Cancer Res Treat.
2019 Jan;51(1):34-42. 10.4143/crt.2017.551.
The Characteristics and Survival Outcomes in Patients Aged 70 Years and Older with Nasopharyngeal Carcinoma in the Intensity-Modulated Radiotherapy Era
- Affiliations
-
- 1State Key Laboratory of Oncology in Southern China, Collaborative Innovation Center of Cancer Medicine, Department of Nasopharyngeal Carcinoma, Sun Yat-sen University Cancer Center, Guangzhou, China. mohy@sysucc.org.cn luodh@sysucc.org.cn
- 2Department of Medical Statistics and Epidemiology and Health Information Research Center and Guangdong Key Laboratory of Medicine, School of Public Health, Sun Yat-sen University, Guangzhou, China.
- 3State Key Laboratory of Oncology in Southern China, Collaborative Innovation Center of Cancer Medicine, Department of VIP Region, Sun Yat-sen University Cancer Center, Guangzhou, China.
- 4Department of Medical Records Statistics, the Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, China.
- 5Department of Radiation Oncology, the Fifth Affiliated Hospital of Sun Yat-sen University, Zhuhai, China.
- KMID: 2437596
- DOI: http://doi.org/10.4143/crt.2017.551
Abstract
- PURPOSE
We aim to examine nasopharyngeal carcinoma (NPC) characteristics and survival outcomes in patients aged 70 years and older in the intensity-modulated radiotherapy (IMRT) era.
MATERIALS AND METHODS
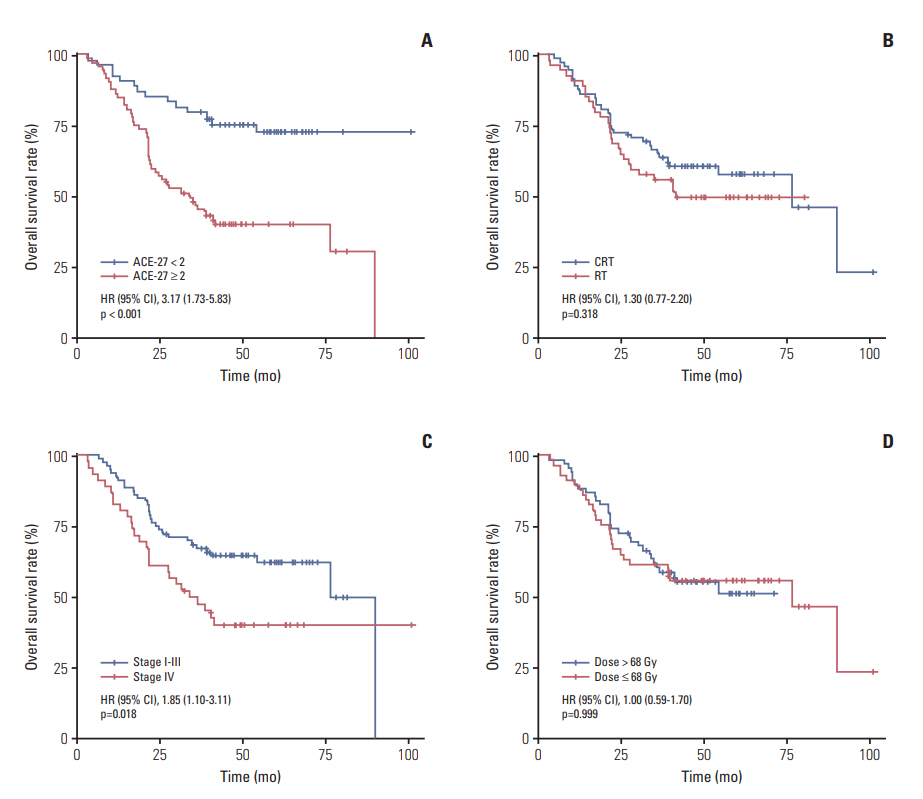
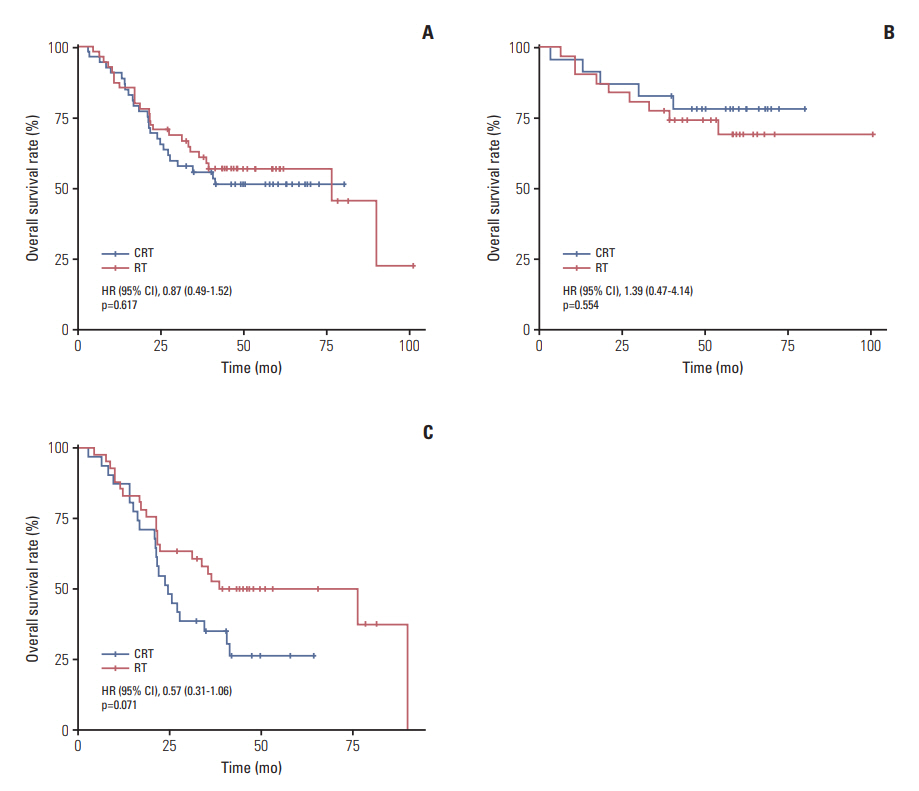
From 2006 to 2013, 126 non-metastatic NPC patients aged ≥ 70 years who were treated with IMRT +/"’ chemotherapy were included. Adult Comorbidity Evaluation 27 (ACE-27) was used to measure patient comorbidities. The overall survival (OS) and cancer-specific survival (CSS)were calculatedwith the Kaplan-Meier method, and differenceswere compared using the log-rank test. The Cox proportional hazards model was used to carry out multivariate analyses.
