Adv Pediatr Surg.
2018 Dec;24(2):60-67. 10.13029/aps.2018.24.2.60.
Abdominal Lymphatic Malformation in Children
- Affiliations
-
- 1Department of Surgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, South Korea. kpnugs@knu.ac.kr
- KMID: 2429802
- DOI: http://doi.org/10.13029/aps.2018.24.2.60
Abstract
- PURPOSE
Lymphatic malformations are benign congenital malformations of the lymphatic system that occur predominantly in children. Most lymphatic malformations occur in the head and neck region, with those in abdominal locations, such as the mesentery, omentum and retroperitoneum, being less common, accounting for fewer than 5% of lymphatic malformations in children. This study analyzed the clinicopathologic characteristics and treatment outcomes of abdominal lymphatic malformations in children.
METHODS
The medical records of 12 pediatric patients treated for abdominal lymphatic malformations at our institution between April 1999 and September 2017 were retrospectively reviewed. Demographic and clinical characteristics, including gender, age, symptoms and signs, diagnostic modalities, and treatment results, were analyzed.
RESULTS
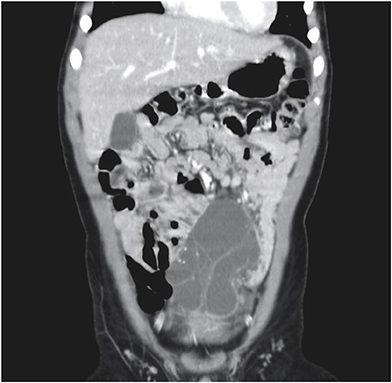
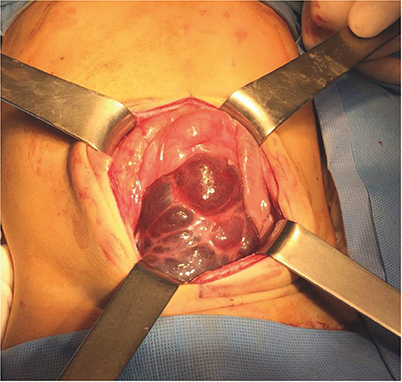
The 12 patients included 11 boys and 1 girl, ranging in age from 3 months to 17 years (median 36.5 months) at presentation. The primary signs and symptoms included abdominal pain, abdominal mass and abdominal distention. Other symptoms and signs included fever, vomiting, scrotal pain and mass, and right inguinal mass. All patients were diagnosed by abdominal ultrasonography and computed tomography, and all underwent surgical excision with or without bowel resection. The lymphatic malformations occurred in the retroperitoneum (n=4), omentum (n=4), jejunal mesentery (n=2), and retroperitoneum and mesentery (n=2). Seven patients underwent complete mass excision, including 3 who underwent laparoscopic excisions, and 3 who underwent mass excision with segmental resection of the adjoining bowel. Two patients underwent incomplete excision because the lesion was extensive and invaded the superior mesenteric vessels. There was no major perioperative morbidity in any patient. At a median follow-up of 50 months (range, 8-183 months), only 1 patient experienced recurrence.
CONCLUSION
Although abdominal lymphatic malformations are benign, most children present with acute abdominal symptoms, necessitating early surgical treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Kim SH, Kim HY, Lee C, Min HS, Jung SE. Clinical features of mesenteric lymphatic malformation in children. J Pediatr Surg. 2016; 51:582–587.
Article2. Muramori K, Zaizen Y, Noguchi S. Abdominal lymphangioma in children: report of three cases. Surg Today. 2009; 39:414–417.
Article3. Konen O, Rathaus V, Dlugy E, Freud E, Kessler A, Shapiro M, et al. Childhood abdominal cystic lymphangioma. Pediatr Radiol. 2002; 32:88–94.
Article4. Goh BK, Tan YM, Ong HS, Chui CH, Ooi LL, Chow PK, et al. Intra-abdominal and retroperitoneal lymphangiomas in pediatric and adult patients. World J Surg. 2005; 29:837–840.
Article5. Okazaki T, Iwatani S, Yanai T, Kobayashi H, Kato Y, Marusasa T, et al. Treatment of lymphangioma in children: our experience of 128 cases. J Pediatr Surg. 2007; 42:386–389.
Article6. de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg. 1998; 85:395–397.
