Intest Res.
2019 Jan;17(1):24-35. 10.5217/ir.2018.00128.
Successful transition from pediatric to adult care in inflammatory bowel disease: what is the key?
- Affiliations
-
- 1Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. bdye@amc.seoul.kr
- 2Department of Inflammatory Bowel Disease Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2438440
- DOI: http://doi.org/10.5217/ir.2018.00128
Abstract
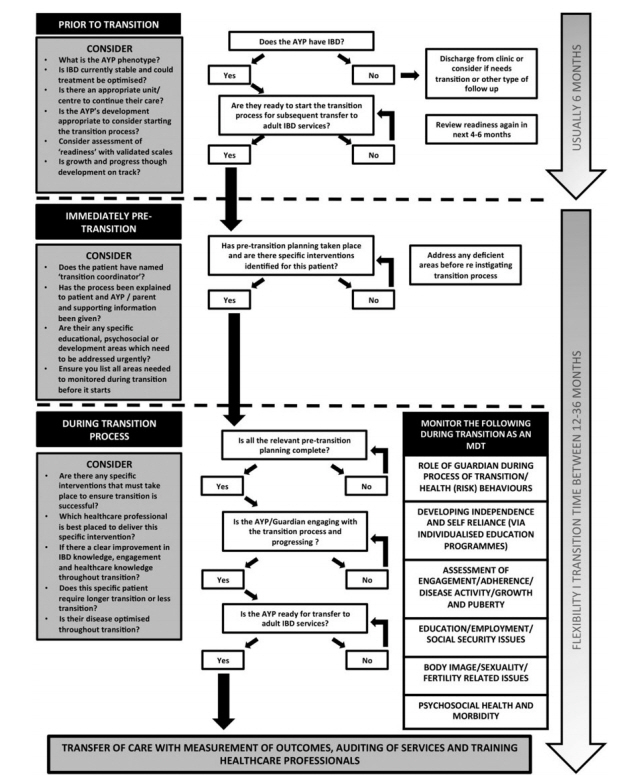
- The incidence of pediatric-onset inflammatory bowel disease (IBD) is on the rise, accounting for up to 25% of IBD cases. Pediatric IBD often has extensive bowel involvement with aggressive and rapidly progressing behavior compared to adult IBD. Because IBD has a high morbidity rate and can have a lifelong impact, successful transition from pediatric to adult care is important to maintain the continuity of care. Furthermore, successful transition facilitates appropriate development and psychosocial well-being among patients, as well as comprehensive and harmonious healthcare delivery amongst stakeholders. However, there are various obstacles related to patients, family, providers, and organizations that interfere with successful transition. Successful transition requires a flexible and tailored plan that is made according to the patient's developmental abilities and situation. This plan should be established through periodic interviews with the patient and family and through close collaboration with other care providers. Through a stepwise approach to the transition process, patients' knowledge and self-management skills can be improved. After preparation for the transition is completed and the obstacles are overcome, patients can be gradually moved to adult care. Finally, successful transition can increase patients' adherence to therapy, maintain the appropriate health status, improve patients' self-management, and promote self-reliance among patients.
MeSH Terms
Figure
Cited by 1 articles
-
How Can We Do Transition Successfully from Pediatric to Adult Clinics in Inflammatory Bowel Disease?
Mi Jin Kim, Sung Noh Hong, Young-Ho Kim, Yon Ho Choe
Korean J Gastroenterol. 2021;77(5):227-230. doi: 10.4166/kjg.2021.065.
Reference
-
1. Benchimol EI, Fortinsky KJ, Gozdyra P, Van den Heuvel M, Van Limbergen J, Griffiths AM. Epidemiology of pediatric inflammatory bowel disease: a systematic review of international trends. Inflamm Bowel Dis. 2011; 17:423–439.
Article2. Benchimol EI, Mack DR, Nguyen GC, et al. Incidence, outcomes, and health services burden of very early onset inflammatory bowel disease. Gastroenterology. 2014; 147:803–813.
Article3. Afzali A, Katz S. Inflammatory bowel disease in the baby to baby boomer: pediatric and elderly onset of IBD. Curr Treat Options Gastroenterol. 2018; 16:289–305.
