Chonnam Med J.
2019 Jan;55(1):54-61. 10.4068/cmj.2019.55.1.54.
Real World Comparison of Rivaroxaban and Warfarin in Korean Patients with Atrial Fibrillation: Propensity Matching Cohort Analysis
- Affiliations
-
- 1Department of Cardiovascular Medicine, Chonnam National University Hospital, Gwangju, Korea. drgood2@empas.com
- KMID: 2432256
- DOI: http://doi.org/10.4068/cmj.2019.55.1.54
Abstract
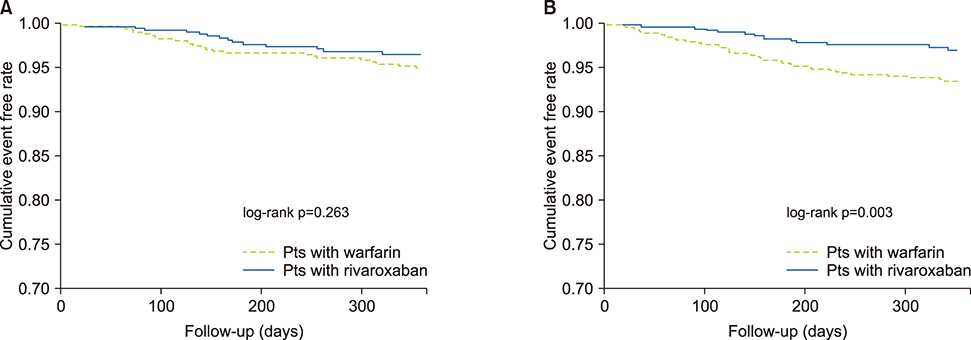
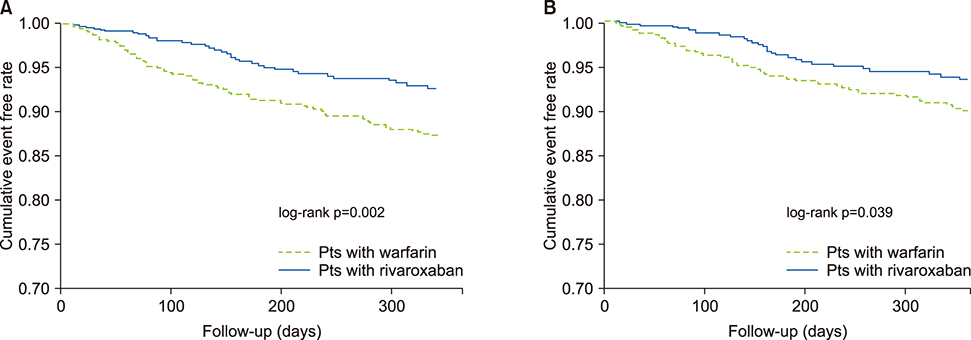
- Rivaroxaban has emerged as a potential alternative to warfarin for the prevention of thromboembolism in patients with atrial fibrillation (AF). However, there has been concern for the risk of major bleeding, especially in Asian patients. We investigated the efficacy and safety of rivaroxaban compared to warfarin in Korean real world practice. A total of 2,208 consecutive non-valvular AF patients were divided into the Warfarin group (n=990) and the Rivaroxaban group (n=1218). Propensity matched 1-year clinical outcomes were compared (Warfarin, n=804; Rivaroxaban, n=804). The efficacy outcome was defined as stroke/systemic embolism (SE). The safety outcome was major bleeding. The primary net clinical benefit (NCB) was defined as the composite of stroke/SE, major bleeding, and all-cause mortality. Secondary, NCB was defined as the composite of stroke, SE, and major bleeding. Rivaroxaban had the similar efficacy in terms of thromboembolic event prevention [hazard ratio (HR) 0.69, 95% confidence interval (CI) 0.37-1.32, p=0.266] compared to warfarin. Rivaroxaban significantly lowered the risk of major bleeding [HR 0.41, 95% CI 0.22-0.76, p=0.004]. Primary NCB was significantly low in the rivaroxaban group [HR 0.54, 95% CI 0.36-0.81, p=0.003]. Secondary NCB was also low in the rivaroxaban group [HR 0.62, 95% CI 0.40-0.99, p=0.041]. Both rivaroxaban 15 mg and 20 mg groups had similar efficacy and significantly lower risks of major bleeding as well as primary and secondary NCB compared to the warfarin group. In patients with non-valvular AF, rivaroxaban had a similar efficacy to warfarin in Korean real world practice. However, rivaroxaban had better safety and net clinical outcomes compared to warfarin.
