Investig Clin Urol.
2019 Jan;60(1):46-53. 10.4111/icu.2019.60.1.46.
Investigation of risk factors for community-acquired urinary tract infections caused by extended-spectrum beta-lactamase Escherichia coli and Klebsiella species
- Affiliations
-
- 1Department of Infectious Diseases and Clinical Microbiology, Samsun Training and Research Hospital, Health Sciences University, Samsun, Turkey.
- 2Department of Infectious Diseases and Clinical Microbiology, Ankara Training and Research Hospital, Health Sciences University, Ankara, Turkey.
- 3Department of Infectious Diseases and Clinical Microbiology, Hacettepe University, Ankara, Turkey.
- 4Department of Infectious Diseases and Clinical Microbiology, Ondokuz Mayıs University, Samsun, Turkey. ftemucin@yahoo.com.tr
- 5Department of Infectious Diseases and Clinical Microbiology, Gulhane Training and Researh Hospital, Ankara, Turkey.
- KMID: 2434625
- DOI: http://doi.org/10.4111/icu.2019.60.1.46
Abstract
- PURPOSE
The aim of this study was to determine the prevalence and risk factors for community-acquired urinary tract infections (CA-UTIs) caused by extended-spectrum β-lactamase (ESBL) producing Escherichia coli and Klebsiella species.
MATERIALS AND METHODS
The patients diagnosed with CA-UTIs caused by E. coli or Klebsiella spp. were included in the study. All of the patients were compared to demographic characteristics, underlying diseases, urinary tract pathology, history of hospitalization, use of antibiotics according to ESBL positivity.
RESULTS
A total of 322 urine isolates were studied. Sixty-six patients (37.1%) of a total of 178 patients were ESBL positive E. coli and Klebsiella spp. Being over the age of sixty (odds ratio [OR], 1.90; p=0.03), history of renal stone (OR, 3.00; p=0.03), urinary tract anatomical of physiological disorder (OR, 2.17; p=0.01), urologic intervention (OR, 3.43; p < 0.001), history of urinary tract surgery (OR, 3.10; p=0.01), history of urinary catheterization (OR, 3.43; p < 0.001), and hospitalization for last 1 year (OR, 3.70; p=0.01) and antibiotic usage in the last 3 months (OR, 1.90; p=0.04) were found as significant risk factors for the producing of ESBL. However, gender and underlying disease were not related for ESBL production.
CONCLUSIONS
In present study, high rate of ESBL positivity was detected in CA-UTIs. The increasing of infections caused by ESBL positive E. coli and Klebsiella spp. are bringing together a lot of the problem, such as antibiotic resistance and reducing treatment options for outpatients. Identification of underlying risk factors would be important for the development of preventive strategies.
Keyword
MeSH Terms
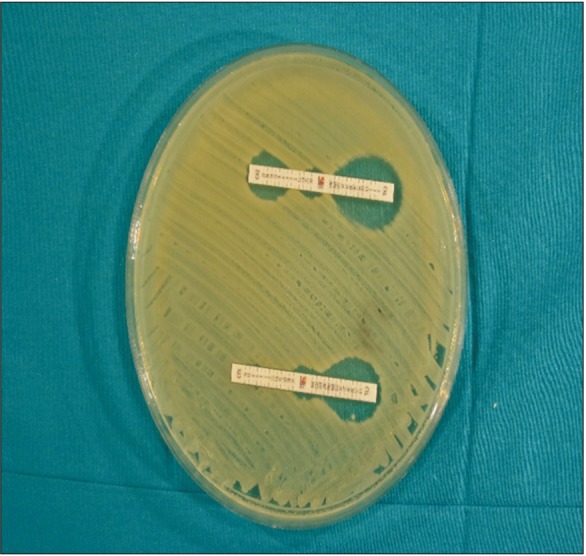
Figure
Reference
-
1. Tumbarello M, Spanu T, Sanguinetti M, Citton R, Montuori E, Leone F, et al. Bloodstream infections caused by extended-spectrum-beta-lactamase-producing Klebsiella pneumoniae: risk factors, molecular epidemiology, and clinical outcome. Antimicrob Agents Chemother. 2006; 50:498–504. PMID: 16436702.2. Kuster SP, Hasse B, Huebner V, Bansal V, Zbinden R, Ruef C, et al. Risks factors for infections with extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae at a tertiary care university hospital in Switzerland. Infection. 2010; 38:33–40. PMID: 20108162.
