Ann Hepatobiliary Pancreat Surg.
2019 Feb;23(1):13-19. 10.14701/ahbps.2019.23.1.13.
Partial ALPPS with a longer wait between procedures is safe and yields adequate future liver remnant hypertrophy
- Affiliations
-
- 1Cardiff Liver Unit, University Hospital of Wales, Cardiff, UK. nagappan.kumar@wales.nhs.uk
- 2Moritz Kaposi Teaching General Hospital, Kaposvár, Hungary.
- 3Department of Radiology, University Hospital of Wales, Cardiff, UK.
- 4Department of Surgery, Tan Tock Seng Hospital, Singapore.
- KMID: 2439041
- DOI: http://doi.org/10.14701/ahbps.2019.23.1.13
Abstract
- BACKGROUNDS/AIMS
Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) has generated controversy due to high morbidity and mortality. We present our series of patients with 30-40% parenchymal transection and minimal hilar dissection.
METHODS
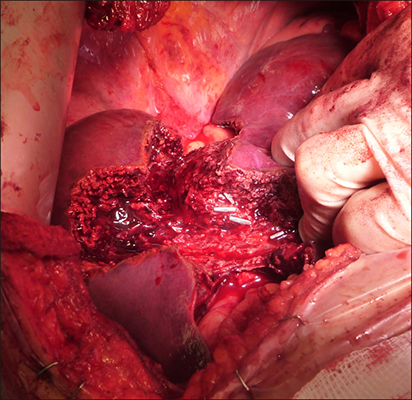
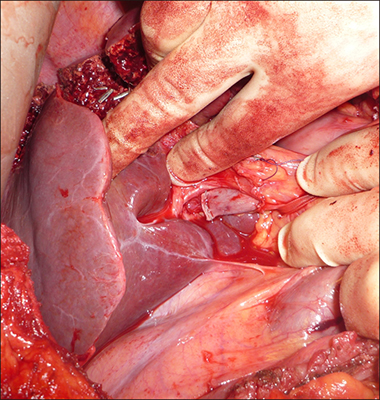
Patients who had partial ALPPS between April 2015 and April 2016 were included. Patients with colorectal liver metastases (CRLM) had their future liver remnants (FLR) cleared with metastasectomies. The liver was divided along the future line of transection to 30-40%, right portal vein was stapled and divided without extensive hilar dissection, with minimal handling of right liver, which was not mobilised. We preserved the middle hepatic vein. Data were collected prospectively for hypertrophy of the FLR, morbidity and mortality.
RESULTS
Among the 8 patients (age 25-68) investigated, one patient with cholangiocarcinoma had portal vein embolization prior to partial ALPPS. All patients completed two stages with adequate FLR hypertrophy at a median of 28 days. No mortality was found. The median length of stay after stages 1 and 2 was 9 and 9.6 days, respectively. The median increase in FLR was 38%.
CONCLUSIONS
A limited transection of 30-40%, minimal hilar dissection and longer wait between stages yielded adequate FLR hypertrophy with low morbidity and no mortality.
MeSH Terms
Figure
Cited by 1 articles
-
How successful is liver resection for colorectal cancer liver metastases in patients over 75 years old?
Nicholas George Mowbray, Carven Chin, Patricia Duncan, David O'Reilly, Zsolt Kaposztas, Sameer Junnarkar, Nagappan Kumar
Ann Hepatobiliary Pancreat Surg. 2021;25(1):18-24. doi: 10.14701/ahbps.2021.25.1.18.
Reference
-
1. Adams RB, Aloia TA, Loyer E, Pawlik TM, Taouli B, Vauthey JN. Selection for hepatic resection of colorectal liver metastases: expert consensus statement. HPB (Oxford). 2013; 15:91–103.2. Bismuth H, Adam R, Lévi F, Farabos C, Waechter F, Castaing D, et al. Resection of nonresectable liver metastases from colorectal cancer after neoadjuvant chemotherapy. Ann Surg. 1996; 224:509–520.3. Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010; 11:38–47.4. Lam VW, Spiro C, Laurence JM, Johnston E, Hollands MJ, Pleass HC, et al. A systematic review of clinical response and survival outcomes of downsizing systemic chemotherapy and rescue liver surgery in patients with initially unresectable colorectal liver metastases. Ann Surg Oncol. 2012; 19:1292–1301.
Article5. van Lienden KP, van den Esschert JW, de Graaf W, Bipat S, Lameris JS, van Gulik TM, et al. Portal vein embolization before liver resection: a systematic review. Cardiovasc Intervent Radiol. 2013; 36:25–34.
