Adv Pediatr Surg.
2018 Dec;24(2):51-59. 10.13029/aps.2018.24.2.51.
Effect of Nutritional Support on Postoperative Growth Velocity of Neonates in Neonatal Intensive Care Unit
- Affiliations
-
- 1Department of Surgery, Chungnam National University College of Medicine and Hospital, Daejeon, Korea. jbprk@cnu.ac.kr
- KMID: 2429801
- DOI: http://doi.org/10.13029/aps.2018.24.2.51
Abstract
- PURPOSE
This study aimed to evaluate the relationship between nutritional support and growth velocity after abdominal surgery in neonates.
METHODS
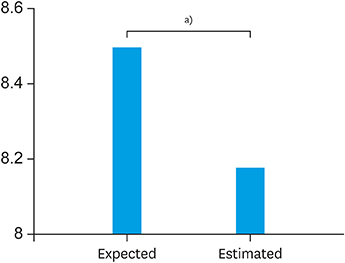
The electronic medical records of 45 neonates who underwent abdominal surgery in neonatal intensive care unit from 2012 to 2016 were collected to see how surgery and postoperative nutrition affect for the growth of neonate with abdominal surgery. The growth velocity was measured from the time of surgery to the time of discharge based on body weight.
RESULTS
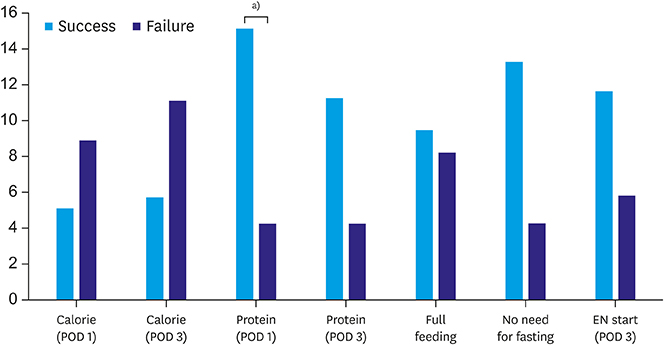
In neonates who achieve their protein requirement on the first day after surgery, the growth velocity was better than that in neonates who did not achieve their protein requirement on the first day after surgery (4.31 vs. 15.21; p=0.004). Based on the type of surgery, length of bowel resection and surgical complications, this study showed better growth velocity in neonates who had no surgical complications (5.34 vs. 12.74; p=0.775), reoperation (5.25 vs. 22.19, p=0.987), or bowel resection (6.79 vs. 9.95, p=0.302). However, there was no statistically significant difference among these factors.
CONCLUSION
We concluded in this study that adequate protein supplement from the first day of surgery could have a positive effect on the growth velocity of neonates who underwent abdominal surgery.
MeSH Terms
Figure
Reference
-
1. Pierro A. Metabolism and nutritional support in the surgical neonate. J Pediatr Surg. 2002; 37:811–822.
Article2. Andorsky DJ, Lund DP, Lillehei CW, Jaksic T, Dicanzio J, Richardson DS, et al. Nutritional and other postoperative management of neonates with short bowel syndrome correlates with clinical outcomes. J Pediatr. 2001; 139:27–33.
Article3. Teitelbaum DH, Coran AG. Perioperative nutritional support in pediatrics. Nutrition. 1998; 14:130–142.
Article4. Koletzko B, Goulet O, Hunt J, Krohn K, Shamir R, et al. Parenteral Nutrition Guidelines Working Group. 1. Guidelines on paediatric parenteral nutrition of the European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) and the European Society for Clinical Nutrition and Metabolism (ESPEN), supported by the European Society of Paediatric Research (ESPR). J Pediatr Gastroenterol Nutr. 2005; 41:Suppl 2. S1–S87.5. Little DC, Rescorla FJ, Grosfeld JL, West KW, Scherer LR, Engum SA. Long-term analysis of children with esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2003; 38:852–856.
Article6. Nicholson GT, Clabby ML, Kanter KR, Mahle WT. Caloric intake during the perioperative period and growth failure in infants with congenital heart disease. Pediatr Cardiol. 2013; 34:316–321.
Article7. Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF, et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics. 2005; 115:696–703.
Article8. Mitting R, Marino L, Macrae D, Shastri N, Meyer R, Pathan N. Nutritional status and clinical outcome in postterm neonates undergoing surgery for congenital heart disease. Pediatr Crit Care Med. 2015; 16:448–452.
Article9. McLeod G, Sherriff J. Preventing postnatal growth failure--the significance of feeding when the preterm infant is clinically stable. Early Hum Dev. 2007; 83:659–665.10. Owens JL, Musa N. Nutrition support after neonatal cardiac surgery. Nutr Clin Pract. 2009; 24:242–249.
Article11. Martin CR, Brown YF, Ehrenkranz RA, O'Shea TM, Allred EN, Belfort MB, et al. Nutritional practices and growth velocity in the first month of life in extremely premature infants. Pediatrics. 2009; 124:649–657.
Article12. Meurling S. The perioperative nutritional care of neonates and infants. Scand J Nutr. 2000; 44:8–11.
Article13. Cole CR, Hansen NI, Higgins RD, Ziegler TR, Stoll BJ. Eunice Kennedy Shriver NICHD Neonatal Research Network. Very low birth weight preterm infants with surgical short bowel syndrome: incidence, morbidity and mortality, and growth outcomes at 18 to 22 months. Pediatrics. 2008; 122:e573–e582.
Article14. Escribano J, Luque V, Ferre N, Mendez-Riera G, Koletzko B, Grote V, et al. Effect of protein intake and weight gain velocity on body fat mass at 6 months of age: the EU Childhood Obesity Programme. Int J Obes (Lond). 2012; 36:548–553.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nutritional Support in Premature Infants
- Nutrition Supply and Growth Post Nutrition Support Team Activity in Neonatal Intensive Care Unit
- Methicillin-resistant Staphylococcus aureus (MRSA) Infection in Neonates
- Amplitude Integrated Electroencephalography in the Neonatal Intensive Care Unit for Diagnosis of Neonatal Seizure
- Perceptions of fatherhood and confidence regarding neonatal care among fathers of high-risk neonates in South Korea: a descriptive study