J Korean Neurosurg Soc.
2024 May;67(3):315-325. 10.3340/jkns.2024.0032.
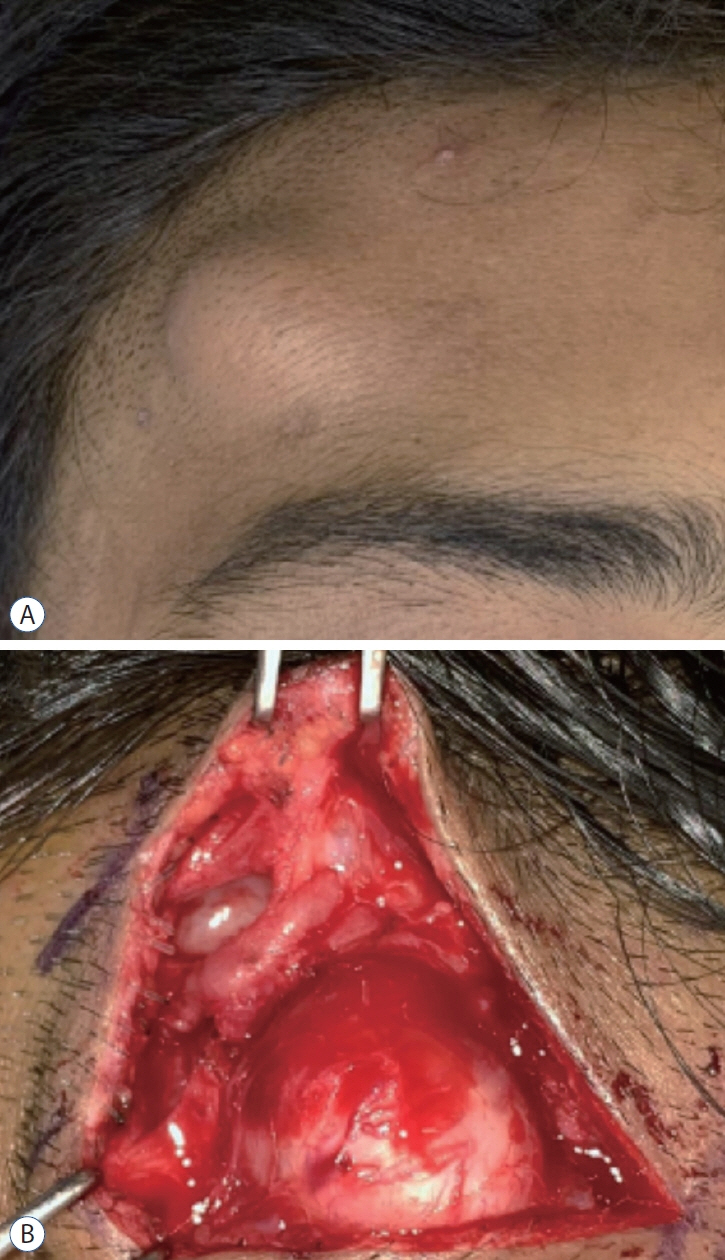
A Review of the Current State and Future Directions for Management of Scalp and Facial Vascular Malformations
- Affiliations
-
- 1Department of Neurosurgery, Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA
- 2Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA Department of Plastic & Oral Surgery, Boston Children’s Hospital, Harvard Medical School, Boston, MA, USA
- KMID: 2554869
- DOI: http://doi.org/10.3340/jkns.2024.0032
Abstract
