J Neurocrit Care.
2018 Dec;11(2):102-109. 10.18700/jnc.180068.
Venous Thromboembolism Following Acute Ischemic Stroke: A Prospective Incidence Study
- Affiliations
-
- 1Department of Neurology, Jeju National University School of Medicine, Jeju, Korea. jaychoi@jejunu.ac.kr
- 2Department of Rehabilitation Medicine, Jeju National University School of Medicine, Jeju, Korea.
- 3Department of Radiology, Jeju National University School of Medicine, Jeju, Korea.
- KMID: 2434836
- DOI: http://doi.org/10.18700/jnc.180068
Abstract
- BACKGROUND
Asians were known to have a relatively lower incidence of venous thromboembolism (VTE), and there is insufficient evidence to suggest a specific D-dimer threshold level for screening VTE in patients with acute stroke.
METHODS
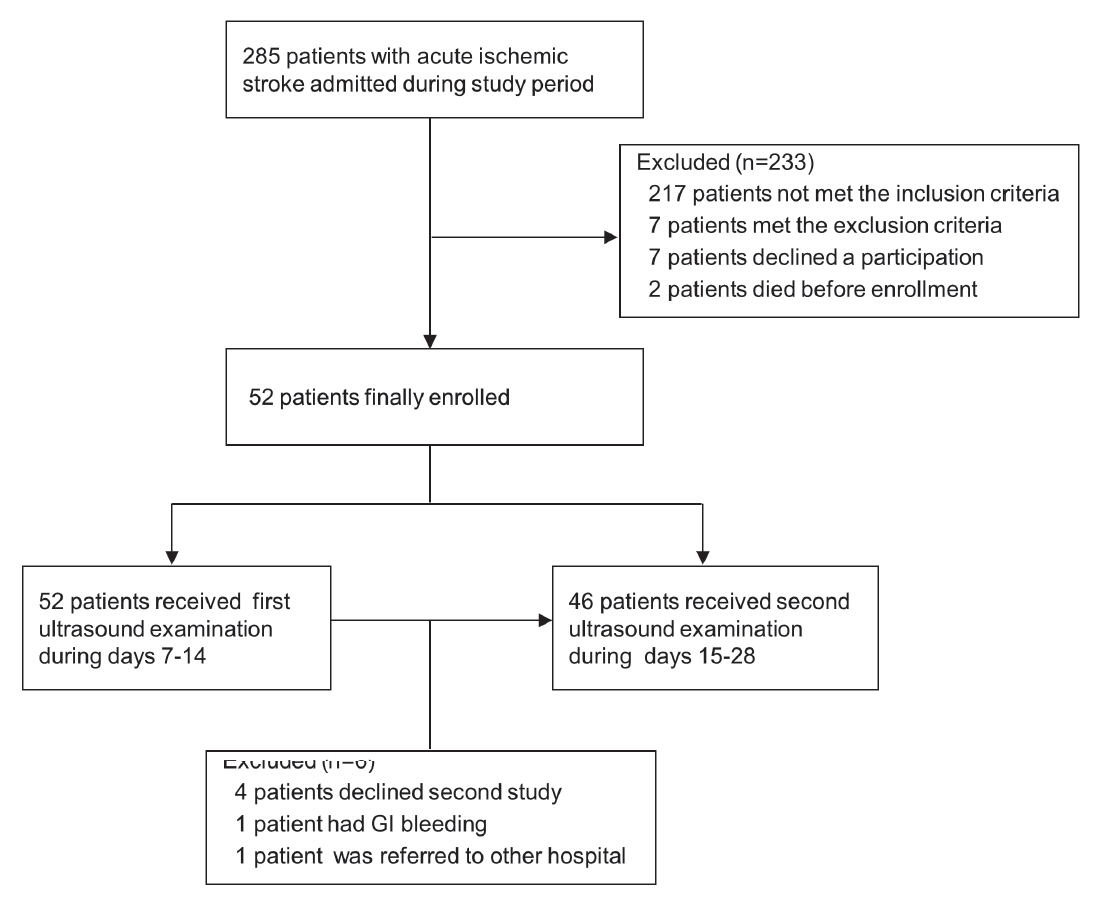
We prospectively enrolled patients with acute ischemic stroke admitted to Jeju National University Hospital. The inclusion criteria were: 1) aged ≥18 years, 2) admission within seven days of symptom onset, and 3) an initial National Institute of Health Stroke Scale (NIHSS) score >1 for the affected lower limb. Ultrasound scans of the lower limbs and plasma D-dimer assays were performed on days 7-14 and 15-28 after stroke onset.
RESULTS
Of 285 patients admitted during the study period, 52 patients met inclusion criteria (mean age 74.5, male 40.4%, median initial NIHSS score 12, and unable to walk unassisted at discharge 76.9%). During 7-14 days, 23 of 52 patients (44.2%) had a D-dimer level above 1.57 mg/L, and 9.6% had a level above 5.50 mg/L. Proximal deep vein thrombosis (DVT) was detected in 3 patients (5.8%, 95% confidence Interval 1.2-16.0%) on ultrasound examination. All DVTs were found in elderly female patients with severe leg weakness. No patient was diagnosed with pulmonary embolism during the study period.
CONCLUSION
The incidence of VTE seems to be very low among Korean patients with acute ischemic stroke. Advanced age, female sex, and severe leg weakness were important risk factors for developing DVT in this study.
Keyword
MeSH Terms
Figure
Reference
-
1. Brandstater ME, Roth EJ, Siebens HC. Venous thromboembolism in stroke: literature review and implications for clinical practice. Arch Phys Med Rehabil. 1992; 73(5-S):S379–91.2. Kelly J, Rudd A, Lewis R, Hunt BJ. Venous thromboembolism after acute stroke. Stroke. 2001; 32:262–7.
