J Neurocrit Care.
2019 Jun;12(1):20-29. 10.18700/jnc.190087.
Cerebrovascular complications during pregnancy and postpartum
- Affiliations
-
- 1Department of Neurology, Brain Research Institue, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Republic of Korea. neurohong79@gmail.com
- KMID: 2452823
- DOI: http://doi.org/10.18700/jnc.190087
Abstract
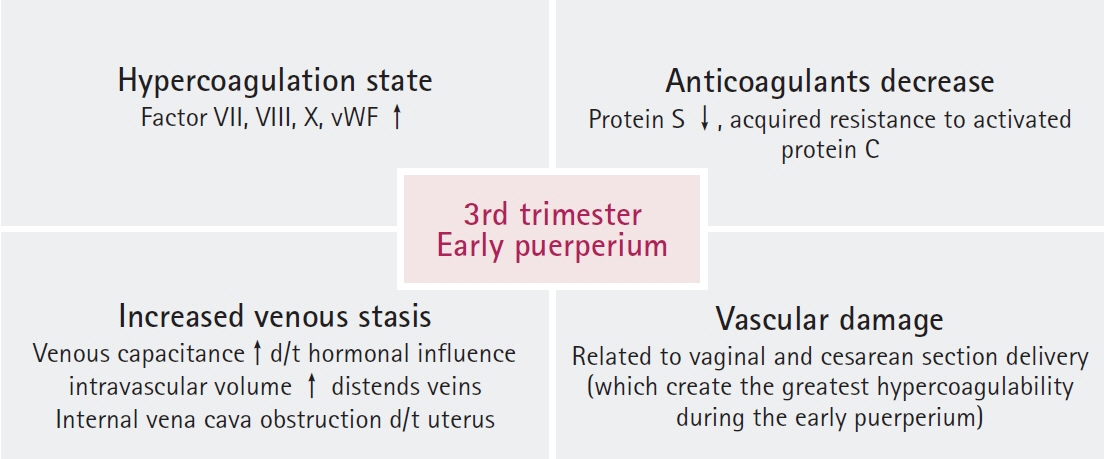