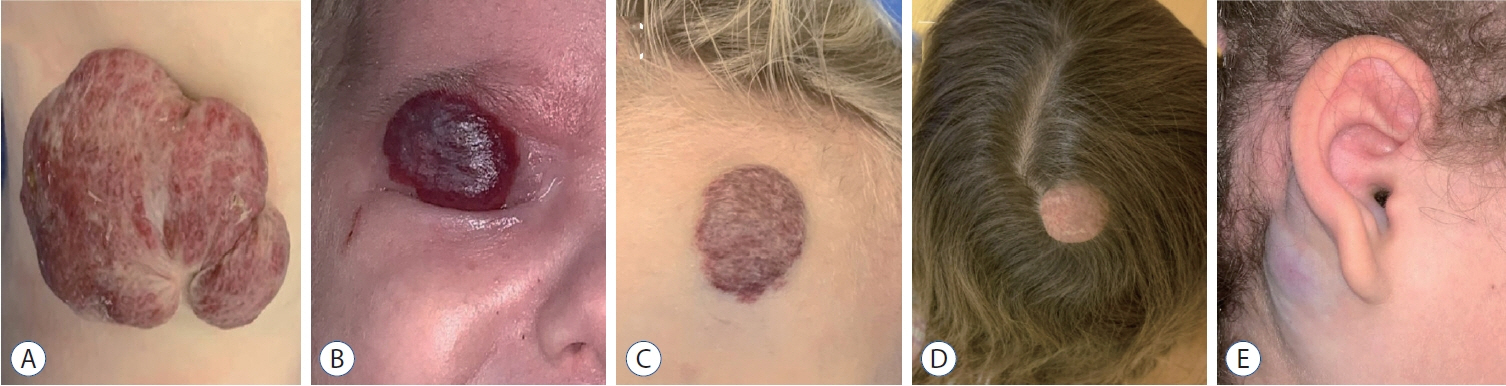
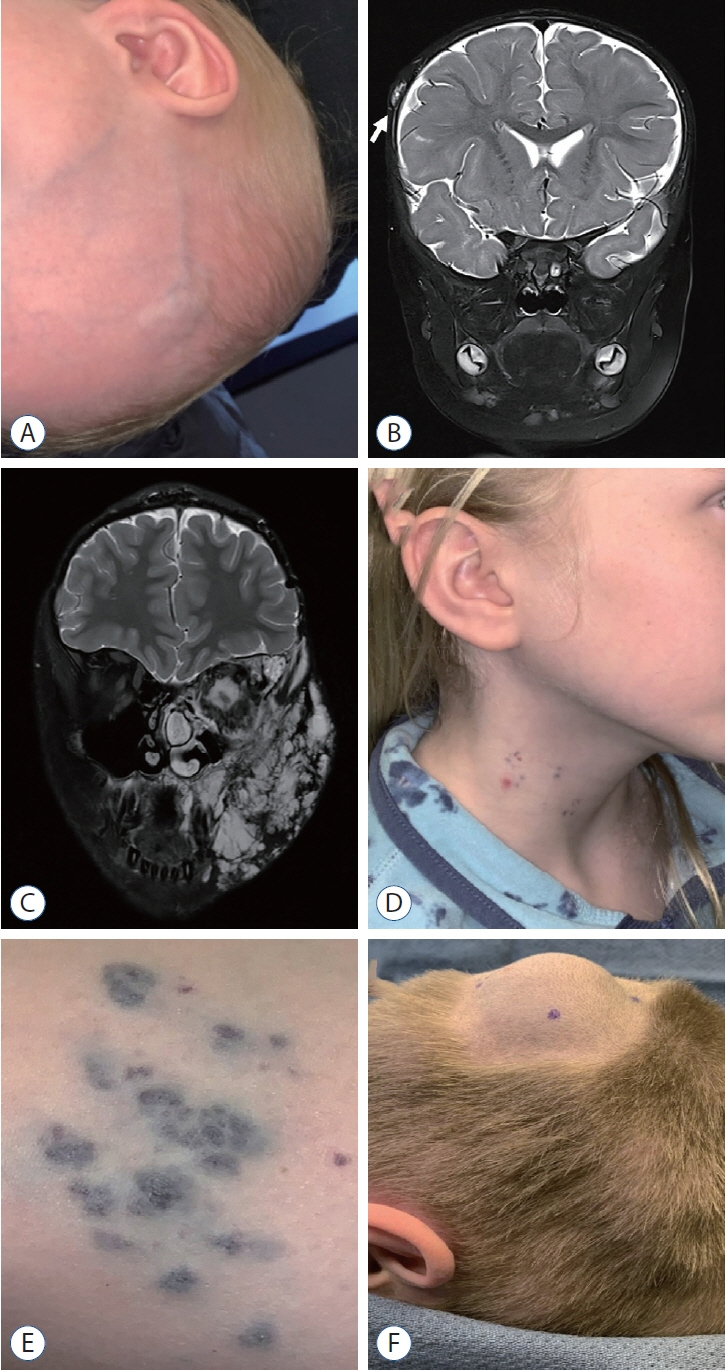
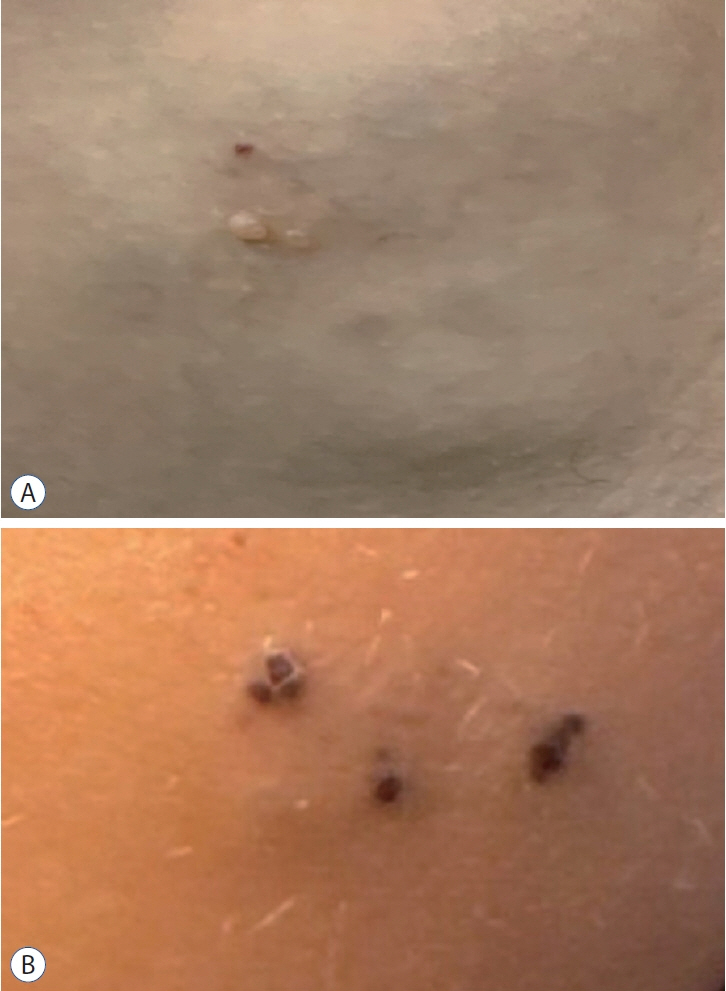
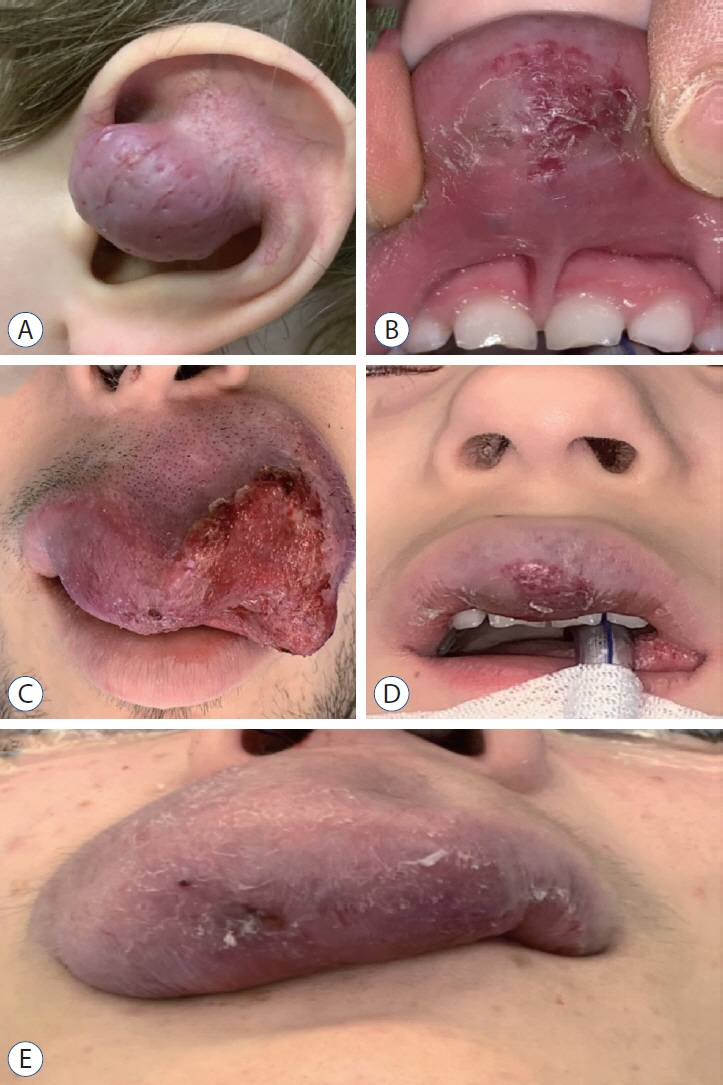
- Vascular malformations are structural abnormalities that are thought to result from errors in vasculogenesis and angiogenesis during embryogenesis. Vascular malformations of the scalp present unique management challenges due to aesthetic and functional implications. This review examines the pathophysiology, clinical presentation, and management techniques for six common types of vascular malformations of the face and scalp : infantile hemangioma, capillary malformations, venous malformations, lymphatic malformations, arteriovenous malformations, and arteriovenous fistulas. These lesions range from common to rare, and have very different natural histories and management paradigms. There has been increasing understanding of the molecular pathways that are altered in association with these vascular lesions and these molecular targets may represent novel strategies of treating lesions that have historically been approached from a structural perspective only.
