Anesth Pain Med.
2018 Oct;13(4):419-422. 10.17085/apm.2018.13.4.419.
Anesthetic management of a chronic liver disease patient with very low platelet counts by considering a rebalanced hemostasis: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. gskim@skku.edu
- KMID: 2436002
- DOI: http://doi.org/10.17085/apm.2018.13.4.419
Abstract
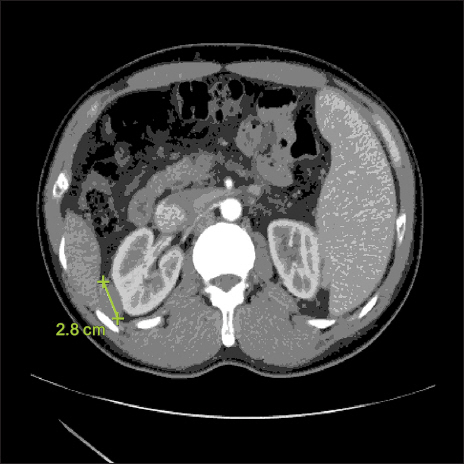
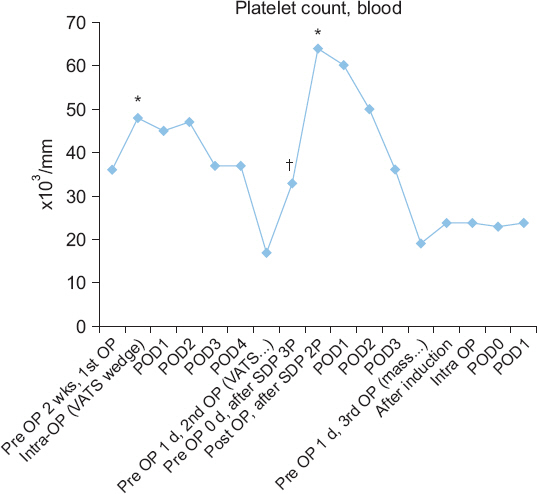
- The coagulation profile of patients with end-stage liver disease (ESLD) is different from that of healthy individuals. Because hemostasis is rebalanced in chronic liver disease, prophylactic transfusion of blood products may be not necessary for these patients even if they show severe coagulation dysfunction in conventional coagulation results. A 44-year-old man with hepatocellular carcinoma, cholangiocarcinoma and liver cirrhosis was scheduled for extra-hepatic mass excision under general anesthesia. His preoperative tests showed severe thrombocytopenia 19 × 10â¹/L. The patient underwent extrahepatic mass excision surgery under general anesthesia without transfusion of blood products. The post-operative course was uneventful without requiring any further hemostatic therapy. In this case report, we focus on the concept of rebalanced hemostasis in ESLD, and coagulation management based on rotational thromboelastometry.
Keyword
MeSH Terms
Figure
Reference
-
REFERENCE
1. Shah NL, Northup PG, Caldwell SH. A clinical survey of bleeding, thrombosis, and blood product use in decompensated cirrhosis patients. Ann Hepatol. 2012; 11:686–90. PMID: 22947530.2. Shah NL, Caldwell SH. Assessing the risk of bleeding and clotting in cirrhosis. Clin Liver Dis. 2016; 7:26–8. DOI: 10.1002/cld.528.3. Lisman T, Porte RJ. Rebalanced hemostasis in patients with liver disease:evidence and clinical consequences. Blood. 2010; 116:878–85. DOI: 10.1182/blood-2010-02-261891. PMID: 20400681.4. Henry Z, Northup PG. The rebalanced hemostasis system in end-stage liver disease and its impact on liver transplantation. Int Anesthesiol Clin. 2017; 55:107–20. DOI: 10.1097/AIA.0000000000000139. PMID: 28221169.5. Lisman T, Leebeek FW, Mosnier LO, Bouma BN, Meijers JC, Janssen HL, et al. Thrombin-activatable fibrinolysis inhibitor deficiency in cirrhosis is not associated with increased plasma fibrinolysis. Gastroenterology. 2001; 121:131–9. DOI: 10.1053/gast.2001.25481. PMID: 11438502.6. Weeder PD, Porte RJ, Lisman T. Hemostasis in liver disease:implications of new concepts for perioperative management. Transfus Med Rev. 2014; 28:107–13. DOI: 10.1016/j.tmrv.2014.03.002. PMID: 24721432.7. Ganter MT, Hofer CK. Coagulation monitoring:current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth Analg. 2008; 106:1366–75. DOI: 10.1213/ane.0b013e318168b367. PMID: 18420846.8. Hartmann M, Szalai C, Saner FH. Hemostasis in liver transplantation:pathophysiology, monitoring, and treatment. World J Gastroenterol. 2016; 22:1541–50. DOI: 10.3748/wjg.v22.i4.1541. PMID: 26819521. PMCID: PMC4721987.9. Kim TY. Perioperative bleeding disorder and intraoperative ponit-of-care testing of coagulation during cardiac surgery. Anesth Pain Med. 2011; 6:1–15.10. Kaufman RM, Djulbegovic B, Gernsheimer T, Kleinman S, Tinmouth AT, Capocelli KE, et al. Platelet transfusion:a clinical practice guideline from the AABB. Ann Intern Med. 2015; 162:205–13. DOI: 10.7326/M14-1589. PMID: 25383671.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver transplantation of a patient with extreme thrombocytopenia - A case report -
- Anesthetic Management of a Patient with Postpartum HELLP Syndrome: A case report
- Gastric Submucosal Hematoma after Endoscopic Hemostasis in Patient with Dual Antiplatelet Therapy
- Anticoagulation in cirrhosis: a new paradigm?
- Anesthetic Management of a Patient with Glanzmann's Thrombasthenia: A case report