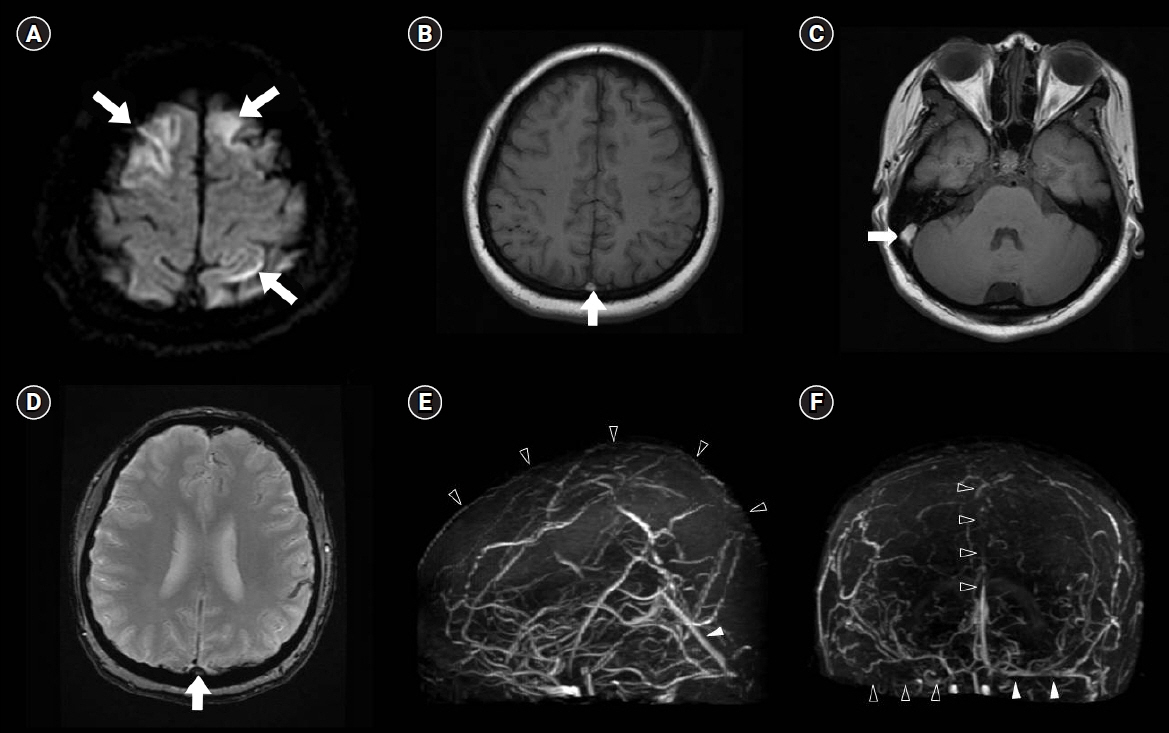
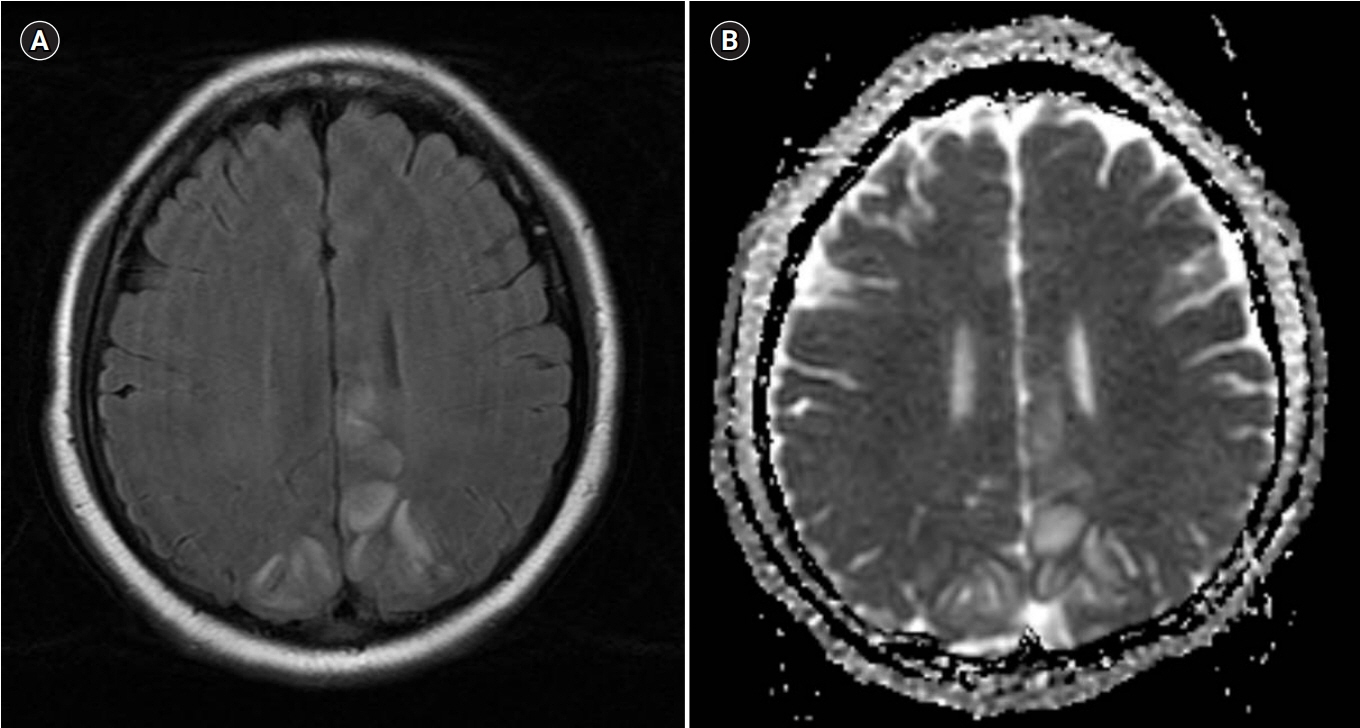
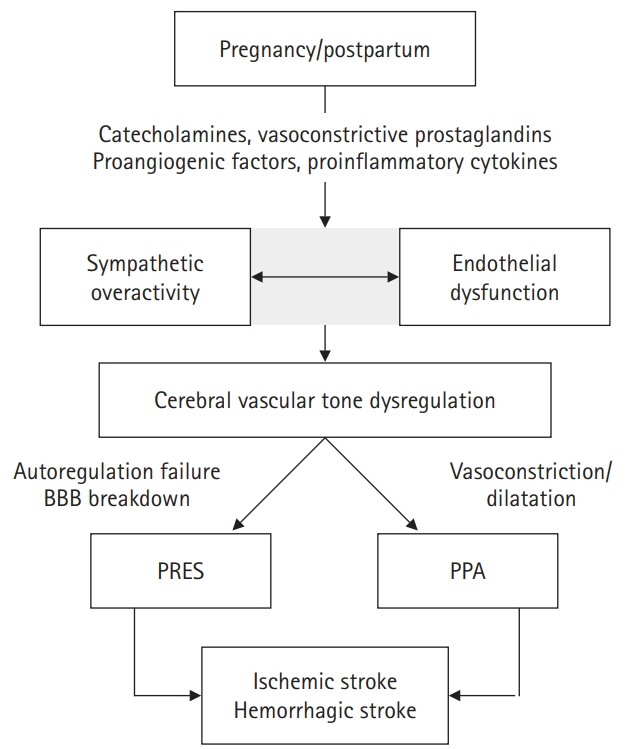
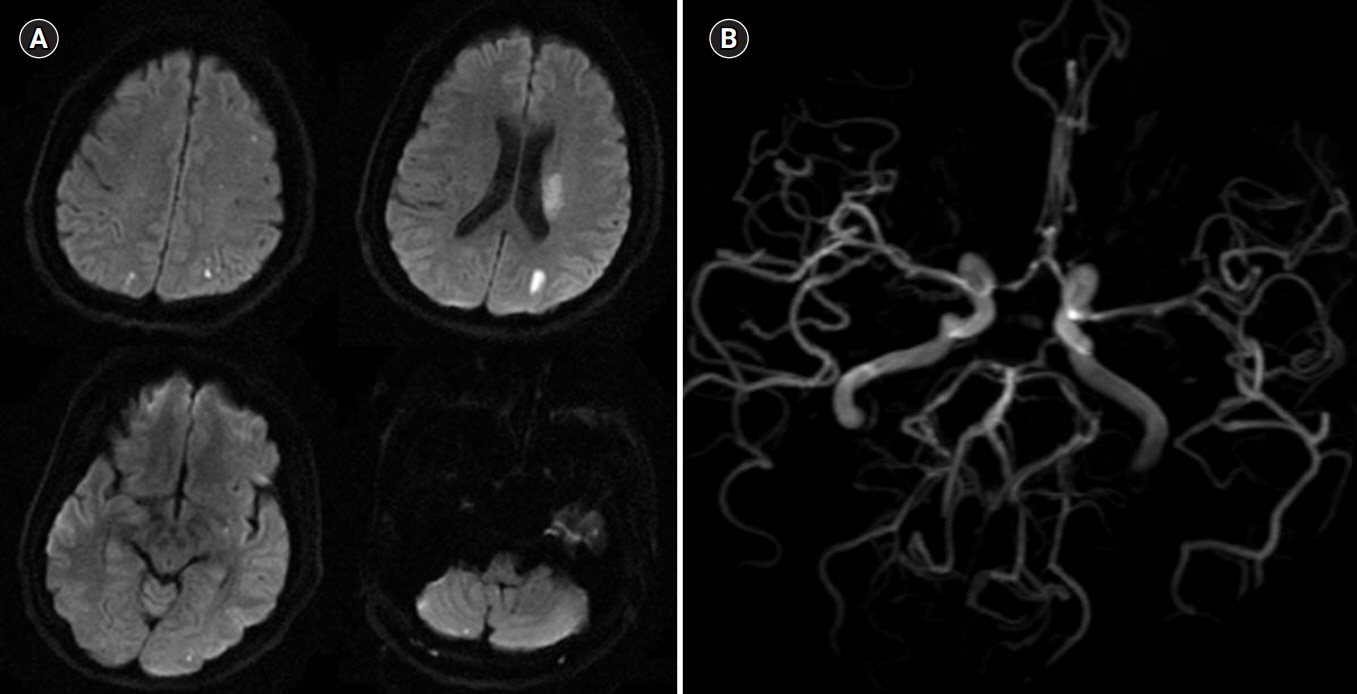
- Cerebrovascular complications that more likely to occur during pregnancy or postpartum include cerebral venous thrombosis, ischemic and hemorrhagic stroke, posterior reversible encephalopathy syndrome, and postpartum angiopathy, which although rare, can lead to serious outcomes for both mother and fetus. Pregnancy is a very unique condition, especially, in terms of treatment and, as such, neurointensivists must always consider its potential effects on the fetus. The purpose of this review is to help understand the physiological changes during pregnancy and postpartum, and to inform treatment decisions regarding pregnancy-related cerebrovascular complications.
