Ann Rehabil Med.
2018 Apr;42(2):270-276. 10.5535/arm.2018.42.2.270.
Pressure Relieving Effect of Adding a Pelvic Well Pad to a Wheelchair Cushion in Individuals With Spinal Cord Injury
- Affiliations
-
- 1Department of Rehabilitation Medicine, National Rehabilitation Center & Hospital, Seoul, Korea. zeeahan@catholic.ac.kr
- KMID: 2432197
- DOI: http://doi.org/10.5535/arm.2018.42.2.270
Abstract
OBJECTIVE
To identify the pressure relieving effect of adding a pelvic well pad, a firm pad that is cut in the ischial area, to a wheelchair cushion on the ischium.
METHODS
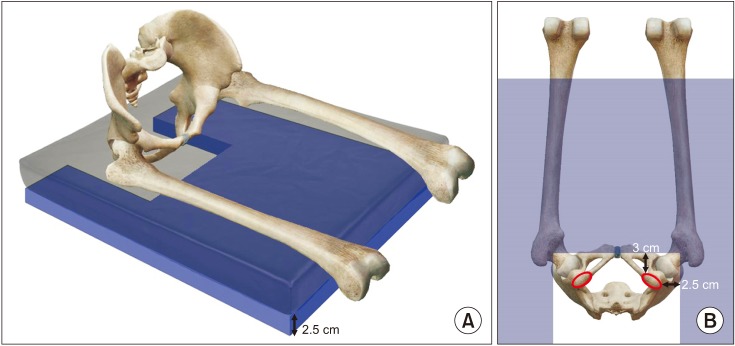
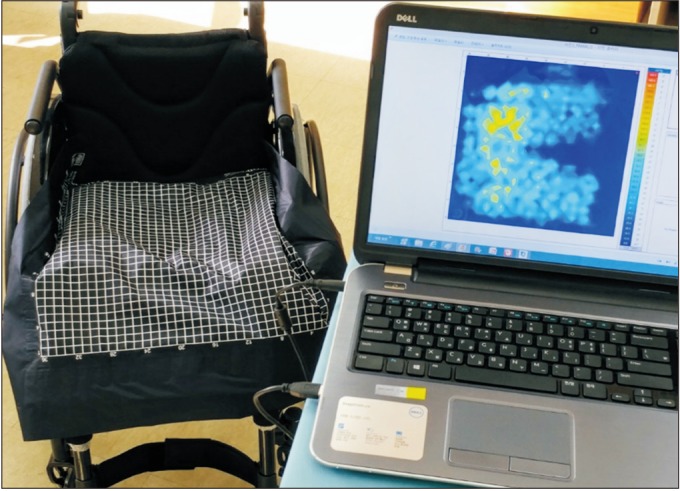
Medical records of 77 individuals with SCI, who underwent interface pressure mapping of the buttock-thigh area, were retrospectively reviewed. The pelvic well pad is a 2.5-cm thick firm pad and has a cut in the ischial area. Expecting additional pressure relief, it can be inserted under a wheelchair cushion. Subjects underwent interface pressure mapping in the subject's wheelchair utilizing the subject's pre-existing pressure relieving cushion and subsequently on a combination of a pelvic well pad and the cushion. The average pressure, peak pressure, and contact area of the buttock-thigh were evaluated.
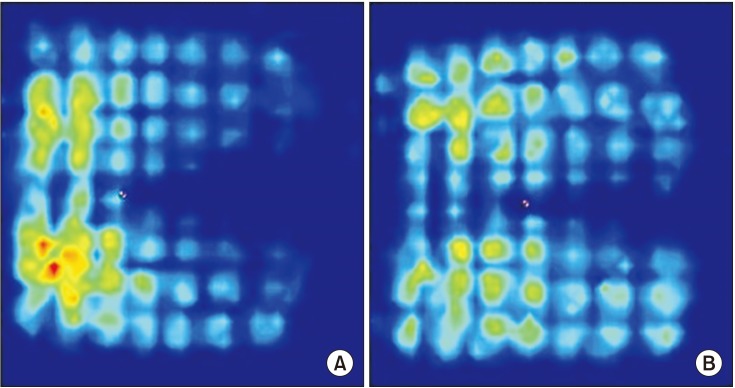
RESULTS
Adding a pelvic well pad, under the pressure relieving cushion, resulted in a decrease in the average and peak pressures and increase in the contact area of the buttock-thigh area when compared with applying only pressure relieving cushions (p < 0.05). The mean of the average pressure decreased from 46.10±10.26 to 44.09±9.92 mmHg and peak pressure decreased from 155.03±48.02 to 131.42±45.86 mmHg when adding a pelvic well pad. The mean of the contact area increased from 1,136.44±262.46 to 1,216.99±255.29 cm².
CONCLUSION
When a pelvic well pad was applied, in addition to a pre-existing pressure relieving cushion, the average and peak pressures of the buttock-thigh area decreased and the contact area increased. These results suggest that adding a pelvic well pad to wheelchair cushion may be effective in preventing a pressure ulcer of the buttock area.
Keyword
MeSH Terms
Figure
Reference
-
1. Javadi M, Hafezi-Nejad N, Vaccaro AR, Rahimi-Movaghar V. Medical complications and patient outcomes in Iranian veterans with spinal cord injury. Adv Clin Exp Med. 2014; 23:269–275. PMID: 24913118.
Article2. New PW, Rawicki HB, Bailey MJ. Nontraumatic spinal cord injury rehabilitation: pressure ulcer patterns, prediction, and impact. Arch Phys Med Rehabil. 2004; 85:87–93. PMID: 14970974.3. Yarkony GM. Pressure ulcers: a review. Arch Phys Med Rehabil. 1994; 75:908–917. PMID: 8053799.
Article4. Rabadi MH, Vincent AS. Do vascular risk factors contribute to the prevalence of pressure ulcer in veterans with spinal cord injury? J Spinal Cord Med. 2011; 34:46–51. PMID: 21528626.
Article5. Kim YC, Park CI, Shin JC, Kim SW, Yoo WK. Epidemiology of pressure sore in spinal cord injured patients. J Korean Acad Rehabil Med. 2010; 22:552–558.6. Stinson M, Schofield R, Gillan C, Morton J, Gardner E, Sprigle S, et al. Spinal cord injury and pressure ulcer prevention: using functional activity in pressure relief. Nurs Res Pract. 2013; 2013:860396. PMID: 23691301.
Article7. Groah SL, Schladen M, Pineda CG, Hsieh CH. Prevention of pressure ulcers among people with spinal cord injury: a systematic review. PM R. 2015; 7:613–636. PMID: 25529614.
Article8. Gil-Agudo A, De la Pena-Gonzalez A, Del Ama-Espinosa A, Perez-Rizo E, Diaz-Dominguez E, Sanchez-Ramos A. Comparative study of pressure distribution at the user-cushion interface with different cushions in a population with spinal cord injury. Clin Biomech (Bristol, Avon). 2009; 24:558–563.
Article9. Levy A, Kopplin K, Gefen A. An air-cell-based cushion for pressure ulcer protection remarkably reduces tissue stresses in the seated buttocks with respect to foams: finite element studies. J Tissue Viability. 2014; 23:13–23. PMID: 24405723.
Article10. Jan YK, Crane BA, Liao F, Woods JA, Ennis WJ. Comparison of muscle and skin perfusion over the ischial tuberosities in response to wheelchair tilt-in-space and recline angles in people with spinal cord injury. Arch Phys Med Rehabil. 2013; 94:1990–1996. PMID: 23602880.
Article11. Jan YK, Crane BA. Wheelchair tilt-in-space and recline does not reduce sacral skin perfusion as changing from the upright to the tilted and reclined position in people with spinal cord injury. Arch Phys Med Rehabil. 2013; 94:1207–1210. PMID: 23313352.
Article12. Jan YK, Liao F, Jones MA, Rice LA, Tisdell T. Effect of durations of wheelchair tilt-in-space and recline on skin perfusion over the ischial tuberosity in people with spinal cord injury. Arch Phys Med Rehabil. 2013; 94:667–672. PMID: 23178540.
Article13. Sprigle S, Maurer C, Soneblum SE. Load redistribution in variable position wheelchairs in people with spinal cord injury. J Spinal Cord Med. 2010; 33:58–64. PMID: 20397444.
Article14. Khasnabis C, Mines K. Wheelchair service training package: reference manual for participants: basic level. Geneva: World Health Organization;2012.15. Khasnabis C, Mines K. Wheelchair service training package: trainer's manual: basic level. Geneva: World Health Organization;2012.16. Peterson MJ, Gravenstein N, Schwab WK, van Oostrom JH, Caruso LJ. Patient repositioning and pressure ulcer risk: monitoring interface pressures of at-risk patients. J Rehabil Res Dev. 2013; 50:477–488. PMID: 23934869.17. Yuen HK, Garrett D. Comparison of three wheelchair cushions for effectiveness of pressure relief. Am J Occup Ther. 2001; 55:470–475. PMID: 11723993.
Article18. Makhsous M, Rowles DM, Rymer WZ, Bankard J, Nam EK, Chen D, et al. Periodically relieving ischial sitting load to decrease the risk of pressure ulcers. Arch Phys Med Rehabil. 2007; 88:862–870. PMID: 17601466.
Article19. Sonenblum SE, Vonk TE, Janssen TW, Sprigle SH. Effects of wheelchair cushions and pressure relief maneuvers on ischial interface pressure and blood flow in people with spinal cord injury. Arch Phys Med Rehabil. 2014; 95:1350–1357. PMID: 24480336.
Article20. Previnaire JG, Fontet P, Opsomer C, Simon M, Ducrocq T. Lipofilling (fat grafting) in the secondary prevention of ischial tuberosity and pelvic pressure ulcers. Spinal Cord. 2016; 54:39–45. PMID: 26481707.
Article21. Yusmido YA, Hisamud-Din N, Mazlan M. Elective proximal lower limb amputation in spinal cord injury patients with chronic pressure ulcers: improve quality of life, function, and shorten hospital stay: case report. Eur J Phys Rehabil Med. 2014; 50:557–560. PMID: 24694951.22. Kim DA, Yi SH, Lee BS, Lim MH, Ryh BJ, Kim HC, et al. Impact of sitting time on seat-interface pressure of spinal cord injured patients. J Korean Acad Rehabil Med. 2009; 33:614–618.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Sitting Time on Seat-Interface Pressure of Spinal Cord Injured Patients
- The Effects of Pressure Relief Methods at Wheelchair Seated Spinal Cord Injured Patients
- The Effects of Body Mass Composition and Cushion Type on Seat-Interface Pressure in Spinal Cord Injured Patients
- The Influence of Wheelchair Use of Individuals with Spinal Cord Injury on Upper Extremity Muscular Function and Cross-Sectional Area
- Effect of wheelchair ergometer training on spinal cord-injured paraplegics