Article4. Sýkora J, Pomahačová R, Kreslová M, Cvalínová D, Štych P, Schwarz J. Current global trends in the incidence of pediatric-onset inflammatory bowel disease. World J Gastroenterol. 2018; 24:2741–2763.
Article5. Paul T, Birnbaum A, Pal DK, et al. Distinct phenotype of early childhood inflammatory bowel disease. J Clin Gastroenterol. 2006; 40:583–586.
Article6. Van Limbergen J, Russell RK, Drummond HE, et al. Definition of phenotypic characteristics of childhood-onset inflammatory bowel disease. Gastroenterology. 2008; 135:1114–1122.
Article7. Goodhand J, Hedin CR, Croft NM, Lindsay JO. Adolescents with IBD: the importance of structured transition care. J Crohns Colitis. 2011; 5:509–519.8. Hait EJ, Barendse RM, Arnold JH, et al. Transition of adolescents with inflammatory bowel disease from pediatric to adult care: a survey of adult gastroenterologists. J Pediatr Gastroenterol Nutr. 2009; 48:61–65.
Article9. Sebastian S, Jenkins H, McCartney S, et al. The requirements and barriers to successful transition of adolescents with inflammatory bowel disease: differing perceptions from a survey of adult and paediatric gastroenterologists. J Crohns Colitis. 2012; 6:830–844.
Article10. American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002; 110:1304–1306.11. American Academy of Pediatrics; American Academy of Family Physicians; American College of Physicians. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011; 128:182–200.12. Gray WN, Maddux MH. Current transition practices in pediatric IBD: findings from a national survey of pediatric providers. Inflamm Bowel Dis. 2016; 22:372–379.13. Gray WN, Holbrook E, Morgan PJ, Saeed SA, Denson LA, Hommel KA. Transition readiness skills acquisition in adolescents and young adults with inflammatory bowel disease: findings from integrating assessment into clinical practice. Inflamm Bowel Dis. 2015; 21:1125–1131.
Article14. Zeisler B, Hyams JS. Transition of management in adolescents with IBD. Nat Rev Gastroenterol Hepatol. 2014; 11:109–115.
Article15. Clarke T, Lusher J. Transitioning patients with inflammatory bowel disease (IBD) from adolescent to adult services: a systematic review. Frontline Gastroenterol. 2016; 7:264–270.
Article16. Afzali A, Wahbeh G. Transition of pediatric to adult care in inflammatory bowel disease: is it as easy as 1, 2, 3? World J Gastroenterol. 2017; 23:3624–3631.
Article17. van Rheenen PF, Aloi M, Biron IA, et al. European Crohn’s and Colitis Organisation topical review on transitional care in inflammatory bowel disease. J Crohns Colitis. 2017; 11:1032–1038.
Article18. Philpott JR, Kurowski JA. Challenges in transitional care in inflammatory bowel disease: a review of the current literature in transition readiness and outcomes. Inflamm Bowel Dis. 2019; 25:45–55.
Article19. Duricova D, Fumery M, Annese V, Lakatos PL, Peyrin-Biroulet L, Gower-Rousseau C. The natural history of Crohn’s disease in children: a review of population-based studies. Eur J Gastroenterol Hepatol. 2017; 29:125–134.20. Heyman MB, Kirschner BS, Gold BD, et al. Children with early-onset inflammatory bowel disease (IBD): analysis of a pediatric IBD consortium registry. J Pediatr. 2005; 146:35–40.
Article21. Vernier-Massouille G, Balde M, Salleron J, et al. Natural history of pediatric Crohn’s disease: a population-based cohort study. Gastroenterology. 2008; 135:1106–1113.
Article22. Kappelman MD, Rifas-Shiman SL, Kleinman K, et al. The prevalence and geographic distribution of Crohn’s disease and ulcerative colitis in the United States. Clin Gastroenterol Hepatol. 2007; 5:1424–1429.
Article23. Ishige T, Tomomasa T, Takebayashi T, et al. Inflammatory bowel disease in children: epidemiological analysis of the nationwide IBD registry in Japan. J Gastroenterol. 2010; 45:911–917.
