Anesth Pain Med.
2019 Jan;14(1):106-111. 10.17085/apm.2019.14.1.106.
Effect of the lateral tilt position on femoral vein cross-sectional area in anesthetized adults
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Chosun University School of Medicine, Gwangju.
- 2Kosin University College of Medicine, Busan, Korea. uamyfriends@hanmail.net
- KMID: 2434208
- DOI: http://doi.org/10.17085/apm.2019.14.1.106
Abstract
- BACKGROUND
A lateral tilt position can affect the size of the femoral vein (FV) due to increased venous blood volume in the dependent side of the body.
METHODS
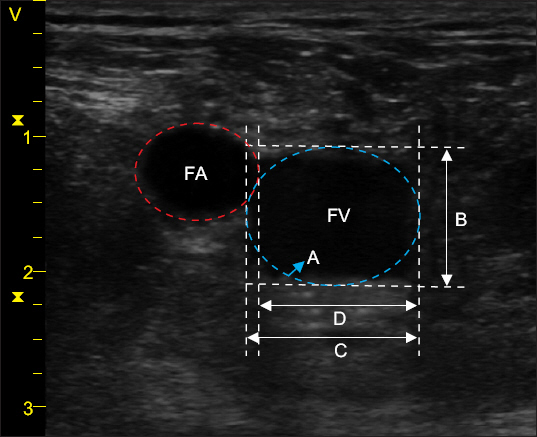
Forty-two patients, aged 20-60 years, were enrolled in this study. The crosssectional area (CSA), anteroposterior, and transverse diameters of the FV were measured 1 cm below the left inguinal line using ultrasound. The value of each parameter was recorded in the following four positions: (1) supine, (2) supine + 10° left-lateral tilt (LLT), (3) 10° reverse Trendelenburg (RT), and (4) RT + LLT.
RESULTS
CSAs of the left FV in the supine, supine + LLT, RT, RT + LLT positions were 0.93 ± 0.22, 1.11 ± 0.29, 1.17 ± 0.29, and 1.31 ± 0.32 cm2, respectively. Compared to the supine position, there was a significant increase in CSA and anteroposterior diameter according to the three changed positions. The transverse diameter of the left FV was significantly increased in supine + LLT, RT, RT + LLT positions compared to that in the supine position (P = 0.010, P = 0.043, P = 0.001, respectively). There was no significant difference in the transverse diameter of the left FV between the supine + LLT and RT positions (P = 1.000).
CONCLUSIONS
Adding LLT to the supine and RT positions increased the CSA of the unilateral FV significantly.
Keyword
MeSH Terms
Figure
Reference
-
1. Taylor RW, Palagiri AV. Central venous catheterization. Crit Care Med. 2007; 35:1390–6. DOI: 10.1097/01.CCM.0000260241.80346.1B. PMID: 17414086.2. Zhang J, Tang S, Hu C, Zhang C, He L, Li X, et al. Femorally inserted central venous catheter in patients with superior vena cava obstruction: choice of the optimal exit site. J Vasc Access. 2017; 18:82–8. DOI: 10.5301/jva.5000592. PMID: 27791258.3. Gordon AC, Saliken JC, Johns D, Owen R, Gray RR. US-guided puncture of the internal jugular vein: complications and anatomic considerations. J Vasc Interv Radiol. 1998; 9:333–8. DOI: 10.1016/S1051-0443(98)70277-5. PMID: 9540919.4. Stone MB, Price DD, Anderson BS. Ultrasonographic investigation of the effect of reverse Trendelenburg on the CSA of the femoral vein. J Emerg Med. 2006; 30:211–3. DOI: 10.1016/j.jemermed.2005.05.022. PMID: 16567260.5. Fronek A, Criqui MH, Denenberg J, Langer RD. Common femoral vein dimensions and hemodynamics including Valsalva response as a function of sex, age, and ethnicity in a population study. J Vasc Surg. 2001; 33:1050–6. DOI: 10.1067/mva.2001.113496. PMID: 11331848.6. Randall C, Schmeiser E, Fiers E, Little A, Dogbey G, Richardson G. Ultrasound investigation of leg position to enhance femoral vein exposure for cannulation. J Emerg Med. 2014; 47:176–81. DOI: 10.1016/j.jemermed.2014.02.001. PMID: 24725821.7. Kim W, Chung RK, Lee GY, Han JI. The effects of hip abduction with external rotation and reverse Trendelenburg position on the size of the femoral vein;ultrasonographic investigation. Korean J Anesthesiol. 2011; 61:205–9. DOI: 10.4097/kjae.2011.61.3.205. PMCID: PMC3198180. PMID: 22025941.8. Suk EH, Kim DH, Kil HK, Kweon TD. Effects of reverse Trendelenburg position and inguinal compression on femoral vein CSA in infants and young children. Anaesthesia. 2009; 64:399–402. DOI: 10.1111/j.1365-2044.2008.05815.x. PMID: 19317705.9. Olavarría VV, Arima H, Anderson CS, Brunser AM, Muñoz-Venturelli P, Heritier S, et al. Head position and cerebral blood flow velocity in acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2014; 37:401–8. DOI: 10.1159/000362533. PMID: 24993471.10. Kim HA, Yi HA, Hong JH, Lee H. Detailed relationship between the pattern of blood pressure change during the Valsalva maneuver and the degree of orthostatic hypotension during the head-up tilt test in patients with orthostatic intolerance: a retrospective case-control study. Medicine (Baltimore). 