J Cardiovasc Imaging.
2018 Sep;26(3):135-143. 10.4250/jcvi.2018.26.e17.
Cardiac Structural or Functional Changes Associated with CHAâ‚‚DSâ‚‚-VASc Scores in Nonvalvular Atrial Fibrillation: A Cross-Sectional Study Using Echocardiography
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Gachon University Gil Medical Center, Incheon, Korea. jeff76@gilhospital.com
- KMID: 2429854
- DOI: http://doi.org/10.4250/jcvi.2018.26.e17
Abstract
- BACKGROUND
CHA2DS2-VASc is the most widely accepted scoring system for atrial fibrillation (AF) to assess stroke risk, although little has been revealed regarding the accompanying cardiac functional/structural changes. This echocardiography study was undertaken to understand the changes related to CHA2DS2-VASc scores.
METHODS
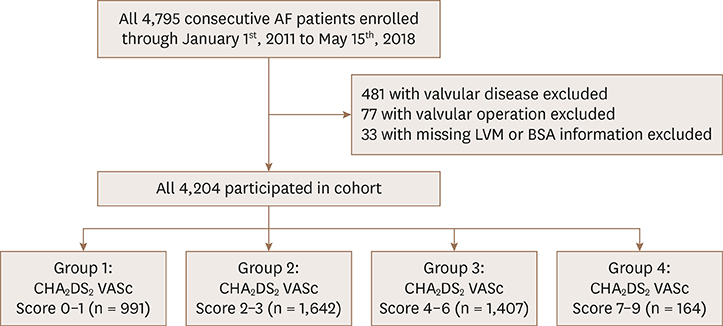
A total of 4,795 nonvalvular AF patients were enrolled for the cohort, from which 591 were excluded as they did not meet the inclusion criteria. Based on the CHA2DS2-VASc scores, the remaining 4,204 patients included in the study were divided into 4 groups: 0 to 1 (n = 991); 2 to 3 (n = 1,642); 4 to 6 (n = 1,407); 7 to 9 (n = 164).
RESULTS
Increase in the left ventricular mass index and prevalence of left ventricular hypertrophy (LVH) were observed with elevating CHA2DS2-VASc scores (p < 0.05 for all). Diastolic parameters such as left atrial volume index (LAVI) and the ratio of early diastolic mitral inflow velocity to early diastolic velocity of the mitral annulus (E/E"²) also increased significantly in the higher CHA2DS2-VASc score groups (p < 0.001 for all), although two-way ANOVA analysis showed that such incremental diastolic impairment was independent of hypertension. LVH (hazard ratio [HR], 3.609; confidence interval [CI], 2.426-5.369; p < 0.001) and E/E"² (HR, 1.087; CI, 1.054-1.121; p < 0.001) were independent risk factors for CHA2DS2-VASc scores 2 or higher.
CONCLUSIONS
Our findings suggest that increasing CHA2DS2-VASc scores are associated with impaired diastolic function that may represent high left atrial pressure favoring thrombogenic propensity.
Keyword
MeSH Terms
Figure
Reference
-
1. Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 2010; 12:1360–1420.2. Akar JG, Marieb MA. Atrial fibrillation and thrombogenesis: innocent bystander or guilty accomplice? JACC Clin Electrophysiol. 2015; 1:218–219.3. Di Tullio MR, Sacco RL, Sciacca RR, Homma S. Left atrial size and the risk of ischemic stroke in an ethnically mixed population. Stroke. 1999; 30:2019–2024.
Article4. Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009; 373:155–166.
Article5. Gupta DK, Giugliano RP, Ruff CT, et al. The prognostic significance of cardiac structure and function in atrial fibrillation: The ENGAGE AF-TIMI 48 Echocardiographic Substudy. J Am Soc Echocardiogr. 2016; 29:537–544.6. Olesen JB, Lip GY, Hansen ML, et al. Validation of risk stratification schemes for predicting stroke and thromboembolism in patients with atrial fibrillation: nationwide cohort study. BMJ. 2011; 342:d124.
Article7. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014; 63:2438–2488.8. Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005; 18:1440–1463.
Article9. Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling--concepts and clinical implications: a consensus paper from an international forum on cardiac remodeling. Behalf of an International Forum on Cardiac Remodeling. J Am Coll Cardiol. 2000; 35:569–582.10. Jia X, Levine GN, Birnbaum Y. The CHA2DS2-VASc score: Not as simple as it seems. Int J Cardiol. 2018; 257:92–96.11. Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Italian Society of Hypertension. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012; 26:343–349.
Article12. Eguchi K, Boden-Albala B, Jin Z, et al. Association between diabetes mellitus and left ventricular hypertrophy in a multiethnic population. Am J Cardiol. 2008; 101:1787–1791.
Article13. Proietti M, Marra AM, Tassone EJ, et al. Frequency of left ventricular hypertrophy in non-valvular atrial fibrillation. Am J Cardiol. 2015; 116:877–882.
Article14. Lim HS, Willoughby SR, Schultz C, et al. Thrombogenic risk in patients with atrial fibrillation: importance of comorbid conditions and intracardiac changes. JACC Clin Electrophysiol. 2015; 1:210–217.15. Buono F, Crispo S, Pagano G, et al. Determinants of left ventricular hypertrophy in patients with recent diagnosis of essential hypertension. J Hypertens. 2014; 32:166–173.
Article16. Gerdts E, Izzo R, Mancusi C, et al. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk (the Campania Salute Network). Int J Cardiol. 2018; 258:257–261.
Article17. Goldman ME, Pearce LA, Hart RG, et al. Pathophysiologic correlates of thromboembolism in nonvalvular atrial fibrillation: I. Reduced flow velocity in the left atrial appendage (The Stroke Prevention in Atrial Fibrillation [SPAF-III] study). J Am Soc Echocardiogr. 1999; 12:1080–1087.
Article18. Ha JW, Lee BK, Kim HJ, et al. Assessment of left atrial appendage filling pattern by using intravenous administration of microbubbles: comparison between mitral stenosis and mitral regurgitation. J Am Soc Echocardiogr. 2001; 14:1100–1106.
Article19. Shively BK, Gelgand EA, Crawford MH. Regional left atrial stasis during atrial fibrillation and flutter: determinants and relation to stroke. J Am Coll Cardiol. 1996; 27:1722–1729.20. Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev. 2011; 91:265–325.
Article21. Kim H, Park YA, Choi SM, et al. Associates and prognosis of giant left atrium; single center experience. J Cardiovasc Ultrasound. 2017; 25:84–90.
Article22. Okin PM, Wachtell K, Devereux RB, et al. Regression of electrocardiographic left ventricular hypertrophy and decreased incidence of new-onset atrial fibrillation in patients with hypertension. JAMA. 2006; 296:1242–1248.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Impact of the CHAâ‚‚DSâ‚‚-VASc Score on Recurrence of Atrial Fibrillation after a Single Catheter Ablation and Atrial Remodeling in Patients with Non-Valvular Atrial Fibrillation
- Stroke Prevention in Atrial Fibrillation
- CHAâ‚‚DSâ‚‚-VASc Score in the Prediction of Ischemic Stroke in Patients after Radiofrequency Catheter Ablation of Typical Atrial Flutter
- A Thin Left Atrial Antral Wall Around the Pulmonary Vein Reflects Structural Remodeling by Atrial Fibrillation and is Associated with Stroke
- A Comparative Study on Cerebral Infarction in Patient with Nonvalvular and Valvular Atrial Fibrillation