Keyword
MeSH Terms
Figure
Reference
-
1. Plauché WC. Myasthenia gravis in mothers and their newborns. Clin Obstet Gynecol. 1991; 34:82–99.2. Confavreux C, Hutchinson M, Hours MM, Cortinovis-Tourniaire P, Moreau T. Rate of pregnancy-related relapse in multiple sclerosis. Pregnancy in Multiple Sclerosis Group. N Engl J Med. 1998; 339:285–91.3. Schmidt D, Canger R, Avanzini G, Battino D, Cusi C, Beck-Mannagetta G, et al. Change of seizure frequency in pregnant epileptic women. J Neurol Neurosurg Psychiatry. 1983; 46:751–5.
Article4. Otani K. Risk factors for the increased seizure frequency during pregnancy and puerperium. Folia Psychiatr Neurol Jpn. 1985; 39:33–41.
Article5. Reisinger TL, Newman M, Loring DW, Pennell PB, Meador KJ. Antiepileptic drug clearance and seizure frequency during pregnancy in women with epilepsy. Epilepsy Behav. 2013; 29:13–8.
Article6. Capeless EL, Clapp JF. Cardiovascular changes in early phase of pregnancy. Am J Obstet Gynecol. 1989; 161(6 Pt 1):1449–53.
Article7. Feske SK, Singhal AB. Cerebrovascular disorders complicating pregnancy. Continuum (Minneap Minn). 2014; 20:80–99.
Article8. Gilson GJ, Samaan S, Crawford MH, Qualls CR, Curet LB. Changes in hemodynamics, ventricular remodeling, and ventricular contractility during normal pregnancy: a longitudinal study. Obstet Gynecol. 1997; 89:957–62.
Article9. Silversides CK, Colman JM. Physiological changes in pregnancy. In : Oakley C, Warnes CA, editors. Heart disease in pregnancy. 2nd ed. Malden: Blackwell Publishing;2007. p. 6–17.10. Liu LX, Arany Z. Maternal cardiac metabolism in pregnancy. Cardiovasc Res. 2014; 101:545–53.
Article11. Anderson RJ, Berl T, McDonald KM, Schrier RW. Prostaglandins: effects on blood pressure, renal blood flow, sodium and water excretion. Kidney Int. 1976; 10:205–15.
Article12. Hull AD, Long DM, Longo LD, Pearce WJ. Pregnancy-induced changes in ovine cerebral arteries. Am J Physiol. 1992; 262(1 Pt 2):R137–43.
Article13. Marx GF. Aortocaval compression: incidence and prevention. Bull N Y Acad Med. 1974; 50:443–6.14. Rabhi Y, Charras-Arthapignet C, Gris JC, Ayoub J, Brun JF, Lopez FM, et al. Lower limb vein enlargement and spontaneous blood flow echogenicity are normal sonographic findings during pregnancy. J Clin Ultrasound. 2000; 28:407–13.
Article15. Marik PE, Plante LA. Venous thromboembolic disease and pregnancy. N Engl J Med. 2008; 359:2025–33.
Article16. James AH. Thrombosis in pregnancy and maternal outcomes. Birth Defects Res C Embryo Today. 2015; 105:159–66.
Article17. Frontera JA, Ahmed W. Neurocritical care complications of pregnancy and puerperum. J Crit Care. 2014; 29:1069–81.
