Acute Crit Care.
2018 May;33(2):73-82. 10.4266/acc.2017.00591.
Current Status and Survival Impact of Infectious Disease Consultation for Multidrug-Resistant Bacteremia in Ventilated Patients: A Single-Center Experience in Korea
- Affiliations
-
- 1Division of Pulmonary, Allergy and Critical Care Medicine, Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. jubilate@pusan.ac.kr
- KMID: 2436314
- DOI: http://doi.org/10.4266/acc.2017.00591
Abstract
- BACKGROUND
We evaluated the current status and survival impact of infectious disease consultation (IDC) in ventilated patients with multidrug-resistant (MDR) bacteremia.
METHODS
One hundred sixty-one consecutive patients from a single tertiary care hospital were enrolled over a 5-year period. Patients with at least one of the following six MDR bacteremias were included: methicillin-resistant Staphylococcus aureus, extended-spectrum β-lactamase-producing gram-negative bacteria (Escherichia coli and Klebsiella pneumonia), carbapenem-resistant gram-negative rods (Acinetobacter baumannii and Pseudomonas aeruginosa), and vancomycin-resistant Enterococcus faecium.
RESULTS
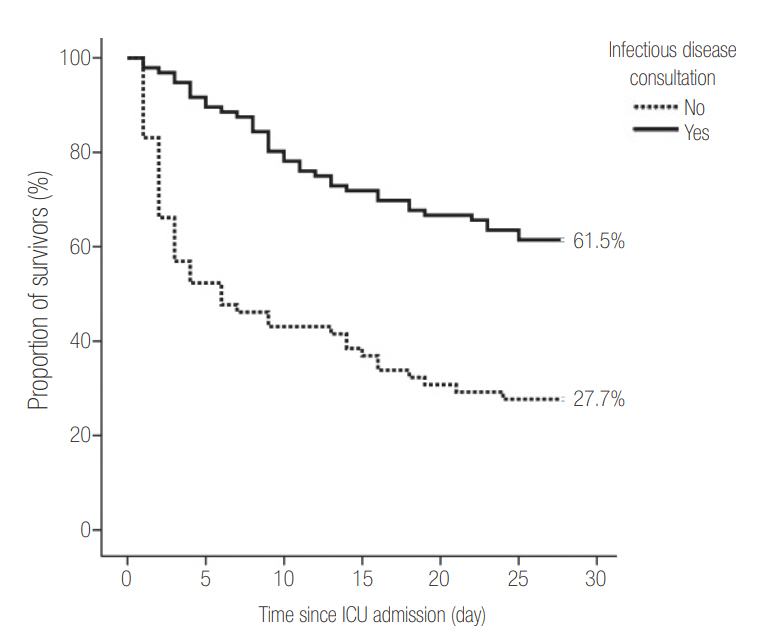
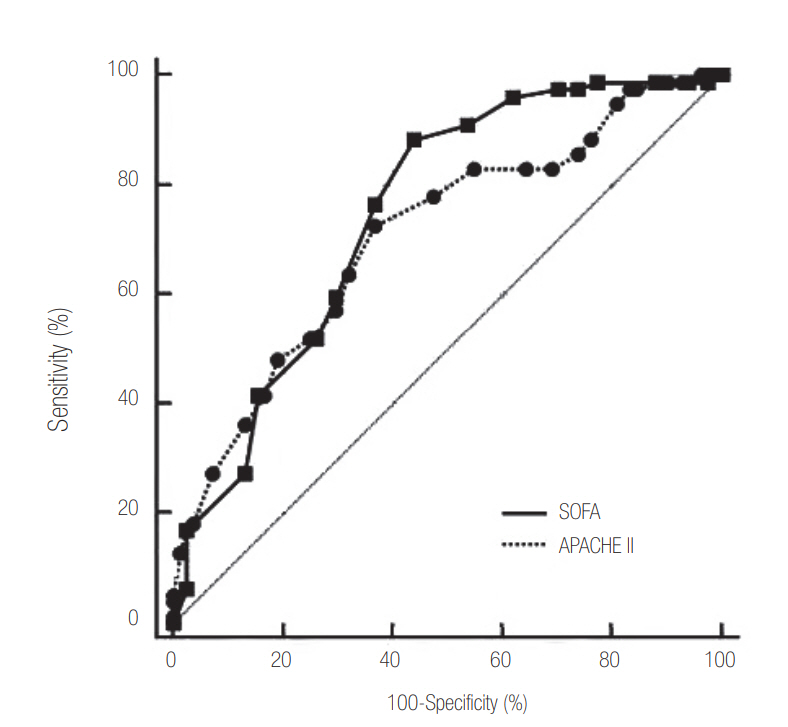
Median patient age was 66 years (range, 18 to 95), and 57.8% of subjects were male. The 28-day mortality after the day of blood culture was 52.2%. An IDC was requested for 96 patients based on a positive blood culture (59.6%). Patients without IDC had significantly higher rate of hemato-oncologic diseases as a comorbidity (36.9% vs. 11.5%, P < 0.001). Patients without an IDC had higher Acute Physiology and Chronic Health Evaluation (APACHE) II score (median, 20; range, 8 to 38 vs. median, 16; range, 5 to 34, P < 0.001) and Sequential Organ Failure Assessment (SOFA) score (median, 9; range, 2 to 17 vs. median, 7; range, 2 to 20; P = 0.020) on the day of blood culture and a higher 28-day mortality rate (72.3% vs. 38.5%, P < 0.001). In patients with SOFA ≥9 (cut-off level based on Youden's index) on the day of blood culture and gram-negative bacteremia, IDC was also significantly associated with lower 28-day mortality (hazard ratio [HR], 0.298; 95% confidence interval [CI], 0.167 to 0.532 and HR, 0.180; 95% CI, 0.097 to 0.333; all P ≥ 0.001) based on multivariate Cox regression analysis.
