Intest Res.
2018 Oct;16(4):579-587. 10.5217/ir.2018.00021.
Patient self-reported symptoms using visual analog scales are useful to estimate endoscopic activity in ulcerative colitis
- Affiliations
-
- 1Second Department of Internal Medicine, Wakayama Medical University, Wakayama, Japan. katojun@wakayama-med.ac.jp
- 2Inflammatory Bowel Disease Center, Yokohama City University Medical Center, Yokohama, Japan.
- KMID: 2434160
- DOI: http://doi.org/10.5217/ir.2018.00021
Abstract
- BACKGROUND/AIMS
In clinical practice, colonoscopy has been regarded as the gold standard for the evaluation of disease severity as well as mucosal healing in ulcerative colitis (UC). Some activity indices incorporating patient symptoms as parameters have been shown to reflect the endoscopic activity of UC. The aim of this study was to examine whether self-reported symptoms with visual analog scales (VAS) can predict endoscopic activity.
METHODS
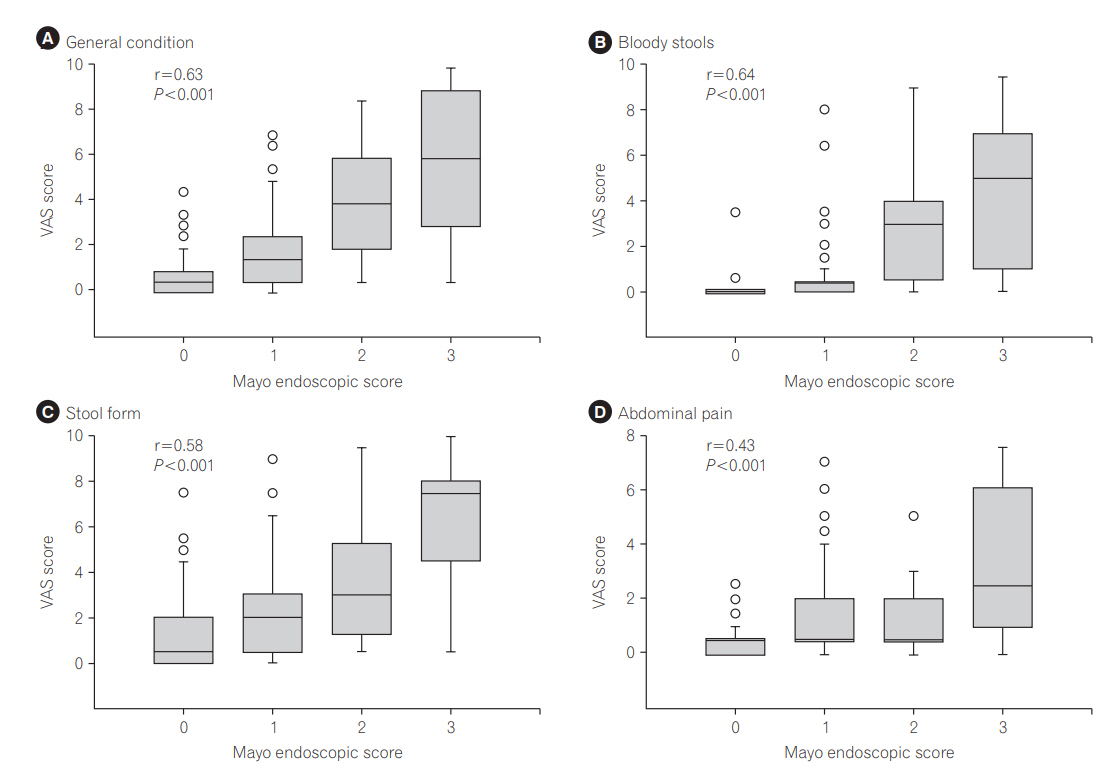
A cross-sectional study of 150 UC patients who underwent colonoscopy with submission of VAS scores of 4 symptoms: general condition, bloody stools, stool form, and abdominal pain (0: no symptoms, 10: the most severe symptoms). Each VAS score was compared with colonoscopic activity assessed with the Mayo endoscopic subscore (MES).
