Korean J Gastroenterol.
2018 Dec;72(6):318-321. 10.4166/kjg.2018.72.6.318.
Large Cell Neuroendocrine Carcinoma of the Extrahepatic Bile Duct
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea. drjtj@paik.ac.kr
- KMID: 2429950
- DOI: http://doi.org/10.4166/kjg.2018.72.6.318
Abstract
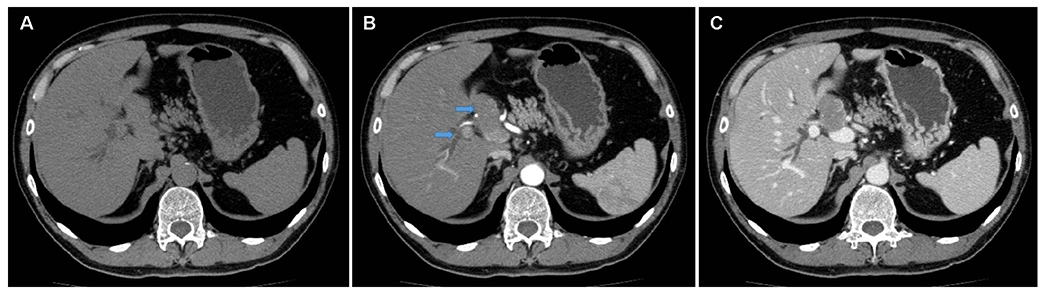
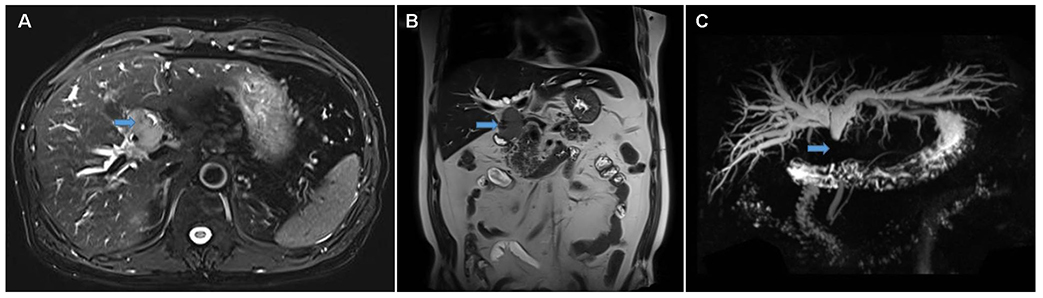
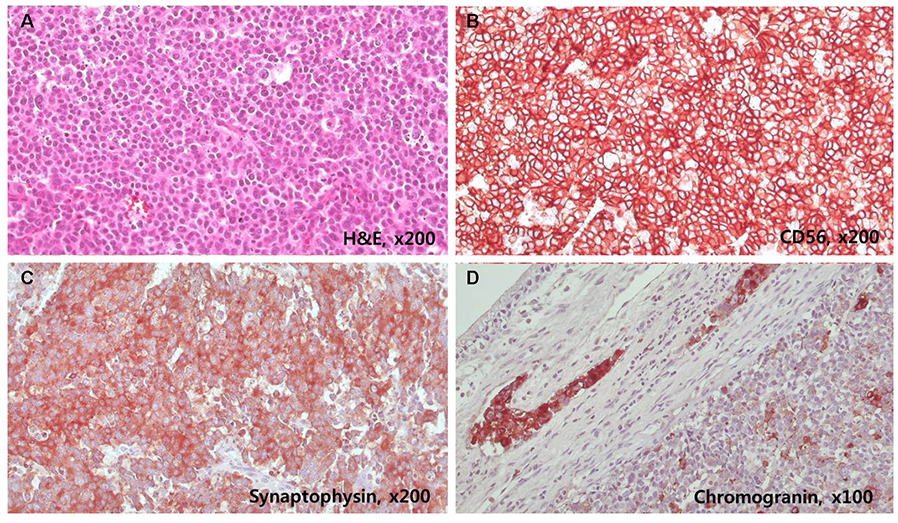
- Primary neuroendocrine tumors originating from the extrahepatic bile duct are rare. Among these tumors, large cell neuroendocrine carcinomas (NECs) are extremely rare. A 59-year-old man was admitted to Sanggye Paik Hospital with jaundice that started 10 days previously. He had a history of laparoscopic cholecystectomy, which he had undergone 12 years previously due to chronic calculous cholecystitis. Laboratory data showed abnormally elevated levels of total bilirubin 15.3 mg/dL (normal 0.2-1.2 mg/dL), AST 200 IU (normal 0-40 IU), ALT 390 IU (normal 0-40 IU), and gamma-glutamyl transferase 1,288 U/L (normal 0-60 U/L). Serum CEA was normal, but CA 19-9 was elevated 5,863 U/mL (normal 0-37 U/mL). Abdominal CT revealed a 4.5 cm sized mass involving the common bile duct and liver hilum and dilatation of both intrahepatic ducts. Percutaneous transhepatic drainage in the left hepatic duct was performed for preoperative biliary drainage. The patient underwent radical common bile duct and Roux-en-Y hepaticojejunostomy for histopathological diagnosis and surgical excision. On histopathological examination, the tumor exhibited large cell NEC (mitotic index >20/10 high-power field, Ki-67 index >20%, CD56 [+], synaptophysin [+], chromogranin [+]). Adjuvant concurrent chemotherapy and radiotherapy were started because the tumor had invaded the proximal resection margin. No recurrence was detected at 10 months by follow-up CT.