RESULTS
For the entire group, only two patients (1.6%) presented stage I disease, and up to 84.1% patients had stage III-IVB disease. All patients had a comorbidity score of 0 in 24 (19.0%), 1 in 45 (35.7%), 2 in 42 (33.3%), and 3 in 15 (11.9%) patients. The main acute grade during radiotherapy was 3-4 adverse events consisting of mucositis (25.4%), bone marrow suppression (16.7%), and dermatitis (8.7%). After treatment, four patients (3.2%) developed temporal lobe injury. Five-year CSS and OS rates were 67.3% (95% confidence interval [CI], 58.6% to 77.4%) and 54.0% (95% CI, 45.6% to 63.9%), respectively. Five-year OS was significantly higher for ACE-27 score 0-1 than ACE-27 score 2-3 (72.9% and 39.9%, respectively; p < 0.001). Multivariate analyses showed ACE-27 score 0-1 was significantly associated with superior OS (hazard ratio [HR], 3.02; 95% CI, 1.64 to 5.55; p < 0.001). In addition, the rate of OS was higher for stage I-III than that of stage IV, with borderline significance (HR, 1.67; 95% CI, 0.99 to 2.82; p=0.053). But no significant advantage was observed in OS when chemotherapy was used (p > 0.05).
CONCLUSION
Our findings suggest IMRT +/- chemotherapy has a manageable toxicity and provides an acceptable survival in patients aged ≥ 70 years with NPC. ACE-27 score was significantly associated with survival outcomes in this group population.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Development and Validation of Web-Based Nomograms to Precisely Predict Survival Outcomes of Non-metastatic Nasopharyngeal Carcinoma in an Endemic Area
Ji-Jin Yao, Li Lin, Tian-Sheng Gao, Wang-Jian Zhang, Wayne R. Lawrence, Jun Ma, Ying Sun
Cancer Res Treat. 2021;53(3):657-670. doi: 10.4143/crt.2020.899.