Article3. Kamphuisen PW, Agnelli G, Sebastianelli M. Prevention of venous thromboembolism after acute ischemic stroke. J Thromb Haemost. 2005; 3:1187–94.
Article4. Pongmoragot J, Rabinstein AA, Nilanont Y, Swartz RH, Zhou L, Saposnik G, et al. Pulmonary embolism in ischemic stroke: clinical presentation, risk factors, and outcome. J Am Heart Assoc. 2013; 2:e000372.
Article5. Bounds JV, Wiebers DO, Whisnant JP, Okazaki H. Mechanisms and timing of deaths from cerebral infarction. Stroke. 1981; 12:474–7.
Article6. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.7. Zakai NA, McClure LA. Racial differences in venous thromboembolism. J Thromb Haemost. 2011; 9:1877–82.
Article8. White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009; 123 Suppl 4:S11–7.
Article9. The Joint Commission. America’s hospitals: improving quality and safety. The joint commission’s annual report 2015 [online]. Available at: https://www.jointcommission.org/assets/1/18/TJC_Annual_Report_2015_EMBARGOED_11_9_15.pdf. Accessed at October 1, 2017.10. Zheng H, Liu L, Sun H, Wang X, Wang Y, Zhou Y, et al. Prophylaxis of deep venous thrombosis and adherence to guideline recommendations among inpatients with acute stroke: results from a multicenter observational longitudinal study in China. Neurol Res. 2008; 30:370–6.
Article11. Choi JC, Bae HJ, Lee SJ, Park JM, Park TH, Cho YJ, et al. Variation in prophylactic anticoagulation for venous thromboembolism among acute stroke patients. J Clin Neurosci. 2017; 45:330–1.
Article12. Stein PD, Hull RD, Patel KC, Olson RE, Ghali WA, Brant R, et al. D-dimer for the exclusion of acute venous thrombosis and pulmonary embolism: a systematic review. Ann Intern Med. 2004; 140:589–602.13. Balogun IO, Roberts LN, Patel R, Pathansali R, Kalra L, Arya R. Clinical and laboratory predictors of deep vein thrombosis after acute stroke. Thromb Res. 2016; 142:33–9.
Article14. Kuwashiro T, Toyoda K, Oyama N, Kawase K, Okazaki S, Nagano K, et al. High plasma D-dimer is a marker of deep vein thrombosis in acute stroke. J Stroke Cerebrovasc Dis. 2012; 21:205–9.
Article15. Guideline developed in collaboration with the American College of Radiology, Society of Pediatric Radiology, Society of Radiologists in Ultrasound. AIUM practice guideline for the performance of peripheral venous ultrasound examinations. J Ultrasound Med. 2015; 34:1–9.16. Wells PS, Anderson DR, Bormanis J, Guy F, Mitchell M, Gray L, et al. Value of assessment of pretest probability of deep-vein thrombosis in clinical management. Lancet. 1997; 350:1795–8.
Article17. Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis. N Engl J Med. 2003; 349:1227–35.
Article18. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015; 17:38–53.
Article19. Tan KS, Rashid AR, Tan CT. Venous thromboembolism in ischaemic stroke in Asia. Neurology Asia. 2008; 13:95–101.20. De Silva DA, Pey HB, Wong MC, Chang HM, Chen CP. Deep vein thrombosis following ischemic stroke among Asians. Cerebrovasc Dis. 2006; 22:245–50.
Article21. Tan SS, Venketasubramanian N, Ong PL, Lim TC. Early deep vein thrombosis: incidence in Asian stroke patients. Ann Acad Med Singapore. 2007; 36:815–20.22. Kong KH, Chua SG, Earnest A. Deep vein thrombosis in stroke patients admitted to a rehabilitation unit in Singapore. Int J Stroke. 2009; 4:175–9.
Article23. Angchaisuksiri P. Venous thromboembolism in Asia--an unrecognised and under-treated problem? Thromb Haemost. 2011; 106:585–90.24. Leizorovicz A, Turpie AG, Cohen AT, Wong L, Yoo MC, Dans A, et al. Epidemiology of venous thromboembolism in Asian patients undergoing major orthopedic surgery without thromboprophylaxis. The SMART study. J Thromb Haemost. 2005; 3:28–34.
Article25. Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, et al. Deepvein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005; 3:2664–70.
Article26. Liew NC, Alemany GV, Angchaisuksiri P, Bang SM, Choi G, DE Silva DA, et al. Asian venous thromboembolism guidelines: updated recommendations for the prevention of venous thromboembolism. Int Angiol. 2017; 36:1–20.
Article27. Harvey RL, Roth EJ, Yarnold PR, Durham JR, Green D. Deep vein thrombosis in stroke. The use of plasma D-dimer level as a screening test in the rehabilitation setting. Stroke. 1996; 27:1516–20.28. Akman MN, Cetin N, Bayramoglu M, Isiklar I, Kilinc S. Value of the D-dimer test in diagnosing deep vein thrombosis in rehabilitation inpatients. Arch Phys Med Rehabil. 2004; 85:1091–4.
Article29. Ageno W, Finazzi S, Steidl L, Biotti MG, Mera V, Melzi D’Eril G, et al. Plasma measurement of D-dimer levels for the early diagnosis of ischemic stroke subtypes. Arch Intern Med. 2002; 162:2589–93.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-Vitamin K Antagonist Oral Anticoagulants in Medical Conditions at High Risk of Thromboembolism beyond Atrial Fibrillation
- Do Statins Help Prevent VTE After Hemorrhagic Stroke During the Acute Period?
- Clinical Year in Review of Venous Thromboembolism
- Cerebrovascular complications during pregnancy and postpartum
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack