Anesth Pain Med.
2018 Oct;13(4):383-387. 10.17085/apm.2018.13.4.383.
Awake fiberoptic orotracheal intubation using a modified Guedel airway in a patient with craniocervical instability and an anticipated difficult airway: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Korea Cancer Center Hospital, Seoul, Korea. jiheui0255@naver.com
- KMID: 2435995
- DOI: http://doi.org/10.17085/apm.2018.13.4.383
Abstract
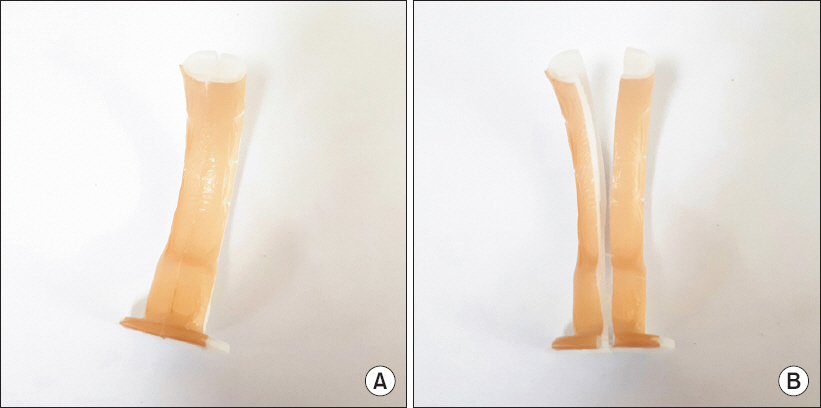
- In patients with upper cervical instability, airway management may provoke subluxation of the craniocervical region and neurologic injury, and can be challenging for the anesthesiologist. Endotracheal intubation using a fiberoptic bronchoscope is frequently used in these patients to minimize spine motion, but this procedure may fail in patients with altered airway anatomy. When fiberoptic endotracheal intubation fails in these patients, optional intubation methods are limited. We describe successful awake fiberoptic orotracheal intubation using a modified Guedel airway divided in the midline for a 59-year-old man with an anticipated difficult airway, due to limited mouth opening, a nasopharyngeal tumor, and craniocervical spine instability after failure of conventional fiberoptic orotracheal intubation.
Keyword
MeSH Terms
Figure
Reference
-
REFERENCE
1. LeGrand SA, Hindman BJ, Dexter F, Weeks JB, Todd MM. Craniocervical motion during direct laryngoscopy and orotracheal intubation with the Macintosh and Miller blades:an in vivo cinefluoroscopic study. Anesthesiology. 2007; 107:884–91. DOI: 10.1097/01.anes.0000291461.62404.46. PMID: 18043056.2. Ezri T, Szmuk P, Evron S, Warters RD, Herman O, Weinbroum AA. Nasal versus oral fiberoptic intubation via a cuffed oropharyngeal airway (COPA) during spontaneous ventilation. J Clin Anesth. 2004; 16:503–7. DOI: 10.1016/j.jclinane.2004.01.006. PMID: 15590253.3. Greenland KB, Irwin MG. The Williams airway intubator, the Ovassapian airway and the Berman airway as upper airway conduits for fibreoptic bronchoscopy in patients with difficult airways. Curr Opin Anaesthesiol. 2004; 17:505–10. DOI: 10.1097/00001503-200412000-00010.4. Ajay S, Singhania A, Akkara AG, Shah A, Adalja M. A study of flexible fiberoptic bronchoscopy aided tracheal intubation for patients undergoing elective surgery under general anesthesia. Indian J Otolaryngol Head Neck Surg. 2013; 65:116–9. DOI: 10.1007/s12070-012-0576-8. PMID: 24427550. PMCID: PMC3649018.5. Cheng KI, Yun MK, Chang MC, Lee KW, Huang SC, Tang CS, et al. Fiberoptic bronchoscopic view change of laryngopharyngeal tissues by different airway supporting techniques:comparison of patients with and without open mouth limitation. J Clin Anesth. 2009; 20:573–9. DOI: 10.1016/j.jclinane.2008.01.013. PMID: 19100929.6. Wahlen BM, Gercek E. Three-dimensional cervical spine movement during intubation using the Macintosh and Bullard laryngoscopes, the bonfils fibrescope and the intubating laryngeal mask airway. Eur J Anaesthesiol. 2004; 21:907–13. DOI: 10.1097/00003643-200411000-00013.7. Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion:a fluoroscopic comparison during intubation with lighted stylet, Glidescope, and Macintosh laryngoscope. Anesth Analg. 2005; 101:910–5. DOI: 10.1213/01.ane.0000166975.38649.27. PMID: 16116013.8. Crosby ET. Airway management in adults after cervical spine trauma. Anesthesiology. 2006; 104:1293–318. DOI: 10.1097/00000542-200606000-00026. PMID: 16732102.9. Sawin PD, Todd MM, Traynelis VC, Farrell SB, Nader A, Sato Y, et al. Cervical spine motion with direct laryngoscopy and orotracheal intubation. An in vivo cinefluoroscopic study of subjects without cervical abnormality. Anesthesiology. 1996; 85:26–36. DOI: 10.1097/00000542-199607000-00005. PMID: 8694378.10. Brimacombe J, Keller C, Künzel KH, Gaber O, Boehler M, Pühringer F. Cervical spine motion during airway management:a cinefluoroscopic study of the posteriorly destabilized third cervical vertebrae in human cadavers. Anesth Analg. 2000; 91:1274–8. DOI: 10.1213/00000539-200011000-00041. PMID: 11049921.11. Sener EB, Sarihasan B, Ustun E, Kocamanoglu S, Kelsaka E, Tur A. Awake tracheal intubation through the intubating laryngeal mask airway in a patient with halo traction. Can J Anaesth. 2002; 49:610–3. DOI: 10.1007/BF03017390. PMID: 12067875.12. Prasarn ML, Conrad B, Rubery PT, Wendling A, Aydog T, Horodyski M, et al. Comparison of 4 airway devices on cervical spine alignment in a cadaver model with global ligamentous instability at C5-C6. Spine (Phila Pa 1976). 2012; 37:476–81. DOI: 10.1097/BRS.0b013e31822419fe. PMID: 21629162.13. Asai T, Shingu K. Difficulty in advancing a tracheal tube over a fiberoptic bronchoscope:incidence, causes and solutions. Br J Anaesth. 2004; 92:870–81. DOI: 10.1093/bja/aeh136. PMID: 15121723.14. Lee SK, Doo AR. Lee fiberoptic intubating airway for facilitating orotracheal fiberoptic intubation. Korean J Anesthesiol. 2013; 65:368–9. DOI: 10.4097/kjae.2013.65.4.368. PMID: 24228158. PMCID: PMC3822037.15. Varghese E, Nagaraj R, Shwethapriya R. Comparison of oral fiberoptic intubation via a modified guedel airway of a laryngeal mask airway in infants and children. J Anaesthesiol Clin Pharmacol. 2013; 29:52–5. DOI: 10.4103/0970-9185.105797. PMID: 23493291. PMCID: PMC3590542.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A fiberoptic orotracheal intubation successfully performed using a modified Guedel airway in a sedated emergency patient - A case report -
- Use of the Airtraq(R) optical laryngoscope as a rescue airway device following failed awake flexible fiberoptic nasotracheal intubation of a patient with severe microsomia: A case report
- Orotracheal intubation in a patient with difficult airway by using fiberoptic nasotracheal intubation: A case report
- The two stage flexible fiberoptic bronchoscoptic awake intubation in a patient with the symptomatic vallecular cyst: A case report
- Use of the Disposcope endoscope for awake orotracheal intubation in an elderly patient with a large vocal cord polyp -a case report-