MeSH Terms
-
Bile Duct Neoplasms
Bile Ducts, Extrahepatic*
Bilirubin
Carcinoma, Neuroendocrine*
Cholecystectomy, Laparoscopic
Cholecystitis
Common Bile Duct
Diagnosis
Dilatation
Drainage
Drug Therapy
Follow-Up Studies
Hepatic Duct, Common
Humans
Jaundice
Liver
Middle Aged
Neuroendocrine Tumors
Radiotherapy
Recurrence
Synaptophysin
Tomography, X-Ray Computed
Transferases
Bilirubin
Synaptophysin
Transferases
Figure
Reference
-
1. Maggard MA, O'Connell JB, Ko CY. Updated population-based review of carcinoid tumors. Ann Surg. 2004; 240:117–122.
Article2. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003; 97:934–959.
Article3. Michalopoulos N, Papavramidis TS, Karayannopoulou G, Pliakos I, Papavramidis ST, Kanellos I. Neuroendocrine tumors of extrahepatic biliary tract. Pathol Oncol Res. 2014; 20:765–775.
Article4. Lee KJ, Cho JH, Lee SH, et al. Clinicopathological characteristics of biliary neuroendocrine neoplasms: a multicenter study. Scand J Gastroenterol. 2017; 52:437–441.
Article5. Ueda Y, Toyama H, Fukumoto T, Ku Y. Prognosis of patients with neuroendocrine neoplasms of the pancreas according to the World Health Organization 2017 classification. JOP. 2017; S(3):216–220.6. Murakami M, Katayama K, Kato S, et al. Large-cell neuroendocrine carcinoma of the common bile duct: a case report and a review of literature. Surg Case Rep. 2016; 2:141.
Article7. Barrón-Rodríguez LP, Manivel JC, Méndez-Sánchez N, Jessurun J. Carcinoid tumor of the common bile duct: evidence for its origin in metaplastic endocrine cells. Am J Gastroenterol. 1991; 86:1073–1076.8. Eltawil KM, Gustafsson BI, Kidd M, Modlin IM. Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol. 2010; 44:687–695.9. Albores-Saavedra J, Nadji M, Henson DE, Ziegels-Weissman J, Mones JM. Intestinal metaplasia of the gallbladder: a morphologic and immunocytochemical study. Hum Pathol. 1986; 17:614–620.
Article10. Kuwabara H, Uda H. Small cell carcinoma of the gall-bladder with intestinal metaplastic epithelium. Pathol Int. 1998; 48:303–306.
Article11. Papotti M, Cassoni P, Sapino A, Passarino G, Krueger JE, Albores-Saavedra J. Large cell neuroendocrine carcinoma of the gallbladder: report of two cases. Am J Surg Pathol. 2000; 24:1424–1428.12. Sasatomi E, Nalesnik MA, Marsh JW. Neuroendocrine carcinoma of the extrahepatic bile duct: case report and literature review. World J Gastroenterol. 2013; 19:4616–4623.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Small-cell Neuroendocrine Carcinoma of the Extrahepatic Bile Duct: A Rare Case Report
- A Case of Multiple Papillary Adenocarcinoma of the Extrahepatic Bile Duct : Findings of ERCP
- Extrahepatic Bile Duct Duplication with Intraductal Papillary Neoplasm: A Case Report
- Small Cell Carcinoma of Extahepatic Bile Duct Presenting with Hemobilia
- Signet Ring Cell Carcinoma of the Extrahepatic Bile Duct