Article24. Cosnes J, Gower-Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011; 140:1785–1794.
Article25. Bernstein CN, Wajda A, Svenson LW, et al. The epidemiology of inflammatory bowel disease in Canada: a population-based study. Am J Gastroenterol. 2006; 101:1559–1568.
Article26. Oh SH, Kim KM. Current issues of pediatric inflammatory bowel disease in Korea. Korean J Pediatr. 2014; 57:465–471.
Article27. Adamiak T, Walkiewicz-Jedrzejczak D, Fish D, et al. Incidence, clinical characteristics, and natural history of pediatric IBD in Wisconsin: a population-based epidemiological study. Inflamm Bowel Dis. 2013; 19:1218–1223.
Article28. Charpentier C, Salleron J, Savoye G, et al. Natural history of elderly-onset inflammatory bowel disease: a population-based cohort study. Gut. 2014; 63:423–432.
Article29. de Bie CI, Paerregaard A, Kolacek S, et al. Disease phenotype at diagnosis in pediatric Crohn’s disease: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis. 2013; 19:378–385.30. Levine A, de Bie CI, Turner D, et al. Atypical disease phenotypes in pediatric ulcerative colitis: 5-year analyses of the EUROKIDS Registry. Inflamm Bowel Dis. 2013; 19:370–377.31. Hong SJ, Cho SM, Choe BH, et al. Characteristics and incidence trends for pediatric inflammatory bowel disease in Daegu-Kyungpook Province in Korea: a multi-center study. J Korean Med Sci. 2018; 33:e132.
Article32. Kim HJ, Oh SH, Kim DY, et al. Clinical characteristics and longterm outcomes of paediatric Crohn’s disease: a single-centre experience. J Crohns Colitis. 2017; 11:157–164.
Article33. Wang XQ, Xiao Y, Xu X, et al. Study of disease phenotype and its association with prognosis of paediatric inflammatory bowel disease in China. BMC Pediatr. 2018; 18:229.
Article34. Pigneur B, Seksik P, Viola S, et al. Natural history of Crohn’s disease: comparison between childhood- and adult-onset disease. Inflamm Bowel Dis. 2010; 16:953–961.35. Nasiri S, Kuenzig ME, Benchimol EI. Long-term outcomes of pediatric inflammatory bowel disease. Semin Pediatr Surg. 2017; 26:398–404.
Article36. Fumery M, Duricova D, Gower-Rousseau C, Annese V, Peyrin-Biroulet L, Lakatos PL. Review article: the natural history of paediatric-onset ulcerative colitis in population-based studies. Aliment Pharmacol Ther. 2016; 43:346–355.
Article37. Griffiths AM. Specificities of inflammatory bowel disease in childhood. Best Pract Res Clin Gastroenterol. 2004; 18:509–523.
Article38. Vaisman N, Dotan I, Halack A, Niv E. Malabsorption is a major contributor to underweight in Crohn’s disease patients in remission. Nutrition. 2006; 22:855–859.
Article39. Gasparetto M, Guariso G. Crohn’s disease and growth deficiency in children and adolescents. World J Gastroenterol. 2014; 20:13219–13233.
Article40. Rosen MJ, Dhawan A, Saeed SA. Inflammatory bowel disease in children and adolescents. JAMA Pediatr. 2015; 169:1053–1060.
Article41. Heuschkel R, Salvestrini C, Beattie RM, Hildebrand H, Walters T, Griffiths A. Guidelines for the management of growth failure in childhood inflammatory bowel disease. Inflamm Bowel Dis. 2008; 14:839–849.
Article42. Ley D, Duhamel A, Behal H, et al. Growth pattern in paediatric Crohn disease is related to inflammatory status. J Pediatr Gastroenterol Nutr. 2016; 63:637–643.