CONCLUSIONS
An IDC for MDR bacteremia was requested less often for ventilated patients with greater disease severity and higher 28-day mortality after blood was drawn. In patients with SOFA ≥9 on the day of blood culture and gram-negative bacteremia, IDC was associated with improved 28-day survival after blood draw for culture.
MeSH Terms
Figure
Reference
-
1. Brusselaers N, Vogelaers D, Blot S. The rising problem of antimicrobial resistance in the intensive care unit. Ann Intensive Care. 2011; 1:47.
Article2. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18:268–81.
Article3. Vardakas KZ, Rafailidis PI, Konstantelias AA, Falagas ME. Predictors of mortality in patients with infections due to multi-drug resistant Gram negative bacteria: the study, the patient, the bug or the drug? J Infect. 2013; 66:401–14.
Article4. Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014; 370:1198–208.
Article5. Levy Hara G, Kanj SS, Pagani L, Abbo L, Endimiani A, Wertheim HF, et al. Ten key points for the appropriate use of antibiotics in hospitalised patients: a consensus from the Antimicrobial Stewardship and Resistance Working Groups of the International Society of Chemotherapy. Int J Antimicrob Agents. 2016; 48:239–46.
Article6. Levy-Hara G, Amábile-Cuevas CF, Gould I, Hutchinson J, Abbo L, Saxynger L, et al. “Ten commandments” for the appropriate use of antibiotics by the practicing physician in an outpatient setting. Front Microbiol. 2011; 2:230.
Article7. Pulcini C, Defres S, Aggarwal I, Nathwani D, Davey P. Design of a ‘day 3 bundle’ to improve the reassessment of inpatient empirical antibiotic prescriptions. J Antimicrob Chemother. 2008; 61:1384–8.
Article8. Pulcini C, Botelho-Nevers E, Dyar OJ, Harbarth S. The impact of infectious disease specialists on antibiotic prescribing in hospitals. Clin Microbiol Infect. 2014; 20:963–72.