RESULTS
All VAS scores were significantly correlated with the endoscopic severity (Spearman correlation coefficients of general condition, bloody stools, stool form, and abdominal pain: 0.63, 0.64, 0.58, and 0.43, respectively). Mucosal healing defined as MES 0 alone was predicted by VAS score < 1.5 on general condition or 0 on bloody stools with sensitivity of 0.84 and 0.76 and specificity of 0.66 and 0.76, respectively. Additionally, VAS score < 2.5 on stool form predicted active lesions in distal colorectum alone with sensitivity of 0.67 and specificity of 0.66, suggesting that this item could predict the indication of topical therapy.
CONCLUSIONS
Self-reported VAS scores on symptoms were correlated with endoscopic activity of UC. To clarify the relationship between VAS and mucosal healing, further validation studies are needed.
MeSH Terms
Figure
Reference
-
1. Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012; 6:965–990.
Article2. Pineton de Chambrun G, Peyrin-Biroulet L, Lémann M, Colombel JF. Clinical implications of mucosal healing for the management of IBD. Nat Rev Gastroenterol Hepatol. 2010; 7:15–29.
Article3. Karoui S, Laz S, Serghini M, Bibani N, Boubaker J, Filali A. Correlation of C-reactive protein with clinical and endoscopic activity in patients with ulcerative colitis. Dig Dis Sci. 2011; 56:1801–1805.
Article4. Yoon JY, Park SJ, Hong SP, Kim TI, Kim WH, Cheon JH. Correlations of C-reactive protein levels and erythrocyte sedimentation rates with endoscopic activity indices in patients with ulcerative colitis. Dig Dis Sci. 2014; 59:829–837.
Article5. Nakarai A, Kato J, Hiraoka S, et al. Prognosis of ulcerative colitis differs between patients with complete and partial mucosal healing, which can be predicted from the platelet count. World J Gastroenterol. 2014; 20:18367–18374.
Article6. Røseth AG, Aadland E, Jahnsen J, Raknerud N. Assessment of disease activity in ulcerative colitis by faecal calprotectin, a novel granulocyte marker protein. Digestion. 1997; 58:176–180.
Article7. Hanai H, Takeuchi K, Iida T, et al. Relationship between fecal calprotectin, intestinal inflammation, and peripheral blood neutrophils in patients with active ulcerative colitis. Dig Dis Sci. 2004; 49:1438–1443.
Article8. D’Incà R, Dal Pont E, Di Leo V, et al. Calprotectin and lactoferrin in the assessment of intestinal inflammation and organic disease. Int J Colorectal Dis. 2007; 22:429–437.
Article9. Schoepfer AM, Beglinger C, Straumann A, Trummler M, Renzulli P, Seibold F. Ulcerative colitis: correlation of the Rachmilewitz endoscopic activity index with fecal calprotectin, clinical activity, C-reactive protein, and blood leukocytes. Inflamm Bowel Dis. 2009; 15:1851–1858.10. Kuriyama M, Kato J, Takemoto K, Hiraoka S, Okada H, Yamamoto K. Prediction of flare-ups of ulcerative colitis using quantitative immunochemical fecal occult blood test. World J Gastroenterol. 2010; 16:1110–1114.
Article11. Nakarai A, Kato J, Hiraoka S, et al. Evaluation of mucosal healing of ulcerative colitis by a quantitative fecal immunochemical test. Am J Gastroenterol. 2013; 108:83–89.
Article12. Takashima S, Kato J, Hiraoka S, et al. Evaluation of mucosal healing in ulcerative colitis by fecal calprotectin vs. fecal immunochemical test. Am J Gastroenterol. 2015; 110:873–880.
Article13. Powell-Tuck J, Day DW, Buckell NA, Wadsworth J, Lennard-Jones JE. Correlations between defined sigmoidoscopic appearances and other measures of disease activity in ulcerative colitis. Dig Dis Sci. 1982; 27:533–537.
Article14. Seo M, Okada M, Maeda K, Oh K. Correlation between endoscopic severity and the clinical activity index in ulcerative colitis. Am J Gastroenterol. 1998; 93:2124–2129.
Article15. Ricanek P, Brackmann S, Perminow G, et al. Evaluation of disease activity in IBD at the time of diagnosis by the use of clinical, biochemical, and fecal markers. Scand J Gastroenterol. 2011; 46:1081–1091.