2016; 95:e3608. DOI: 10.1097/MD.0000000000003608. PMID: 27175668. PMCID: PMC4902510.11. Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015; 373:1220–9. DOI: 10.1056/NEJMoa1500964. PMID: 26398070.12. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003; 348:1123–33. DOI: 10.1056/NEJMra011883. PMID: 12646670.13. Cho WJ, Jang MK, Lee SC, Chin YJ, Chung CJ. Analysis for failure and immediate complications of subclavian venous catheterization. Anesth Pain Med. 2008; 3:149–53.14. Iwashima S, Ishikawa T, Ohzeki T. Ultrasound-guided versus landmark-guided femoral vein access in pediatric cardiac catheterization. Pediatr Cardiol. 2008; 29:339–42. DOI: 10.1007/s00246-007-9066-2. PMID: 17851631.15. Scholz T, Mathisen O, Bergan A, Osnes S, Innes R, Pedersen T, et al. Percutaneous technique for venovenous bypass including a heat exchanger is safe and reliable in liver transplantation. Transpl Int. 1997; 10:180–4. DOI: 10.1111/j.1432-2277.1997.tb00682.x. PMID: 9163856.16. Lu SY, Matsusaki T, Abuelkasem E, Sturdevant ML, Humar A, Hilmi IA, et al. Complications related to invasive hemodynamic monitors during adult liver transplantation. Clin Transplant. 2013; 27:823–8. DOI: 10.1111/ctr.12222. PMID: 24033433.17. Langer T, Santini A, Bottino N, Crotti S, Batchinsky AI, Pesenti A, et al. “Awake” extracorporeal membrane oxygenation (ECMO): pathophysiology, technical considerations, and clinical pioneering. Crit Care. 2016; 20:150. DOI: 10.1186/s13054-016-1329-y. PMID: 27357690. PMCID: PMC4928342.18. Powell JT, Mink JT, Nomura JT, Levine BJ, Jasani N, Nichols WL, et al. Ultrasound-guidance can reduce adverse events during femoral central venous cannulation. J Emerg Med. 2014; 46:519–24. DOI: 10.1016/j.jemermed.2013.08.023. PMID: 24462032.19. Reusz G, Csomos A. The role of ultrasound guidance for vascular access. Curr Opin Anaesthesiol. 2015; 28:710–6. DOI: 10.1097/ACO.0000000000000245. PMID: 26539789.20. Backlund BH, Hopkins E, Kendall JL. Ultrasound guidance for central venous access by emergency physicians in Colorado. West J Emerg Med. 2012; 13:320–5. DOI: 10.5811/westjem.2011.11.6821. PMID: 22942932. PMCID: PMC3421972.21. Buchanan MS, Backlund B, Liao MM, Sun J, Cydulka RK, Smith-Coggins R, et al. Use of ultrasound guidance for central venous catheter placement: survey from the American Board of Emergency Medicine longitudinal study of emergency physicians. Acad Emerg Med. 2014; 21:416–21. DOI: 10.1111/acem.12350. PMID: 24730404.22. Ballard DW, Reed ME, Rauchwerger AS, Chettipally UK, Offerman SR, Mark DG, et al. Emergency physician perspectives on central venous catheterization in the emergency department: a survey-based study. Acad Emerg Med. 2014; 21:623–30. DOI: 10.1111/acem.12386. PMID: 25039545.23. Soni NJ, Reyes LF, Keyt H, Arango A, Gelfond JA, Peters JI, et al. Use of ultrasound guidance for central venous catheterization: a national survey of intensivists and hospitalists. J Crit Care. 2016; 36:277–83. DOI: 10.1016/j.jcrc.2016.07.014. PMID: 27491563.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The effects of hip abduction with external rotation and reverse Trendelenburg position on the size of the femoral vein; ultrasonographic investigation
- Effect of Trendelenburg position on right and left internal jugular vein cross-sectional area
- The simultaneous application of positive-end expiratory pressure with the Trendelenburg position minimizes respiratory fluctuations in internal jugular vein size
- Effects of incrementally increasing tidal volume on the cross-sectional area of the right internal jugular vein
- Radiographic Examination at Lateral Decubitus Position for Reducing the Variability of Cup Inclination