Keyword
Figure
Reference
-
References
1. Ajiboye N, Chalouhi N, Starke RM, Zanaty M, Bell R. Cerebral arteriovenous malformations: evaluation and management. ScientificWorldJournal. 2014:649036. 2014.
Article2. Anderson KR, Schoch JJ, Lohse CM, Hand JL, Davis DM, Tollefson MM. Increasing incidence of infantile hemangiomas (IH) over the past 35 years: correlation with decreasing gestational age at birth and birth weight. J Am Acad Dermatol. 74:120–126. 2016.
Article3. Arnold R, Chaudry G. Diagnostic imaging of vascular anomalies. Clin Plast Surg. 38:21–29. 2011.4. Badejo L, Rockwood P. Traumatic arteriovenous fistula of the scalp. Case report. J Neurosurg. 66:773–774. 1987.5. Cenzato M, Boeris D, Piparo M, Fratianni A, Piano MA, Dones F, et al. Complications in AVM Surgery. In : Esposito G, Regli L, Cenzato M, Kaku Y, Tanaka M, Tsukahara T, editors. Trends in Cerebrovascular Surgery and Interventions. Cham: Springer;2021.6. Chamli A, Aggarwal P, Jamil RT, Litaiem N. Hemangioma in StatPearls. Treasure Island: StatPearls Publishing;2024.7. Cheng J, Liu B, Farjat AE, Routh J. National characteristics of lymphatic malformations in children: inpatient estimates and trends in the United States, 2000 to 2009. J Pediatr Hematol Oncol. 40:221–223. 2018.
Article8. Cheng YC, Chen HC, Wu CH, Wu YY, Sun MH, Chen WH, et al. Magnetic resonance angiography in the diagnosis of cerebral arteriovenous malformation and dural arteriovenous fistulas: comparison of timeresolved magnetic resonance angiography and three dimensional timeof-flight magnetic resonance angiography. Iran J Radiol. 13:e19814. 2016.
Article9. Cohen MM Jr. Vascular update: morphogenesis, tumors, malformations, and molecular dimensions. Am J Med Genet A. 140:2013–2038. 2006.10. Cox JA, Bartlett E, Lee EI. Vascular malformations: a review. Semin Plast Surg. 28:58–63. 2014.
Article11. Eifert S, Villavicencio JL, Kao TC, Taute BM, Rich NM. Prevalence of deep venous anomalies in congenital vascular malformations of venous predominance. J Vasc Surg. 31:462–471. 2000.
Article12. Fisher-Jeffes ND, Domingo Z, Madden M, de Villiers JC. Arteriovenous malformations of the scalp. Neurosurgery. 36:656–660. discussion 660. 1995.
Article13. Fishman SJ, Mulliken JB. Vascular anomalies. A primer for pediatricians. Pediatr Clin North Am. 45:1455–1477. 1998.14. Ghoddusi Johari H, Shahriarirad R, Erfani A, Darabi MH. High flow scalp arteriovenous malformation: a case report. World J Plast Surg. 9:228–231. 2020.
Article15. Greenberger S, Bischoff J. Pathogenesis of infantile haemangioma. Br J Dermatol. 169:12–19. 2013.
Article16. Gupta V, Chugh M, Walia BS, Vaishya S, Jha AN. Use of CT angiography for anatomic localization of arteriovenous malformation nidal components. AJNR Am J Neuroradiol. 29:1837–1840. 2008.