Article3. Hyle EP, Lipworth AD, Zaoutis TE, Nachamkin I, Fishman NO, Bilker WB, et al. Risk factors for increasing multidrug resistance among extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella species. Clin Infect Dis. 2005; 40:1317–1324. PMID: 15825035.4. Calbo E, Romaní V, Xercavins M, Gómez L, Vidal CG, Quintana S, et al. Risk factors for community-onset urinary tract infections due to Escherichia coli harbouring extended-spectrum beta-lactamases. J Antimicrob Chemother. 2006; 57:780–783. PMID: 16492721.5. Rodríguez-Baño J, Alcalá JC, Cisneros JM, Grill F, Oliver A, Horcajada JP, et al. Community infections caused by extended-spectrum beta-lactamase-producing Escherichia coli. Arch Intern Med. 2008; 168:1897–1902. PMID: 18809817.6. Meier S, Weber R, Zbinden R, Ruef C, Hasse B. Extended-spectrum β-lactamase-producing Gram-negative pathogens in community-acquired urinary tract infections: an increasing challenge for antimicrobial therapy. Infection. 2011; 39:333–340. PMID: 21706226.
Article7. Rodríguez-Baño J, Navarro MD, Romero L, Martínez-Martínez L, Muniain MA, Perea EJ, et al. Epidemiology and clinical features of infections caused by extended-spectrum beta-lactamase-producing Escherichia coli in nonhospitalized patients. J Clin Microbiol. 2004; 42:1089–1094. PMID: 15004058.8. Søraas A, Sundsfjord A, Sandven I, Brunborg C, Jenum PA. Risk factors for community-acquired urinary tract infections caused by ESBL-producing Enterobacteriaceae –a case-control study in a low prevalence country. PLoS One. 2013; 8:e69581. PMID: 23936052.
Article9. Ben-Ami R, Rodríguez-Baño J, Arslan H, Pitout JD, Quentin C, Calbo ES, et al. A multinational survey of risk factors for infection with extended-spectrum beta-lactamase-producing Enterobacteriaceae in nonhospitalized patients. Clin Infect Dis. 2009; 49:682–690. PMID: 19622043.10. Yilmaz E, Akalin H, Ozbey S, Kordan Y, Sinirtaş M, Gürcüoglu E, et al. Risk factors in community-acquired/onset urinary tract infections due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae. J Chemother. 2008; 20:581–585. PMID: 19028620.11. Azap OK, Arslan H, Serefhanoğlu K, Colakoğlu S, Erdoğan H, Timurkaynak F, et al. Risk factors for extended-spectrum beta-lactamase positivity in uropathogenic Escherichia coli isolated from community-acquired urinary tract infections. Clin Microbiol Infect. 2010; 16:147–151. PMID: 19689464.12. Sobel JD, Kaye D. Urinary tract infections. In : Bennett JE, Dolin R, Douglas RG, Mandell GL, editors. Mandell, Douglas, and Bennett's principles and practice of infectious diseases. 6th ed. Philadelphia: Churchill Livingstone;2005. p. 875–905.13. Matthew A Wikler. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing: twentieth informational supplement. Wayne: Clinical and Laboratory Standards Institute;2010.14. Steinke DT, Seaton RA, Phillips G, MacDonald TM, Davey PG. Prior trimethoprim use and trimethoprim-resistant urinary tract infection: a nested case-control study with multivariate analysis for other risk factors. J Antimicrob Chemother. 2001; 47:781–787. PMID: 11389110.
Article15. Arslan H, Azap OK, Ergönül O, Timurkaynak F. Urinary Tract Infection Study Group. Risk factors for ciprofloxacin resistance among Escherichia coli strains isolated from community-acquired urinary tract infections in Turkey. J Antimicrob Chemother. 2005; 56:914–918. PMID: 16174685.
Article16. Kurtaran B, Candevir A, Tasova Y, Kibar F, Inal AS, Komur S, et al. Antibiotic resistance in community-acquired urinary-tract infections: prevalence and risk factors. Med Sci Monit. 2010; 16:CR246–CR251. PMID: 20424552.17. Gupta K, Hooton TM, Naber KG, Wullt B, Colgan R, Miller LG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: a 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis. 2011; 52:e103–e120. PMID: 21292654.