Article6. Capussotti L, Muratore A, Baracchi F, Lelong B, Ferrero A, Regge D, et al. Portal vein ligation as an efficient method of increasing the future liver remnant volume in the surgical treatment of colorectal metastases. Arch Surg. 2008; 143:978–982.7. Adam R, Laurent A, Azoulay D, Castaing D, Bismuth H. Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg. 2000; 232:777–785.
Article8. Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012; 255:405–414.9. Dupré A, Hitier M, Peyrat P, Chen Y, Meeus P, Rivoire M. Associating portal embolization and artery ligation to induce rapid liver regeneration in staged hepatectomy. Br J Surg. 2015; 102:1541–1550.10. Schadde E, Raptis DA, Schnitzbauer AA, Ardiles V, Tschuor C, Lesurtel M, et al. Prediction of mortality after ALPPS stage-1: an analysis of 320 patients from the International ALPPS Registry. Ann Surg. 2015; 262:780–785.11. Figueras J, Belghiti J. The ALPPS approach: should we sacrifice basic therapeutic rules in the name of innovation. World J Surg. 2014; 38:1520–1521.12. Oldhafer KJ, Donati M, Jenner RM, Stang A, Stavrou GA. ALPPS for patients with colorectal liver metastases: effective liver hypertrophy, but early tumor recurrence. World J Surg. 2014; 38:1504–1509.
Article13. Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, et al. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995; 21:1317–1321.14. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213.15. Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011; 149:713–724.
Article16. de Santibañes E, Alvarez FA, Ardiles V, Pekolj J, de Santibañes M. Inverting the ALPPS paradigm by minimizing first stage impact: the Mini-ALPPS technique. Langenbecks Arch Surg. 2016; 401:557–563.17. Li J, Kantas A, Ittrich H, Koops A, Achilles EG, Fischer L, et al. Avoid “all-touch” by hybrid ALPPS to achieve oncological efficacy. Ann Surg. 2016; 263:e6–e7.18. Adam R, Imai K, Castro Benitez C, Allard MA, Vibert E, Sa Cunha A, et al. Outcome after associating liver partition and portal vein ligation for staged hepatectomy and conventional two-stage hepatectomy for colorectal liver metastases. Br J Surg. 2016; 103:1521–1529.
Article19. Moris D, Ronnekleiv-Kelly S, Kostakis ID, Tsilimigras DI, Beal EW, Papalampros A, et al. Operative results and oncologic outcomes of Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) versus Two-Stage Hepatectomy (TSH) in patients with unresectable colorectal liver metastases: a systematic review and meta-analysis. World J Surg. 2018; 42:806–815.20. Matsuo K, Murakami T, Kawaguchi D, Hiroshima Y, Koda K, Yamazaki K, et al. Histologic features after surgery associating liver partition and portal vein ligation for staged hepatectomy versus those after hepatectomy with portal vein embolization. Surgery. 2016; 159:1289–1298.21. Zeile M, Bakal A, Volkmer JE, Stavrou GA, Dautel P, Hoeltje J, et al. Identification of cofactors influencing hypertrophy of the future liver remnant after portal vein embolization-the effect of collaterals on embolized liver volume. Br J Radiol. 2016; 89:20160306.22. Schadde E, Schnitzbauer AA, Tschuor C, Raptis DA, Bechstein WO, Clavien PA. Systematic review and meta-analysis of feasibility, safety, and efficacy of a novel procedure: associating liver partition and portal vein ligation for staged hepatectomy. Ann Surg Oncol. 2015; 22:3109–3120.23. Røsok BI, Björnsson B, Sparrelid E, Hasselgren K, Pomianowska E, Gasslander T, et al. Scandinavian multicenter study on the safety and feasibility of the associating liver partition and portal vein ligation for staged hepatectomy procedure. Surgery. 2016; 159:1279–1286.
Article24. Belghiti J, Dokmak S, Schadde E. ALPPS: innovation for innovation's sake. Surgery. 2016; 159:1287–1288.
Article25. Cieslak KP, Olthof PB, van Lienden KP, Besselink MG, Busch OR, van Gulik TM, et al. Assessment of liver function using (99m)Tc-mebrofenin hepatobiliary scintigraphy in ALPPS (Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy). Case Rep Gastroenterol. 2015; 9:353–360.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associated Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Registry: What Have We Learned?
- Associating microwave ablation and portal vein ligation for staged hepatectomy for the treatment of huge hepatocellular carcinoma with cirrhosis
- A minimally invasive first stage of ALPPS for hepatoblastoma in a child
- Two cases of ALPPS procedure: simultaneous ALPPS and colorectal resection and ALPPS procedure for hepatic malignancy larger than 15 centimeter
- Monosegment associating liver partition and portal vein ligation for staged hepatectomy: Preserving segment 1 as the only liver remnant after hepatocellular carcinoma recurrence