Article18. Abdul Sultan A, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ. Risk of first venous thromboembolism in pregnant women in hospital: population based cohort study from England. BMJ. 2013; 347:f6099.
Article19. Tepper NK, Boulet SL, Whiteman MK, Monsour M, Marchbanks PA, Hooper WC, et al. Postpartum venous thromboembolism: incidence and risk factors. Obstet Gynecol. 2014; 123:987–96.20. Abdul Sultan A, Grainge MJ, West J, Fleming KM, Nelson-Piercy C, Tata LJ. Impact of risk factors on the timing of first postpartum venous thromboembolism: a population-based cohort study from England. Blood. 2014; 124:2872–80.
Article21. De Stefano V, Chiusolo P, Paciaroni K, Leone G. Epidemiology of factor V Leiden: clinical implications. Semin Thromb Hemost. 1998; 24:367–79.
Article22. Kim S, Song I, Kim HK, Huh S. Thrombophilia in Korean patients with arterial or venous thromboembolisms. Ann Surg Treat Res. 2016; 90:340–5.
Article23. Kim TW, Kim WK, Lee JH, Kim SB, Kim SW, Suh C, et al. Low prevalence of activated protein C resistance and coagulation factor V Arg506 to Gln mutation among Korean patients with deep vein thrombosis. J Korean Med Sci. 1998; 13:587–90.
Article24. Grandone E, Margaglione M, Colaizzo D, D'Andrea G, Cappucci G, Brancaccio V, et al. Genetic susceptibility to pregnancy-related venous thromboembolism: roles of factor V Leiden, prothrombin G20210A, and methylenetetrahydrofolate reductase C677T mutations. Am J Obstet Gynecol. 1998; 179:1324–8.
Article25. Rosendaal FR, Reitsma PH. Genetics of venous thrombosis. J Thromb Haemost. 2009; 7 Suppl 1:301–4.
Article26. Branch DW, Silver RM, Blackwell JL, Reading JC, Scott JR. Outcome of treated pregnancies in women with antiphospholipid syndrome: an update of the Utah experience. Obstet Gynecol. 1992; 80:614–20.27. Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO. VTE, thrombophilia, antithrombotic therapy, and pregnancy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e691S–736S.28. Bateman BT, Schumacher HC, Bushnell CD, Pile-Spellman J, Simpson LL, Sacco RL, et al. Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology. 2006; 67:424–9.
Article29. Scott CA, Bewley S, Rudd A, Spark P, Kurinczuk JJ, Brocklehurst P, et al. Incidence, risk factors, management, and outcomes of stroke in pregnancy. Obstet Gynecol. 2012; 120(2 Pt 1):318–24.
Article30. ACOG Practice Bulletin No. 202: Gestational hypertension and preeclampsia. Obstet Gynecol. 2019; 133:e1–25.31. Heit JA, Kobbervig CE, James AH, Petterson TM, Bailey KR, Melton LJ 3rd. Trends in the incidence of venous thromboembolism during pregnancy or postpartum: a 30-year population-based study. Ann Intern Med. 2005; 143:697–706.
Article32. James AH. Prevention and treatment of venous thromboembolism in pregnancy. Clin Obstet Gynecol. 2012; 55:774–87.
Article33. Konkle BA. Diagnosis and management of thrombosis in pregnancy. Birth Defects Res C Embryo Today. 2015; 105:185–9.
Article34. Cantú C, Barinagarrementeria F. Cerebral venous thrombosis associated with pregnancy and puerperium. Review of 67 cases. Stroke. 1993; 24:1880–4.
Article35. James AH, Jamison MG, Brancazio LR, Myers ER. Venous thromboembolism during pregnancy and the postpartum period: incidence, risk factors, and mortality. Am J Obstet Gynecol. 2006; 194:1311–5.
Article36. James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005; 106:509–16.
Article37. Witlin AG, Friedman SA, Egerman RS, Frangieh AY, Sibai BM. Cerebrovascular disorders complicating pregnancy: beyond eclampsia. Am J Obstet Gynecol. 1997; 176:1139–45.38. Bousser MG, Ferro JM. Cerebral venous thrombosis: an update. Lancet Neurol. 2007; 6:162–70.