Article43. Lee JJ, Escher JC, Shuman MJ, et al. Final adult height of children with inflammatory bowel disease is predicted by parental height and patient minimum height Z-score. Inflamm Bowel Dis. 2010; 16:1669–1677.44. Davies JH, Evans BA, Gregory JW. Bone mass acquisition in healthy children. Arch Dis Child. 2005; 90:373–378.45. Jakobsen C, Paerregaard A, Munkholm P, et al. Pediatric inflammatory bowel disease: increasing incidence, decreasing surgery rate, and compromised nutritional status: a prospective population-based cohort study 2007-2009. Inflamm Bowel Dis. 2011; 17:2541–2550.
Article46. Ballinger AB, Savage MO, Sanderson IR. Delayed puberty associated with inflammatory bowel disease. Pediatr Res. 2003; 53:205–210.47. Perminow G, Brackmann S, Lyckander LG, et al. A characterization in childhood inflammatory bowel disease, a new population-based inception cohort from South-Eastern Norway, 2005-07, showing increased incidence in Crohn’s disease. Scand J Gastroenterol. 2009; 44:446–456.
Article48. Duigenan S, Gee MS. Imaging of pediatric patients with inflammatory bowel disease. AJR Am J Roentgenol. 2012; 199:907–915.49. Towbin AJ, Sullivan J, Denson LA, Wallihan DB, Podberesky DJ. CT and MR enterography in children and adolescents with inflammatory bowel disease. Radiographics. 2013; 33:1843–1860.50. Pall H, Zacur GM, Kramer RE, et al. Bowel preparation for pediatric colonoscopy: report of the NASPGHAN endoscopy and procedures committee. J Pediatr Gastroenterol Nutr. 2014; 59:409–416.51. Ruemmele FM, Veres G, Kolho KL, et al. Consensus guidelines of ECCO/ESPGHAN on the medical management of pediatric Crohn’s disease. J Crohns Colitis. 2014; 8:1179–1207.52. Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977-2009. Am J Gastroenterol. 2012; 107:579–588.
Article53. Vilar P, de Carpi JM, Acuña CE, Masiques MA. Infliximab in paediatric inflammatory bowel disease. J Crohns Colitis. 2007; 1:2–9.
Article54. Ruemmele FM, Turner D. Differences in the management of pediatric and adult onset ulcerative colitis: lessons from the joint ECCO and ESPGHAN consensus guidelines for the management of pediatric ulcerative colitis. J Crohns Colitis. 2014; 8:1–4.
Article55. Jakobsen C, Bartek J Jr, Wewer V, et al. Differences in phenotype and disease course in adult and paediatric inflammatory bowel disease: a population-based study. Aliment Pharmacol Ther. 2011; 34:1217–1224.
Article56. Frolkis AD, Dykeman J, Negrón ME, et al. Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 2013; 145:996–1006.
Article57. Malik S, Ahmed SF, Wilson ML, et al. The effects of anti-TNFalpha treatment with adalimumab on growth in children with Crohn’s disease (CD). J Crohns Colitis. 2012; 6:337–344.
Article58. Borrelli O, Bascietto C, Viola F, et al. Infliximab heals intestinal inflammatory lesions and restores growth in children with Crohn’s disease. Dig Liver Dis. 2004; 36:342–347.
Article59. Walters TD, Gilman AR, Griffiths AM. Linear growth improves during infliximab therapy in children with chronically active severe Crohn’s disease. Inflamm Bowel Dis. 2007; 13:424–430.
Article60. Malik S, Wong SC, Bishop J, et al. Improvement in growth of children with Crohn disease following anti-TNF-alpha therapy can be independent of pubertal progress and glucocorticoid reduction. J Pediatr Gastroenterol Nutr. 2011; 52:31–37.
Article61. Blum RW, Garell D, Hodgman CH, et al. Transition from childcentered to adult health-care systems for adolescents with chronic conditions: a position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993; 14:570–576.
Article62. Gumidyala AP, Greenley RN, Plevinsky JM, et al. Moving on: transition readiness in adolescents and young adults with IBD. Inflamm Bowel Dis. 2018; 24:482–489.
