Urogenit Tract Infect.
2018 Dec;13(3):66-71. 10.14777/uti.2018.13.3.66.
Comparison of the Efficacy between the Single-Dose and Three-Day Prophylactic Antibiotic Regimens for the Prevention of Bacterial Infections in Patients with Percutaneous Nephrolithotomy: A Randomized Controlled Study
- Affiliations
-
- 1Department of Urology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hkpark@amc.seoul.kr
- KMID: 2431250
- DOI: http://doi.org/10.14777/uti.2018.13.3.66
Abstract
- PURPOSE
To determine the appropriate regimen of antibiotic prophylaxis for the prevention of bacterial infections in patients receiving percutaneous nephrolithotomy (PCNL).
MATERIALS AND METHODS
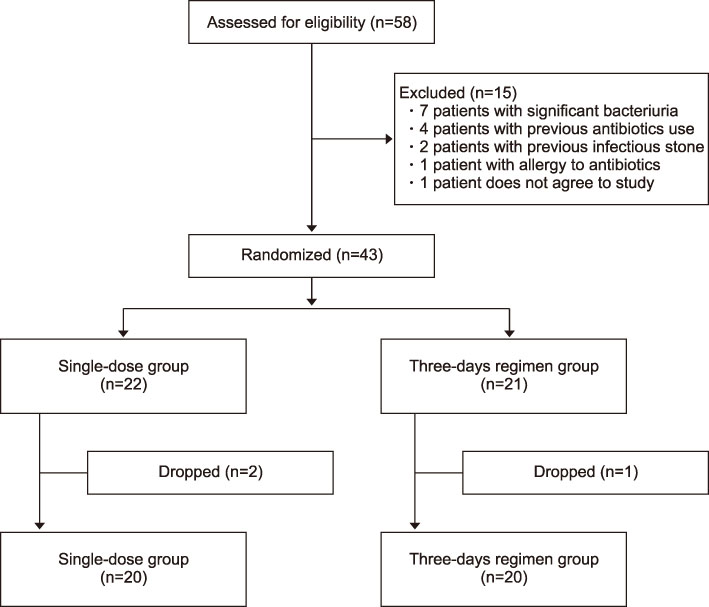
Forty patients, who planned to undergo PCNL from October 2015 to August 2017, were assigned randomly into two groups. Patients in the single-dose group (n=20) were administered an intravenous single dose of 2 g ceftriaxone 30 minutes before PCNL, whereas those in the three-days regimen group (n=20) were administered a preoperative intravenous single dose of 2 g ceftriaxone and an additional postoperative oral cefpodoxime proxetil (100 mg twice a day) for three days. The incidences of infectious complications in the two groups, such as pyrexia, systemic inflammatory response syndrome (SIRS), and sepsis, were compared.
RESULTS
Fever (axillary temperature >38.0℃) did not develop in any of the patients in the single-dose group but developed in one patient (5.0%) in the three-day regimen group due to pneumonia (p=0.3). SIRS developed in a total of eight patients (20.0%), four patients from each group. None of the patients in either group developed sepsis after PCNL.
CONCLUSIONS
The three-day prophylactic antibiotic regimen did not demonstrate better efficacy for the prevention of bacterial infections in patients with PCNL compared to the single-dose prophylactic antibiotic regimen.
MeSH Terms
Figure
Reference
-
1. Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016; 69:475–482.
Article2. Tyson MD 2nd, Humphreys MR. Postoperative complications after percutaneous nephrolithotomy: a contemporary analysis by insurance status in the United States. J Endourol. 2014; 28:291–297.
Article3. Singh P, Yadav S, Singh A, Saini AK, Kumar R, Seth A, et al. Systemic inflammatory response syndrome following percutaneous nephrolithotomy: assessment of risk factors and their impact on patient outcomes. Urol Int. 2016; 96:207–211.
Article4. Wolf JS Jr, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ. Urologic Surgery Antimicrobial Prophylaxis Best Practice Policy Panel. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008; 179:1379–1390.
Article5. Cadeddu JA, Chen R, Bishoff J, Micali S, Kumar A, Moore RG, et al. Clinical significance of fever after percutaneous nephrolithotomy. Urology. 1998; 52:48–50.
Article6. Shim M, Park M, Park HK. Effects of continuous peritubal local anesthetic instillation on postoperative pain after percutaneous nephrolithotomy: a prospective, randomized three-arm study. J Endourol. 2016; 30:504–509.
Article7. Tom WR, Wollin DA, Jiang R, Radvak D, Simmons WN, Preminger GM, et al. Next-generation single-use ureteroscopes: an in vitro comparison. J Endourol. 2017; 31:1301–1306.
Article8. Turck M, Stamm W. Nosocomial infection of the urinary tract. Am J Med. 1981; 70:651–654.
Article9. Farrell DJ, Morrissey I, De Rubeis D, Robbins M, Felmingham D. A UK multicentre study of the antimicrobial susceptibility of bacterial pathogens causing urinary tract infection. J Infect. 2003; 46:94–100.
Article10. Bryce A, Hay AD, Lane IF, Thornton HV, Wootton M, Costelloe C. Global prevalence of antibiotic resistance in paediatric urinary tract infections caused by Escherichia coli and association with routine use of antibiotics in primary care: systematic review and meta-analysis. BMJ. 2016; 352:i939.11. Niranjan V, Malini A. Antimicrobial resistance pattern in Escherichia coli causing urinary tract infection among inpatients. Indian J Med Res. 2014; 139:945–948.12. Zowawi HM, Harris PN, Roberts MJ, Tambyah PA, Schembri MA, Pezzani MD, et al. The emerging threat of multidrug-resistant Gram-negative bacteria in urology. Nat Rev Urol. 2015; 12:570–584.
Article13. Edlin RS, Shapiro DJ, Hersh AL, Copp HL. Antibiotic resistance patterns of outpatient pediatric urinary tract infections. J Urol. 2013; 190:222–227.
Article14. Bag S, Kumar S, Taneja N, Sharma V, Mandal AK, Singh SK. One week of nitrofurantoin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. Urology. 2011; 77:45–49.
Article15. Demirtas A, Yildirim YE, Sofikerim M, Kaya EG, Akinsal EC, Tombul ST, et al. Comparison of infection and urosepsis rates of ciprofloxacin and ceftriaxone prophylaxis before percutaneous nephrolithotomy: a prospective and randomised study. ScientificWorldJournal. 2012; 2012:916381.
Article16. Dogan HS, Sahin A, Cetinkaya Y, Akdogan B, Ozden E, Kendi S. Antibiotic prophylaxis in percutaneous nephrolithotomy: prospective study in 81 patients. J Endourol. 2002; 16:649–653.
Article17. Lai WS, Assimos D. The role of antibiotic prophylaxis in percutaneous nephrolithotomy. Rev Urol. 2016; 18:10–14.18. Chew BH, Miller NL, Abbott JE, Lange D, Humphreys MR, Pais VM Jr, et al. A randomized controlled trial of preoperative prophylactic antibiotics prior to percutaneous nephrolithotomy in a low infectious risk population: a report from the EDGE consortium. J Urol. 2018; 200:801–808.
Article19. Lee MY, Choi HJ, Choi JY, Song M, Song Y, Kim SW, et al. Dissemination of ST131 and ST393 community-onset, ciprofloxacin-resistant Escherichia coli clones causing urinary tract infections in Korea. J Infect. 2010; 60:146–153.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Is extended preoperative antibiotic prophylaxis for high-risk patients necessary before percutaneous nephrolithotomy?
- A Systematic Review of Randomized Controlled Trials of Antibiotic Use in Diabetic Foot Ulcer Infections: Focus on Clinical Cure
- Are prophylactic antibiotics necessary in elective laparoscopic cholecystectomy, regardless of patient risk?
- Recommendations for Antibacterial Prophylaxis in Endourological Procedures
- Prophylactic antibiotics in intra-oral bone grafting procedures: a prospective, randomized, double-blind clinical trial