Article39. Howie PW. Anticoagulants in pregnancy. Clin Obstet Gynaecol. 1986; 13:349–63.
Article40. Rutherford SE, Phelan JP. Thromboembolic disease in pregnancy. Clin Perinatol. 1986; 13:719–39.
Article41. Burgazlı KM, Bilgin M, Kavukçu E, Altay MM, Ozkan HT, Coşkun U, et al. Diagnosis and treatment of deep-vein thrombosis and approach to venous thromboembolism in obstetrics and gynecology. J Turk Ger Gynecol Assoc. 2011; 12:168–75.42. Cohen H, Arachchillage DR, Middeldorp S, Beyer-Westendorf J, Abdul-Kadir R. Management of direct oral anticoagulants in women of childbearing potential: guidance from the SSC of the ISTH. J Thromb Haemost. 2016; 14:1673–6.
Article43. Forestier F, Daffos F, Capella-Pavlovsky M. Low molecular weight heparin (PK 10169) does not cross the placenta during the second trimester of pregnancy study by direct fetal blood sampling under ultrasound. Thromb Res. 1984; 34:557–60.
Article44. Forestier F, Daffos F, Rainaut M, Toulemonde F. Low molecular weight heparin (CY 216) does not cross the placenta during the third trimester of pregnancy. Thromb Haemost. 1987; 57:234.
Article45. Wasay M, Bakshi R, Bobustuc G, Kojan S, Sheikh Z, Dai A, et al. Cerebral venous thrombosis: analysis of a multicenter cohort from the United States. J Stroke Cerebrovasc Dis. 2008; 17:49–54.
Article46. Arya R. How I manage venous thromboembolism in pregnancy. Br J Haematol. 2011; 153:698–708.
Article47. McKenna R, Cole ER, Vasan U. Is warfarin sodium contraindicated in the lactating mother? J Pediatr. 1983; 103:325–7.
Article48. Razmara A, Bakhadirov K, Batra A, Feske SK. Cerebrovascular complications of pregnancy and the postpartum period. Curr Cardiol Rep. 2014; 16:532.
Article49. Grear KE, Bushnell CD. Stroke and pregnancy: clinical presentation, evaluation, treatment, and epidemiology. Clin Obstet Gynecol. 2013; 56:350–9.50. Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, et al. Pregnancy and the risk of stroke. N Engl J Med. 1996; 335:768–74.
Article51. Dias MS, Sekhar LN. Intracranial hemorrhage from aneurysms and arteriovenous malformations during pregnancy and the puerperium. Neurosurgery. 1990; 27:855–65.
Article52. Horton JC, Chambers WA, Lyons SL, Adams RD, Kjellberg RN. Pregnancy and the risk of hemorrhage from cerebral arteriovenous malformations. Neurosurgery. 1990; 27:867–71.
Article53. Sharma A, Whitesell RT, Moran KJ. Imaging pattern of intracranial hemorrhage in the setting of posterior reversible encephalopathy syndrome. Neuroradiology. 2010; 52:855–63.
Article54. Fugate JE, Ameriso SF, Ortiz G, Schottlaender LV, Wijdicks EF, Flemming KD, et al. Variable presentations of postpartum angiopathy. Stroke. 2012; 43:670–6.
Article55. Mas JL, Lamy C. Stroke in pregnancy and the puerperium. J Neurol. 1998; 245:305–13.
Article56. Feske SK. Stroke in pregnancy. Semin Neurol. 2007; 27:442–52.
Article57. Lamy C, Oppenheim C, Méder JF, Mas JL. Neuroimaging in posterior reversible encephalopathy syndrome. J Neuroimaging. 2004; 14:89–96.
Article58. McKinney AM, Jagadeesan BD, Truwit CL. Central-variant posterior reversible encephalopathy syndrome: brainstem or basal ganglia involvement lacking cortical or subcortical cerebral edema. AJR Am J Roentgenol. 2013; 201:631–8.
Article59. Raman R, Devaramane R, Jagadish GM, Chowdaiah S. Various imaging manifestations of posterior reversible encephalopathy syndrome (PRES) on magnetic resonance imaging (MRI). Pol J Radiol. 2017; 82:64–70.
Article60. Savvidou MD, Hingorani AD, Tsikas D, Frölich JC, Vallance P, Nicolaides KH. Endothelial dysfunction and raised plasma concentrations of asymmetric dimethylarginine in pregnant women who subsequently develop pre-eclampsia. Lancet. 2003; 361:1511–7.
Article61. Schwartz RB, Feske SK, Polak JF, DeGirolami U, Iaia A, Beckner KM, et al. Preeclampsia-eclampsia: clinical and neuroradiographic correlates and insights into the pathogenesis of hypertensive encephalopathy. Radiology. 2000; 217:371–6.
Article62. Edvinsson L, Owman C, Sjöberg NO. Autonomic nerves, mast cells, and amine receptors in human brain vessels. A histochemical and pharmacological study. Brain Res. 1976; 115:377–93.
Article63. Singhal AB, Hajj-Ali RA, Topcuoglu MA, Fok J, Bena J, Yang D, et al. Reversible cerebral vasoconstriction syndromes: analysis of 139 cases. Arch Neurol. 2011; 68:1005–12.64. Ducros A, Bousser MG. Reversible cerebral vasoconstriction syndrome. Pract Neurol. 2009; 9:256–67.
Article65. Singhal AB. Postpartum angiopathy with reversible posterior leukoencephalopathy. Arch Neurol. 2004; 61:411–6.
Article66. Ducros A. Reversible cerebral vasoconstriction syndrome. Lancet Neurol. 2012; 11:906–17.
Article67. Singhal AB, Bernstein RA. Postpartum angiopathy and other cerebral vasoconstriction syndromes. Neurocrit Care. 2005; 3:91–7.
Article68. Leonhardt G, Gaul C, Nietsch HH, Buerke M, Schleussner E. Thrombolytic therapy in pregnancy. J Thromb Thrombolysis. 2006; 21:271–6.
Article69. Jauch EC, Saver JL, Adams HP Jr, Bruno A, Connors JJ, Demaerschalk BM, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013; 44:870–947.70. Leffert LR, Clancy CR, Bateman BT, Cox M, Schulte PJ, Smith EE, et al. Treatment patterns and short-term outcomes in ischemic stroke in pregnancy or postpartum period. Am J Obstet Gynecol. 2016; 214:723.
Article71. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–110.
Article72. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160–236.73. CLASP collaborative group. Low dose aspirin in pregnancy and early childhood development: follow up of the collaborative low dose aspirin study in pregnancy. Br J Obstet Gynaecol. 1995; 102:861–8.74. Roberge S, Bujold E, Nicolaides KH. Meta-analysis on the effect of aspirin use for prevention of preeclampsia on placental abruption and antepartum hemorrhage. Am J Obstet Gynecol. 2018; 218:483–9.
Article75. Meyers PM, Halbach VV, Malek AM, Phatouros CC, Dowd CF, Lawton MT, et al. Endovascular treatment of cerebral artery aneurysms during pregnancy: report of three cases. AJNR Am J Neuroradiol. 2000; 21:1306–11.76. Visintin C, Mugglestone MA, Almerie MQ, Nherera LM, James D, Walkinshaw S, et al. Management of hypertensive disorders during pregnancy: summary of NICE guidance. BMJ. 2010; 341:c2207.
Article77. American College of Obstetricians and Gynecologists; Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013; 122:1122–31.78. Kintiraki E, Papakatsika S, Kotronis G, Goulis DG, Kotsis V. Pregnancy-induced hypertension. Hormones (Athens). 2015; 14:211–23.
Article79. Which anticonvulsant for women with eclampsia? Evidence from the Collaborative Eclampsia Trial. Lancet. 1995; 345:1455–63.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Pruritic Urticarial Papules and Plaques of Pregnancy in the Postpartum
- Two Cases of Cerebral Hemorrhage in the Antepartum and Postpartum
- Recurrent Hyperthyroidism Following Postpartum Thyroiditis in a Woman with Hashimoto's Thyroiditis
- Preeclampsia Increases the Incidence of Postpartum Cerebrovascular Disease in Korean Population
- Pruritic Urticarial Papules and Plaques of Pregnancy with Unique Distribution Developing in Postpartum Period