Keyword
MeSH Terms
Figure
Reference
-
1. Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012; 125:e2–e220.2. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016; 18:1609–1678.
Article3. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.
Article4. Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361:1139–1151.
Article5. Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013; 369:2093–2104.
Article6. Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365:883–891.
Article7. Chan YH, See LC, Tu HT, Yeh YH, Chang SH, Wu LS, et al. Efficacy and safety of apixaban, dabigatran, rivaroxaban, and warfarin in Asians with nonvalvular atrial fibrillation. J Am Heart Assoc. 2018; 7:e008150.
Article8. Joung B. Real-world data and recommended dosage of non-vitamin K oral anticoagulants for Korean patients. Korean Circ J. 2017; 47:833–841.
Article9. Lopes RD, Guimarães PO, Kolls BJ, Wojdyla DM, Bushnell CD, Hanna M, et al. Intracranial hemorrhage in patients with atrial fibrillation receiving anticoagulation therapy. Blood. 2017; 129:2980–2987.
Article10. Shen AY, Yao JF, Brar SS, Jorgensen MB, Chen W. Racial/ethnic differences in the risk of intracranial hemorrhage among patients with atrial fibrillation. J Am Coll Cardiol. 2007; 50:309–315.
Article11. Li YG, Lee SR, Choi EK, Lip GY. Stroke prevention in atrial fibrillation: focus on Asian patients. Korean Circ J. 2018; 48:665–684.
Article12. Lip GY, Wang KL, Chiang CE. Non-vitamin K antagonist oral anticoagulants (NOACs) for stroke prevention in Asian patients with atrial fibrillation: time for a reappraisal. Int J Cardiol. 2015; 180:246–254.
Article13. Wang KL, Lip GY, Lin SJ, Chiang CE. Non-vitamin K antagonist oral anticoagulants for stroke prevention in Asian patients with nonvalvular atrial fibrillation: meta-analysis. Stroke. 2015; 46:2555–2561.
Article14. Camm AJ, Amarenco P, Haas S, Hess S, Kirchhof P, Kuhls S, et al. XANTUS: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation. Eur Heart J. 2016; 37:1145–1153.
Article15. Beyer-Westendorf J, Camm AJ, Coleman CI, Tamayo S. Rivaroxaban real-world evidence: validating safety and effectiveness in clinical practice. Thromb Haemost. 2016; 116:Suppl 2. S13–S23.
Article16. Lee KH, Park HW, Cho JG, Yoon NS, Kim SS, Kim MR, et al. Comparison of non-vitamin K antagonist oral anticoagulants and warfarin on clinical outcomes in atrial fibrillation patients with renal dysfunction. Europace. 2015; 17:Suppl 2. ii69–ii75.
Article17. Lee KH, Park HW, Lee N, Hyun DY, Won J, Oh SS, et al. Optimal dose of dabigatran for the prevention of thromboembolism with minimal bleeding risk in Korean patients with atrial fibrillation. Europace. 2017; 19:Suppl 4. iv1–iv9.
Article18. Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3:692–694.
Article19. JCS Joint Working Group. Guidelines for pharmacotherapy of atrial fibrillation (JCS 2013). Circ J. 2014; 78:1997–2021.20. Cha MJ, Choi EK, Han KD, Lee SR, Lim WH, Oh S, et al. Effectiveness and safety of non-vitamin K antagonist oral anticoagulants in Asian patients with atrial fibrillation. Stroke. 2017; 48:3040–3048.
Article21. Kim YH, Shim J, Tsai CT, Wang CC, Vilela G, Muengtaweepongsa S, et al. XANAP: a real-world, prospective, observational study of patients treated with rivaroxaban for stroke prevention in atrial fibrillation in Asia. J Arrhythm. 2018; 34:418–427.
Article22. Coleman CI, Antz M, Bowrin K, Evers T, Simard EP, Bonnemeier H, et al. Real-world evidence of stroke prevention in patients with nonvalvular atrial fibrillation in the United States: the REVISIT-US study. Curr Med Res Opin. 2016; 32:2047–2053.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical outcomes of direct-acting oral anticoagulants compared to warfarin in patients with non-valvular atrial fibrillation
- Real-world Data and Recommended Dosage of Non-vitamin K Oral Anticoagulants for Korean Patients
- New oral anticoagulants
- Cost-Effectiveness of Rivaroxaban Compared to Warfarin for Stroke Prevention in Atrial Fibrillation
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation