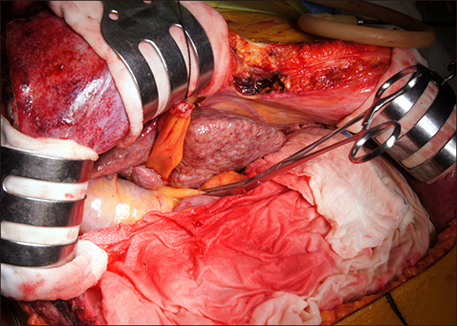
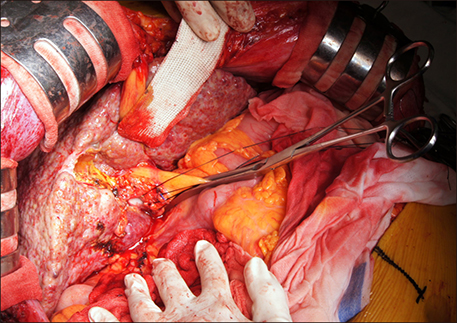
Simulated assessment of splanchnic hemodynamics on prolonged occlusion of the hepatoduodenal ligament showed that patients with cirrhotic liver appeared to tolerate the procedure as like in the patients with normal liver. We accumulated experience on the prolonged Pringle maneuver with curved intestinal clamps.
RESULTS
This technique was applied to more than 60 cases of adult LDLT operations from early 2014 until the end of 2018. Initially, application of this technique was limited to patients showing heavy bleeding during perihilar mobilization. Thereafter, this technique was applied at the start of liver mobilization and stopped after complete mobilization of the retro-hepatic vena cava. Recently, this technique was also applied during dissection of the hepatoduodenal ligament. The mean total occlusion duration was 67±13 minutes. No patient suffered from major serosal peritoneal tearing-associated bleeding or hepatic artery problems. Intentional prolonged occlusion over two hours was applied to five patients who had advanced hepatocellular carcinoma.
CONCLUSIONS
We believe that prolonged occlusion of the hepatoduodenal ligament is a simple effective method to reduce intraoperative bleeding, and that it has potential benefit to reduce the risk of intraoperative tumor spread during LDLT operations.
MeSH Terms
Figure
Cited by 3 articles
-
Prolonged hepatic inflow occlusion to reduce bleeding during recipient hepatectomy in living donor liver transplantation
Jin-Uk Choi, Shin Hwang, I-Ji Chung, Sang-Hyun Kang, Chul-Soo Ahn, Deok-Bog Moon, Tae-Yong Ha, Ki-Hun Kim, Gi-Won Song, Dong-Hwan Jung, Gil-Chun Park, Young-In Yoon, Hui-Dong Cho, Sung-Gyu Lee
Korean J Transplant. 2020;34(1):55-61. doi: 10.4285/kjt.2020.34.1.55.Recipient liver splitting to facilitate piggyback hepatectomy in adult living donor liver transplantation
Sung-Min Kim, Shin Hwang, Deok-Bog Moon, Dong-Hwan Jung
Korean J Transplant. 2021;35(2):124-129. doi: 10.4285/kjt.20.0055.Recipient hepatectomy under total hepatic vascular exclusion to prevent hepatocellular carcinoma spread in living donor liver transplantation
Young-In Yoon, Shin Hwang, Deok-Bog Moon, Dong-Hwan Jung, Sung-Gyu Lee
Korean J Transplant. 2021;35(2):130-136. doi: 10.4285/kjt.20.0056.
Reference
-
1. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 2006; 12:920–927.
Article2. Hwang S, Lee SG, Moon DB, Ahn CS, Kim KH, Lee YJ, et al. Salvage living donor liver transplantation after prior liver resection for hepatocellular carcinoma. Liver Transpl. 2007; 13:741–746.
Article3. Lee KF, Wong J, Cheung SYS, Chong CCN, Hui JWY, Leung VYF, et al. Does intermittent pringle maneuver increase postoperative complications after hepatectomy for hepatocellular carcinoma? A randomized controlled trial. World J Surg. 2018; 42:3302–3311.
Article4. Huang CJ, Cheng KW, Chen CL, Wu SC, Shih TH, Yang SC, et al. Predictive factors for pediatric patients requiring massive blood transfusion during living donor liver transplantation. Ann Transplant. 2013; 18:443–447.
Article5. Yoon JU, Byeon GJ, Park JY, Yoon SH, Ryu JH, Ri HS. Bloodless living donor liver transplantation: risk factors, outcomes, and diagnostic predictors. Medicine (Baltimore). 2018; 97:e13581.6. Pringle JH. V. Notes on the arrest of hepatic hemorrhage due to trauma. Ann Surg. 1908; 48:541–549.7. Park YK, Kim BW, Wang HJ, Xu W. Usefulness of the Pinch-Burn-Cut (PBC) technique for recipient hepatectomy in liver transplantation. Korean J Hepatobiliary Pancreat Surg. 2012; 16:13–16.
Article8. Lee KW, Joh JW, Kim SJ, Choi SH, Heo JS, Lee HH, et al. High hilar dissection: new technique to reduce biliary complication in living donor liver transplantation. Liver Transpl. 2004; 10:1158–1162.
Article9. Scatton O, Brustia R, Belli G, Pekolj J, Wakabayashi G, Gayet B. What kind of energy devices should be used for laparoscopic liver resection? Recommendations from a systematic review. J Hepatobiliary Pancreat Sci. 2015; 22:327–334.
Article10. Liu CL, Fan ST, Cheung ST, Lo CM, Ng IO, Wong J. Anterior approach versus conventional approach right hepatic resection for large hepatocellular carcinoma: a prospective randomized controlled study. Ann Surg. 2006; 244:194–203.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recipient liver splitting to facilitate piggyback hepatectomy in adult living donor liver transplantation
- Recipient hepatectomy under total hepatic vascular exclusion to prevent hepatocellular carcinoma spread in living donor liver transplantation
- Minimal-incision donor right hepatectomy for living donor liver transplantation
- Diaphragmatic herniation following donor hepatectomy for living donor liver transplantation: a serious complication not given due recognition
- Technical refinement of the anterior sectional drainage in right liver transplantation: a single center experience