Reference
-
References
1. Chua ML, Wee JT, Hui EP, Chan AT. Nasopharyngeal carcinoma. Lancet. 2016; 387:1012–24.
Article2. Zhang LF, Li YH, Xie SH, Ling W, Chen SH, Liu Q, et al. Incidence trend of nasopharyngeal carcinoma from 1987 to 2011 in Sihui County, Guangdong Province, South China: an ageperiod-cohort analysis. Chin J Cancer. 2015; 34:350–7.
Article3. United Nations. World population prospects: the 2010 revision. New York: United Nations;2011.4. Hui EP, Ma BB, Leung SF, King AD, Mo F, Kam MK, et al. Randomized phase II trial of concurrent cisplatin-radiotherapy with or without neoadjuvant docetaxel and cisplatin in advanced nasopharyngeal carcinoma. J Clin Oncol. 2009; 27:242–9.
Article5. Chen L, Hu CS, Chen XZ, Hu GQ, Cheng ZB, Sun Y, et al. Concurrent chemoradiotherapy plus adjuvant chemotherapy versus concurrent chemoradiotherapy alone in patients with locoregionally advanced nasopharyngeal carcinoma: a phase 3 multicentre randomised controlled trial. Lancet Oncol. 2012; 13:163–71.
Article6. Liu H, Chen QY, Guo L, Tang LQ, Mo HY, Zhong ZL, et al. Feasibility and efficacy of chemoradiotherapy for elderly patients with locoregionally advanced nasopharyngeal carcinoma: results from a matched cohort analysis. Radiat Oncol. 2013; 8:70.
Article7. Zeng Q, Xiang YQ, Wu PH, Lv X, Qian CN, Guo X. A matched cohort study of standard chemo-radiotherapy versus radiotherapy alone in elderly nasopharyngeal carcinoma patients. PLoS One. 2015; 10:e0119593.
Article8. Zhang Y, Yi JL, Huang XD, Xu GZ, Xiao JP, Li SY, et al. Inherently poor survival of elderly patients with nasopharyngeal carcinoma. Head Neck. 2015; 37:771–6.
Article9. Sze HC, Ng WT, Chan OS, Shum TC, Chan LL, Lee AW. Radical radiotherapy for nasopharyngeal carcinoma in elderly patients: the importance of co-morbidity assessment. Oral Oncol. 2012; 48:162–7.
Article10. Xiao G, Cao Y, Qiu X, Wang W, Wang Y. Influence of gender and age on the survival of patients with nasopharyngeal carcinoma. BMC Cancer. 2013; 13:226.
Article11. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–4.
Article12. Piccirillo JF. Importance of comorbidity in head and neck cancer. Laryngoscope. 2000; 110:593–602.
Article13. Lai SZ, Li WF, Chen L, Luo W, Chen YY, Liu LZ, et al. How does intensity-modulated radiotherapy versus conventional two-dimensional radiotherapy influence the treatment results in nasopharyngeal carcinoma patients? Int J Radiat Oncol Biol Phys. 2011; 80:661–8.14. ICRU report. Prescribing, recording, and reporting photon beam therapy (Report 62). Bethesda, MD: International Commission on Radiation Units and Measurements;1999.15. ICRU report. Prescribing, recording, and reporting photonbeam intensity-modulated radiation therapy (IMRT) (Vol. 83). . Bethesda, MD: International Commission on Radiation Units and Measurements;2010.16. Wang YX, King AD, Zhou H, Leung SF, Abrigo J, Chan YL, et al. Evolution of radiation-induced brain injury: MR imagingbased study. Radiology. 2010; 254:210–8.
Article17. Guo R, Sun Y, Yu XL, Yin WJ, Li WF, Chen YY, et al. Is primary tumor volume still a prognostic factor in intensity modulated radiation therapy for nasopharyngeal carcinoma? Radiother Oncol. 2012; 104:294–9.
Article18. Li WF, Sun Y, Chen M, Tang LL, Liu LZ, Mao YP, et al. Locoregional extension patterns of nasopharyngeal carcinoma and suggestions for clinical target volume delineation. Chin J Cancer. 2012; 31:579–87.
Article19. Yi JL, Gao L, Huang XD, Li SY, Luo JW, Cai WM, et al. Nasopharyngeal carcinoma treated by radical radiotherapy alone: ten-year experience of a single institution. Int J Radiat Oncol Biol Phys. 2006; 65:161–8.