Article9. Schmitt S, McQuillen DP, Nahass R, Martinelli L, Rubin M, Schwebke K, et al. Infectious diseases specialty intervention is associated with decreased mortality and lower healthcare costs. Clin Infect Dis. 2014; 58:22–8.
Article10. Kim JH, Hong SK, Kim KC, Lee MG, Lee KM, Jung SS, et al. Influence of full-time intensivist and the nurse-to-patient ratio on the implementation of severe sepsis bundles in Korean intensive care units. J Crit Care. 2012; 27:414. e11-21.
Article11. Kwak SH, Jeong CW, Lee SH, Lee HJ, Koh Y. Current status of intensive care units registered as critical care subspecialty training hospitals in Korea. J Korean Med Sci. 2014; 29:431–7.
Article12. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013; 39:165–228.
Article13. Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–8.
Article14. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985; 13:818–29.15. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996; 22:707–10.
Article16. Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006; 163:670–5.
Article17. Turner RB, Valcarlos E, Won R, Chang E, Schwartz J. Impact of infectious diseases consultation on clinical outcomes of patients with Staphylococcus aureus bacteremia in a community health system. Antimicrob Agents Chemother. 2016; 60:5682–7.
Article18. Bai AD, Showler A, Burry L, Steinberg M, Ricciuto DR, Fernandes T, et al. Impact of infectious disease consultation on quality of care, mortality, and length of stay in Staphylococcus aureus bacteremia: results from a large multicenter cohort study. Clin Infect Dis. 2015; 60:1451–61.
Article19. Tedeschi S, Trapani F, Giannella M, Cristini F, Tumietto F, Bartoletti M, et al. An antimicrobial stewardship program based on systematic infectious disease consultation in a rehabilitation facility. Infect Control Hosp Epidemiol. 2017; 38:76–82.
Article20. Hamandi B, Husain S, Humar A, Papadimitropoulos EA. Impact of infectious disease consultation on the clinical and economic outcomes of solid organ transplant recipients admitted for infectious complications. Clin Infect Dis. 2014; 59:1074–82.
Article21. Choi SH, Cho SY, Park JH, Chung JW. Impact of infectious-disease specialist consultations on outcomes of Staphylococcus aureus bacteremia in a hospital with a low volume of patients with S. aureus bacteremia. J Infect. 2011; 62:181–5.
Article22. Howard P, Pulcini C, Levy Hara G, West RM, Gould IM, Harbarth S, et al. An international cross-sectional survey of antimicrobial stewardship programmes in hospitals. J Antimicrob Chemother. 2015; 70:1245–55.
Article23. Holloway KA, Rosella L, Henry D. The Impact of WHO essential medicines policies on inappropriate use of antibiotics. PLoS One. 2016; 11:e0152020.
Article24. Saunderson RB, Gouliouris T, Nickerson EK, Cartwright EJ, Kidney A, Aliyu SH, et al. Impact of routine bedside infectious disease consultation on clinical management and outcome of Staphylococcus aureus bacteraemia in adults. Clin Microbiol Infect. 2015; 21:779–85.25. Robinson JO, Pozzi-Langhi S, Phillips M, Pearson JC, Christiansen KJ, Coombs GW, et al. Formal infectious diseases consultation is associated with decreased mortality in Staphylococcus aureus bacteraemia. Eur J Clin Microbiol Infect Dis. 2012; 31:2421–8.
Article26. Fries BL, Licitra C, Crespo A, Akhter K, Busowski MT, Salazar D, et al. Infectious diseases consultation and the management of Staphylococcus aureus bacteremia. Clin Infect Dis. 2014; 58:598–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sequential Organ Failure Assessment score as a predictor of mortality in ventilated patients with multidrug-resistant bacteremia
- Current status of multidrug-resistant bacteria
- Communication of Infectious Diseases Consultant
- Multidrug-resistant bacteria: a national challenge requiring urgent addressal
- Effects of Cessation of Single-Room Isolation on Transmission of Vancomycin-Resistant Enterococcus in a Hospital