Article16. Turner D, Seow CH, Greenberg GR, Griffiths AM, Silverberg MS, Steinhart AH. A systematic prospective comparison of noninvasive disease activity indices in ulcerative colitis. Clin Gastroenterol Hepatol. 2009; 7:1081–1088.
Article17. Pagnini C, Menasci F, Festa S, et al. Application of clinical indexes in ulcerative colitis patients in regular follow-up visit: correlation with endoscopic ‘mucosal healing’ and implication for management. Preliminary results. Eur Rev Med Pharmacol Sci. 2015; 19:3674–3681.18. Colombel JF, Rutgeerts P, Reinisch W, et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology. 2011; 141:1194–1201.
Article19. Huskisson EC. Measurement of pain. Lancet. 1974; 2:1127–1131.
Article20. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis: a randomized study. N Engl J Med. 1987; 317:1625–1629.
Article21. Walmsley RS, Ayres RC, Pounder RE, Allan RN. A simple clinical colitis activity index. Gut. 1998; 43:29–32.
Article22. Lichtiger S, Present DH, Kornbluth A, et al. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med. 1994; 330:1841–1845.
Article23. Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008; 14:1660–1666.
Article24. Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989; 298:82–86.
Article25. Sutherland LR, Martin F, Greer S, et al. 5-Aminosalicylic acid enema in the treatment of distal ulcerative colitis, proctosigmoiditis, and proctitis. Gastroenterology. 1987; 92:1894–1898.
Article26. Colombel JF, Keir ME, Scherl A, et al. Discrepancies between patient-reported outcomes, and endoscopic and histological appearance in UC. Gut. 2017; 66:2063–2068.
Article27. Yokoyama K, Kobayashi K, Mukae M, Sada M, Koizumi W. Clinical study of the relation between mucosal healing and longterm outcomes in ulcerative colitis. Gastroenterol Res Pract. 2013; 2013:192794. doi: 10.1155/2013/192794.
Article28. D’Haens G, Ferrante M, Vermeire S, et al. Fecal calprotectin is a surrogate marker for endoscopic lesions in inflammatory bowel disease. Inflamm Bowel Dis. 2012; 18:2218–2224.
Article29. Kristensen V, Klepp P, Cvancarova M, Røseth A, Skar V, Moum B. Prediction of endoscopic disease activity in ulcerative colitis by two different assays for fecal calprotectin. J Crohns Colitis. 2015; 9:164–169.
Article30. Langhorst J, Elsenbruch S, Koelzer J, Rueffer A, Michalsen A, Dobos GJ. Noninvasive markers in the assessment of intestinal inflammation in inflammatory bowel diseases: performance of fecal lactoferrin, calprotectin, and PMN-elastase, CRP, and clinical indices. Am J Gastroenterol. 2008; 103:162–169.
Article31. Kato J, Kuriyama M, Hiraoka S, Yamamoto K. Is sigmoidoscopy sufficient for evaluating inflammatory status of ulcerative colitis patients? J Gastroenterol Hepatol. 2011; 26:683–687.
Article32. Travis SP, Schnell D, Krzeski P, et al. Developing an instrument to assess the endoscopic severity of ulcerative colitis: the Ulcerative Colitis Endoscopic Index of Severity (UCEIS). Gut. 2012; 61:535–542.
Article33. Riley SA, Mani V, Goodman MJ, Dutt S, Herd ME. Microscopic activity in ulcerative colitis: what does it mean? Gut. 1991; 32:174–178.
Article34. Bessissow T, Lemmens B, Ferrante M, et al. Prognostic value of serologic and histologic markers on clinical relapse in ulcerative colitis patients with mucosal healing. Am J Gastroenterol. 2012; 107:1684–1692.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Nonischemic Central Retinal Vein Occlusion Developed in the course of Ulcerative Colits
- A Case of Cytomegalvirus Colitis Developed during the Treatment of Ulcerative Colitis
- Combined eosinophilic gastroenteritis and ulcerative colitis successfully treated by vedolizumab: a case report
- Chronological Review of Endoscopic Indices in Inflammatory Bowel Disease
- Acute pulmonary manifestation in ulcerative colitis