Article7. Hinds DF, Aponte EM, Secko M, Mehta N. Identification of a pediatric intra-abdominal cystic lymphangioma using point-of-care ultrasonography. Pediatr Emerg Care. 2015; 31:62–64.
Article8. Li H, Bai YZ. Calcified mesenteric lymphangioma mimicking a teratoma in a 4-year-old child. Pediatr Neonatol. 2016; 57:256–258.
Article9. Wilson SR, Bohrer S, Losada R, Price AP. Retroperitoneal lymphangioma: an unusual location and presentation. J Pediatr Surg. 2006; 41:603–605.
Article10. Hancock BJ, St-Vil D, Luks FI, Di Lorenzo M, Blanchard H. Complications of lymphangiomas in children. J Pediatr Surg. 1992; 27:220–224.
Article11. Hatten MT, Hamrick-Turner JE, Smith DB. Mesenteric cystic lymphangioma: radiologic appearance mimicking cystic teratoma. Pediatr Radiol. 1996; 26:458–460.
Article12. Méndez-Gallart R, Bautista A, Estévez E, Rodríguez-Barca P. Abdominal cystic lymphangiomas in pediatrics: surgical approach and outcomes. Acta Chir Belg. 2011; 111:374–377.
Article13. Merrot T, Chaumoitre K, Simeoni-Alias J, Alessandrini P, Guys JM, Panuel M. Abdominal cystic lymphangiomas in children. Clinical, diagnostic and therapeutic aspects: apropos of 21 cases. Ann Chir. 1999; 53:494–499.14. Steyaert H, Guitard J, Moscovici J, Juricic M, Vaysse P, Juskiewenski S. Abdominal cystic lymphangioma in children: benign lesions that can have a proliferative course. J Pediatr Surg. 1996; 31:677–680.
Article15. Weeda VB, Booij KA, Aronson DC. Mesenteric cystic lymphangioma: a congenital and an acquired anomaly? Two cases and a review of the literature. J Pediatr Surg. 2008; 43:1206–1208.
Article16. Niu ZB. Retroperitoneal lymphatic malformation in child with horseshoe kidney. Urology. 2012; 79:437–439.
Article17. Rifenburg NE, Batton B, Vade A. Ruptured retroperitoneal lymphatic malformation. Comput Med Imaging Graph. 2006; 30:61–63.
Article18. Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003; 196:598–603.
Article19. Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004; 24:1353–1365.
Article20. Tian C, Zheng Y, Ren X, Li B. A giant abdominal cystic tumour: mesentery cystic lymphangioma. Dig Liver Dis. 2015; 47:816–817.
Article21. Teixeira L, Castro M, Leite J, Teixeira H, Teixeira R, Pettersen H, et al. Mesenteric cystic lymphangioma: a prenatal diagnostic challenge. Prenat Diagn. 2007; 27:479–480.
Article22. Kim HE, Seo JM, Lee SK. Laparoscopic excision of an intraabdominal cystic lymphangioma: a case report. J Korean Assoc Pediatr Surg. 2008; 14:196–199.
Article23. Fujino A, Moriya Y, Morikawa Y, Hoshino K, Watanabe T, Shimojima N, et al. A role of cytokines in OK-432 injection therapy for cystic lymphangioma: an approach to the mechanism. J Pediatr Surg. 2003; 38:1806–1809.
Article24. Hwang D, Lee S, Lim SY, Lee SK, Seo JM. Surgical treatment of difficult cervicofacial lymphangioma in children. J Korean Assoc Pediatr Surg. 2015; 21:17–23.
Article25. Mikhail M, Kennedy R, Cramer B, Smith T. Sclerosing of recurrent lymphangioma using OK-432. J Pediatr Surg. 1995; 30:1159–1160.
Article26. Ogita S, Tsuto T, Nakamura K, Deguchi E, Tokiwa K, Iwai N. OK-432 therapy for lymphangioma in children: why and how does it work? J Pediatr Surg. 1996; 31:477–480.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Congenital Lymphatic Malformation
- Radiofrequency Ablation of Microcystic Lymphatic Malformation in the Oral Cavity: 2 Case Studies
- Percutaneous Drainage and Povidone-Iodine Sclerotherapy of Cervical Lymphatic Malformation
- A Case of Klippel-Trenaunay Syndrome with Microcystic Lymphatic Malformation on Anus
- A Review of the Current State and Future Directions for Management of Scalp and Facial Vascular Malformations