Article18. Kung CH, Ku WW, Lee CH, Fung CP, Kuo SC, Chen TL, et al. Epidemiology and risk factors of community-onset urinary tract infection caused by extended-spectrum β-lactamase-producing Enterobacteriaceae in a medical center in Taiwan: a prospective cohort study. J Microbiol Immunol Infect. 2015; 48:168–174. PMID: 24064292.
Article19. Karlowsky JA, Kelly LJ, Thornsberry C, Jones ME, Sahm DF. Trends in antimicrobial resistance among urinary tract infection isolates of Escherichia coli from female outpatients in the United States. Antimicrob Agents Chemother. 2002; 46:2540–2545. PMID: 12121930.20. Kahlmeter G. An international survey of the antimicrobial susceptibility of pathogens from uncomplicated urinary tract infections: the ECO·SENS project. J Antimicrob Chemother. 2003; 51:69–76. PMID: 12493789.21. Zhanel GG, Karlowsky JA, Harding GK, Carrie A, Mazzulli T, Low DE, et al. A Canadian national surveillance study of urinary tract isolates from outpatients: comparison of the activities of trimethoprim-sulfamethoxazole, ampicillin, mecillinam, nitrofurantoin and ciprofloxacin. Antimicrob Agents Chemother. 2000; 44:1089–1092. PMID: 10722520.
Article22. Castanheira M, Farrell SE, Krause KM, Jones RN, Sader HS. Contemporary diversity of β-lactamases among Enterobacteriaceae in the nine U.S. census regions and ceftazidime-avibactam activity tested against isolates producing the most prevalent β-lactamase groups. Antimicrob Agents Chemother. 2014; 58:833–838. PMID: 24247134.
Article23. Nicolas-Chanoine MH, Bertrand X, Madec JY. Escherichia coli ST131, an intriguing clonal group. Clin Microbiol Rev. 2014; 27:543–574. PMID: 24982321.
Article24. Hyle EP, Lipworth AD, Zaoutis TE, Nachamkin I, Bilker WB, Lautenbach E. Impact of inadequate initial antimicrobial therapy on mortality in infections due to extended-spectrum beta-lactamase-producing Enterobacteriaceae: variability by site of infection. Arch Intern Med. 2005; 165:1375–1380. PMID: 15983286.25. Alós JI, Serrano MG, Gómez-Garcés JL, Perianes J. Antibiotic resistance of Escherichia coli from community-acquired urinary tract infections in relation to demographic and clinical data. Clin Microbiol Infect. 2005; 11:199–203. PMID: 15715717.
Article26. Colodner R, Rock W, Chazan B, Keller N, Guy N, Sakran W, et al. Risk factors for the development of extended-spectrum beta-lactamase-producing bacteria in nonhospitalized patients. Eur J Clin Microbiol Infect Dis. 2004; 23:163–167. PMID: 14986159.
Article27. Khanfar HS, Bindayna KM, Senok AC, Botta GA. Extended spectrum beta-lactamases (ESBL) in Escherichia coli and Klebsiella pneumoniae: trends in hospital and community settings. J Infect Dev Ctries. 2009; 3:295–299. PMID: 19759493.
Article28. Osthoff M, McGuinness SL, Wagen AZ, Eisen DP. Urinary tract infections due to extended-spectrum beta-lactamase-producing Gram-negative bacteria: identification of risk factors and outcome predictors in an Australian tertiary referral hospital. Int J Infect Dis. 2015; 34:79–83. PMID: 25769526.
Article29. Lautenbach E, Patel JB, Bilker WB, Edelstein PH, Fishman NO. Extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for infection and impact of resistance on outcomes. Clin Infect Dis. 2001; 32:1162–1171. PMID: 11283805.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors for Community-onset Urinary Tract Infections due to Extended-spectrum beta-lactamase Producing Bacteria in Children
- Febrile Urinary Tract Infections Caused by Community-Acquired Extended-Spectrum beta-Lactamase-Producing and-Nonproducing Bacteria: A Comparative Study
- Clinical Prediction Score for Community-Onset Bloodstream Infections Caused by Extended-Spectrum Beta-Lactamase-Producing Escherichia coli and Klebsiella Species
- Comparison of Extended-Spectrum beta-Lactamase-Producing Escherichia coli and Klebsiella pneumoniae Bloodstream Infection Epidemiology
- Community-onset Necrotizing Fasciitis Caused by Extended-spectrum Beta-lactamase-producing Eshcerichia coli