Article20. Zhang MX, Li J, Shen GP, Zou X, Xu JJ, Jiang R, et al. Intensity-modulated radiotherapy prolongs the survival of patients with nasopharyngeal carcinoma compared with conventional two-dimensional radiotherapy: a 10-year experience with a large cohort and long follow-up. Eur J Cancer. 2015; 51:2587–95.
Article21. Peng G, Wang T, Yang KY, Zhang S, Zhang T, Li Q, et al. A prospective, randomized study comparing outcomes and toxicities of intensity-modulated radiotherapy vs. conventional two-dimensional radiotherapy for the treatment of nasopharyngeal carcinoma. Radiother Oncol. 2012; 104:286–93.
Article22. Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL Jr. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004; 291:2441–7.
Article23. Rogers SN, Aziz A, Lowe D, Husband DJ. Feasibility study of the retrospective use of the Adult Comorbidity Evaluation index (ACE-27) in patients with cancer of the head and neck who had radiotherapy. Br J Oral Maxillofac Surg. 2006; 44:283–8.
Article24. Paleri V, Wight RG, Davies GR. Impact of comorbidity on the outcome of laryngeal squamous cancer. Head Neck. 2003; 25:1019–26.
Article25. Ramakrishnan Y, Paleri V, Shah R, Steen IN, Wight RG, Kelly CG. Comorbidity in nasopharyngeal carcinoma: a preliminary communication on the prevalence, descriptive distribution and impact on outcome. Clin Otolaryngol. 2007; 32:484–8.
Article26. Lee AW, Foo W, Law SC, Poon YF, Sze WM, O SK, et al. Nasopharyngeal carcinoma: presenting symptoms and duration before diagnosis. Hong Kong Med J. 1997; 3:355–61.27. Cheung MC, Chan AS, Law SC, Chan JH, Tse VK. Impact of radionecrosis on cognitive dysfunction in patients after radiotherapy for nasopharyngeal carcinoma. Cancer. 2003; 97:2019–26.
Article28. Zhou GQ, Yu XL, Chen M, Guo R, Lei Y, Sun Y, et al. Radiation-induced temporal lobe injury for nasopharyngeal carcinoma: a comparison of intensity-modulated radiotherapy and conventional two-dimensional radiotherapy. PLoS One. 2013; 8:e67488.
Article29. Zeng L, Tian YM, Sun XM, Chen CY, Han F, Xiao WW, et al. Late toxicities after intensity-modulated radiotherapy for nasopharyngeal carcinoma: patient and treatment-related risk factors. Br J Cancer. 2014; 110:49–54.
Article30. Kong C, Zhu XZ, Lee TF, Feng PB, Xu JH, Qian PD, et al. LASSO-based NTCP model for radiation-induced temporal lobe injury developing after intensity-modulated radiotherapy of nasopharyngeal carcinoma. Sci Rep. 2016; 6:26378.
Article31. Bortolin MT, Pratesi C, Dolcetti R, Bidoli E, Vaccher E, Zanussi S, et al. Clinical value of Epstein-Barr virus DNA levels in peripheral blood samples of Italian patients with undifferentiated carcinoma of nasopharyngeal type. Cancer Lett. 2006; 233:247–54.
Article32. Lin JC, Wang WY, Liang WM, Chou HY, Jan JS, Jiang RS, et al. Long-term prognostic effects of plasma epstein-barr virus DNA by minor groove binder-probe real-time quantitative PCR on nasopharyngeal carcinoma patients receiving concurrent chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2007; 68:1342–8.
Article33. Tang LQ, Chen QY, Guo SS, Chen WH, Li CF, Zhang L, et al. The impact of plasma Epstein-Barr virus DNA and fibrinogen on nasopharyngeal carcinoma prognosis: an observational study. Br J Cancer. 2014; 111:1102–11.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Value and Staging Classification of Lymph Nodal Necrosis in Nasopharyngeal Carcinoma after Intensity-Modulated Radiotherapy
- Locoregionally advanced nasopharyngeal carcinoma treated with intensity-modulated radiotherapy plus concurrent weekly cisplatin with or without neoadjuvant chemotherapy
- Paranasal Sinus Invasion in Nasopharyngeal Carcinoma after Intensity-Modulated Radiotherapy
- Is the Use of Intensity-Modulated Radiotherapy Beneficial for Pancreatic Cancer Patients?
- Magnetic Resonance Imaging–Detected Intracranial Extension in the T4 Classification Nasopharyngeal Carcinoma with Intensity-Modulated Radiotherapy