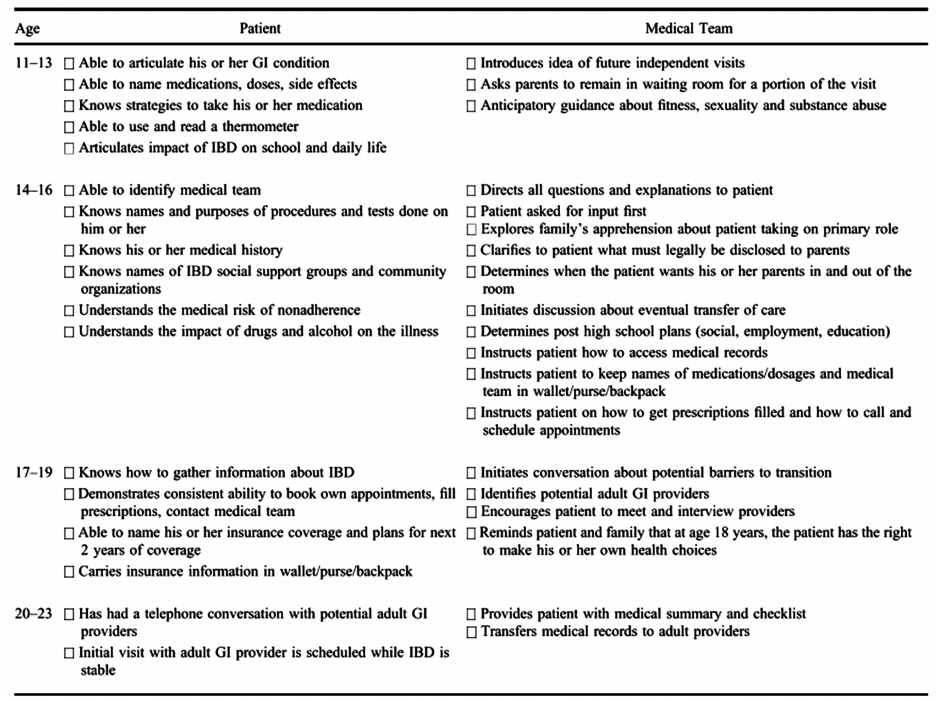
Article63. Hait E, Arnold JH, Fishman LN. Educate, communicate, anticipate-practical recommendations for transitioning adolescents with IBD to adult health care. Inflamm Bowel Dis. 2006; 12:70–73.
Article64. Baldassano R, Ferry G, Griffiths A, Mack D, Markowitz J, Winter H. Transition of the patient with inflammatory bowel disease from pediatric to adult care: recommendations of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2002; 34:245–248.
Article65. de Silva PS, Fishman LN. Transition of the patient with IBD from pediatric to adult care-an assessment of current evidence. Inflamm Bowel Dis. 2014; 20:1458–1464.
Article66. Campbell F, Biggs K, Aldiss SK, et al. Transition of care for adolescents from paediatric services to adult health services. Cochrane Database Syst Rev. 2016; 4:CD009794.
Article67. Sawyer SM, Afifi RA, Bearinger LH, et al. Adolescence: a foundation for future health. Lancet. 2012; 379:1630–1640.
Article68. Gray WN, Schaefer MR, Resmini-Rawlinson A, Wagoner ST. Barriers to transition from pediatric to adult care: a systematic review. J Pediatr Psychol. 2018; 43:488–502.
Article69. Keefer L, Kiebles JL, Taft TH. The role of self-efficacy in inflammatory bowel disease management: preliminary validation of a disease-specific measure. Inflamm Bowel Dis. 2011; 17:614–620.70. Hommel KA, Greenley RN, Maddux MH, Gray WN, Mackner LM. Self-management in pediatric inflammatory bowel disease: a clinical report of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2013; 57:250–257.71. Kahn SA. the transition from pediatric to adult inflammatory bowel disease care. Gastroenterol Hepatol (N Y). 2016; 12:403–406.72. Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ: Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011; 36:160–171.
Article73. Wood DL, Sawicki GS, Miller MD, et al. The Transition Readiness Assessment Questionnaire (TRAQ): its factor structure, reliability, and validity. Acad Pediatr. 2014; 14:415–422.
Article74. Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A socialecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011; 37:883–895.
Article75. Gilleland J, Amaral S, Mee L, Blount R. Getting ready to leave: transition readiness in adolescent kidney transplant recipients. J Pediatr Psychol. 2012; 37:85–96.