Article17. Haggstrom AN, Lammer EJ, Schneider RA, Marcucio R, Frieden IJ. Patterns of infantile hemangiomas: new clues to hemangioma pathogenesis and embryonic facial development. Pediatrics. 117:698–703. 2006.
Article18. Hasturk AE, Erten F, Ayata T. Giant non-traumatic arteriovenous malformation of the scalp. Asian J Neurosurg. 7:39–41. 2012.
Article19. Healy J, Balcazar JA, Rivera L, Ruas V. Rapid lymphatic malformation expansion: Imaging, association with asymptomatic Streptococcus infection, multidisciplinary management, and therapeutic approach. Radiol Case Rep. 18:3162–3168. 2023.
Article20. Hemangioma Investigator Group, Haggstrom AN, Drolet BA, Baselga E, Chamlin SL, Garzon MC, et al. Prospective study of infantile hemangiomas: demographic, prenatal, and perinatal characteristics. J Pediatr. 150:291–294. 2007.
Article21. Holmes LB. Chorionic villus sampling and hemangiomas. J Craniofac Surg. 20 Suppl 1:675–677. 2009.
Article22. Jinnin M, Medici D, Park L, Limaye N, Liu Y, Boscolo E, et al. Suppressed NFAT-dependent VEGFR1 expression and constitutive VEGFR2 signaling in infantile hemangioma. Nat Med. 14:1236–1246. 2008.
Article23. Khan IS, Kiehna EN, Satti KF, Ehtesham M, Ghiassi M, Singer RJ. Surgical management of large scalp infantile hemangiomas. Surg Neurol Int. 5:41. 2014.
Article24. Kilcline C, Frieden IJ. Infantile hemangiomas: how common are they? A systematic review of the medical literature. Pediatr Dermatol. 25:168–173. 2008.
Article25. Krowchuk DP, Frieden IJ, Mancini AJ, Darrow DH, Blei F, Greene AK, et al. Clinical practice guideline for the management of infantile hemangiomas. Pediatrics. 143:e20183475. 2019.
Article26. Kumar R, Sharma G, Sharma BS. Management of scalp arterio-venous malformation: case series and review of literature. Br J Neurosurg. 26:371–377. 2012.
Article27. Léauté-Labrèze C, Harper JI, Hoeger PH. Infantile haemangioma. Lancet. 390:85–94. 2017.
Article28. Lee SY, Loll EG, Hassan AS, Cheng M, Wang A, Farmer DL. Genetic and molecular determinants of lymphatic malformations: potential targets for therapy. J Dev Biol. 10:11. 2022.
Article29. Liu L, Li X, Zhao Q, Yang L, Jiang X. Pathogenesis of port-wine stains: directions for future therapies. Int J Mol Sci. 23:12139. 2022.
Article30. Malm M, Carlberg M. Port-wine stain--a surgical and psychological problem. Ann Plast Surg. 20:512–516. 1988.
Article31. Meyer JS, Hoffer FA, Barnes PD, Mulliken JB. Biological classification of soft-tissue vascular anomalies: MR correlation. AJR Am J Roentgenol. 157:559–564. 1991.
Article32. Mohamed WN, Abdullah NN, Muda AS. Scalp arteriovenous malformation : a case report. Malays J Med Sci. 15:55–57. 2008.33. Nagpal K, Ahmed K, Cuschieri R. Diagnosis and management of acute traumatic arteriovenous fistula. Int J Angiol. 17:214–216. 2008.
Article34. Nätynki M, Kangas J, Miinalainen I, Sormunen R, Pietilä R, Soblet J, et al. Common and specific effects of TIE2 mutations causing venous malformations. Hum Mol Genet. 24:6374–6389. 2015.
Article35. Nguyen V, Hochman M, Mihm MC Jr, Nelson JS, Tan W. The pathogenesis of port wine stain and Sturge Weber syndrome: complex interactions between genetic alterations and aberrant MAPK and PI3K activation. Int J Mol Sci. 20:2243. 2019.
Article36. Nosher JL, Murillo PG, Liszewski M, Gendel V, Gribbin CE. Vascular anomalies: a pictorial review of nomenclature, diagnosis and treatment. World J Radiol. 6:677–692. 2014.
Article37. Olivieri B, White CL, Restrepo R, McKeon B, Karakas SP, Lee EY. Lowflow vascular malformation pitfalls: from clinical examination to practical imaging evaluation--part 2, venous malformation mimickers. AJR Am J Roentgenol. 206:952–962. 2016.
Article38. Perkins JA, Manning SC, Tempero RM, Cunningham MJ, Edmonds JL Jr, Hoffer FA, et al. Lymphatic malformations: current cellular and clinical investigations. Otolaryngol Head Neck Surg. 142:789–794. 2010.
Article39. Richter GT, Friedman AB. Hemangiomas and vascular malformations: current theory and management. Int J Pediatr. 2012:645678. 2012.
Article40. Rodríguez Bandera AI, Sebaratnam DF, Wargon O, Wong LF. Infantile hemangioma. Part 1: epidemiology, pathogenesis, clinical presentation and assessment. J Am Acad Dermatol. 85:1379–1392. 2021.
Article41. Sakai K, Kitagawa T, Nakano Y, Saito T, Suzuki K, Kondo H, et al. Surgical resection of scalp arteriovenous fistulas after neurosurgical operation: a case report. Interdiscip Neurosurg. 27:101409. 2022.
Article42. Shi Y, Liu P, Liu Y, Quan K, Li P, Li Z, et al. Case report: endovascular treatment of two scalp arteriovenous malformation cases via direct percutaneous catheterization: a case series. Front Neurol. 13:945961. 2022.
Article43. Tamai N, Hashii Y, Osuga K, Chihara T, Morii E, Aozasa K, et al. Kaposiform hemangioendothelioma arising in the deltoid muscle without the Kasabach-Merritt phenomenon. Skeletal Radiol. 39:1043–1046. 2010.
Article44. Tan W, Wang J, Zhou F, Gao L, Yin R, Liu H, et al. Coexistence of Eph receptor B1 and ephrin B2 in port-wine stain endothelial progenitor cells contributes to clinicopathological vasculature dilatation. Br J Dermatol. 177:1601–1611. 2017.
Article45. Uebelhoer M, Nätynki M, Kangas J, Mendola A, Nguyen HL, Soblet J, et al. Venous malformation-causative TIE2 mutations mediate an AKTdependent decrease in PDGFB. Hum Mol Genet. 22:3438–3448. 2013.
Article46. Vikkula M, Boon LM, Mulliken JB. Molecular genetics of vascular malformations. Matrix Biol. 20:327–335. 2001.
Article47. Wali S, Alsolmi A, Babgi M, Alqurashi A, Alghamdi D, Bajunaid K, et al. Scalp arteriovenous malformation with dual bilateral arterial feeders: case report and review of literature. Interdiscip Neurosurg. 27:101431. 2022.
Article48. Wang X, Bove AM, Simone G, Ma B. Molecular bases of VEGFR-2-mediated physiological function and pathological role. Front Cell Dev Biol. 8:599281. 2020.
Article49. White CL, Olivieri B, Restrepo R, McKeon B, Karakas SP, Lee EY. Lowflow vascular malformation pitfalls: from clinical examination to practical imaging evaluation--part 1, lymphatic malformation mimickers. AJR Am J Roentgenol. 206:940–951. 2016.
Article50. Zhang X, Zhao X, Wu P, Zhao Z, Liu M, Wang YA. Prevalence and associated factors of anxiety and depression among patients with oromaxillofacial venous malformations. Ann Palliat Med. 10:8642–8650. 2021.
Article51. Zheng F, Augustus Pitts H, Goldbrunner R, Krischek B. Traumatic arteriovenous fistula of the scalp in the left temporoparietal region with intra- and extracranial blood supply. Case Rep Vasc Med. 2016:8671472. 2016.
Article52. Zhou Q, Zheng JW, Mai HM, Luo QF, Fan XD, Su LX, et al. Treatment guidelines of lymphatic malformations of the head and neck. Oral Oncol. 47:1105–1109. 2011.
Article53. Zyck S, Davidson CL, Sampath R. Arteriovenous Malformations in StatPearls. Treasure Island: StatPearls Publishing;2024.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Cerebral Vascular Malformations : Current and Future Perspectives
- A Case of Acquired Multiple Arteriovenous Malformations on the Scalp in the Patient of Liver Cirrhosis
- Advances in laser and stem cell treatment: current technologies, limitations, and future prospects
- Management of Asymptomatic Vascular Malformation
- Intervention of Vascular Diseases of the Spine