Article76. Ferris ME, Harward DH, Bickford K, et al. A clinical tool to measure the components of health-care transition from pediatric care to adult care: the UNC TR(x)ANSITION scale. Ren Fail. 2012; 34:744–753.
Article77. Benchimol EI, Walters TD, Kaufman M, et al. Assessment of knowledge in adolescents with inflammatory bowel disease using a novel transition tool. Inflamm Bowel Dis. 2011; 17:1131–1137.
Article78. Fishman LN, Houtman D, van Groningen J, Arnold J, Ziniel S. Medication knowledge: an initial step in self-management for youth with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2011; 53:641–645.79. Izaguirre MR, Keefer L. Development of a self-efficacy scale for adolescents and young adults with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2014; 59:29–32.
Article80. Yerushalmy-Feler A, Ron Y, Barnea E, et al. Adolescent transition clinic in inflammatory bowel disease: quantitative assessment of self-efficacy skills. Eur J Gastroenterol Hepatol. 2017; 29:831–837.81. Izaguirre MR, Taft T, Keefer L. Validation of a self-efficacy scale for adolescents and young adults with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2017; 65:546–550.
Article82. Brooks AJ, Smith PJ, Lindsay JO. Monitoring adolescents and young people with inflammatory bowel disease during transition to adult healthcare. Frontline Gastroenterol. 2018; 9:37–44.
Article83. Greenley RN, Stephens M, Doughty A, Raboin T, Kugathasan S. Barriers to adherence among adolescents with inflammatory bowel disease. Inflamm Bowel Dis. 2010; 16:36–41.
Article84. Hommel KA, Davis CM, Baldassano RN. Objective versus subjective assessment of oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2009; 15:589–593.
Article85. Hommel KA, Davis CM, Baldassano RN. Medication adherence and quality of life in pediatric inflammatory bowel disease. J Pediatr Psychol. 2008; 33:867–874.
Article86. Mackner LM, Crandall WV. Oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis. 2005; 11:1006–1012.
Article87. Oliva-Hemker MM, Abadom V, Cuffari C, Thompson RE. Nonadherence with thiopurine immunomodulator and mesalamine medications in children with Crohn disease. J Pediatr Gastroenterol Nutr. 2007; 44:180–184.
Article88. Paine CW, Stollon NB, Lucas MS, et al. Barriers and facilitators to successful transition from pediatric to adult inflammatory bowel disease care from the perspectives of providers. Inflamm Bowel Dis. 2014; 20:2083–2091.
Article89. Bennett AL, Moore D, Bampton PA, Bryant RV, Andrews JM. Outcomes and patients’ perspectives of transition from paediatric to adult care in inflammatory bowel disease. World J Gastroenterol. 2016; 22:2611–2620.
Article90. Jeganathan J, Lee CH, Rahme A, et al. Pediatric-to-adult transition and medication adherence in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2017; 23:1065–1070.
Article91. Dabadie A, Troadec F, Heresbach D, Siproudhis L, Pagenault M, Bretagne JF. Transition of patients with inflammatory bowel disease from pediatric to adult care. Gastroenterol Clin Biol. 2008; 32:451–459.
Article92. Fu N, Jacobson K, Round A, Evans K, Qian H, Bressler B. Transition clinic attendance is associated with improved beliefs and attitudes toward medicine in patients with inflammatory bowel disease. World J Gastroenterol. 2017; 23:5405–5411.
Article93. Cole R, Ashok D, Razack A, Azaz A, Sebastian S. Evaluation of outcomes in adolescent inflammatory bowel disease patients following transfer from pediatric to adult health care services: case for transition. J Adolesc Health. 2015; 57:212–217.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Transition from Pediatric to Adult Care in Inflammatory Bowel Disease: What is the Key?
- How Can We Do Transition Successfully from Pediatric to Adult Clinics in Inflammatory Bowel Disease?
- Pediatric to adult inflammatory bowel disease transition: the Asian experience
- Characteristics and Treatment Outcomes of Transition among Patients with Inflammatory Bowel Disease
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence